Published online May 14, 2005. doi: 10.3748/wjg.v11.i18.2773
Revised: December 29, 2003
Accepted: February 17, 2004
Published online: May 14, 2005
AIM: Small intestinal bacterial overgrowth (SIBO) may contribute to the appearance of several gastrointestinal nonspecific symptoms. Acute diverticulitis is affected by some similar symptoms and bacterial colonic overgrowth. We assessed the prevalence of SIBO in acute uncomplicated diverticulitis and evaluated its influence on the clinical course of the disease.
METHODS: We studied 90 consecutive patients (39 males, 51 females, mean age 67.2 years, range 32-91 years). Sixty-one patients (67.78%) and 29 patients (32.22%) were affected by constipation-or diarrhea-prevalent diverticulitis respectively. All subjects were investigated by lactulose H2-breath test at the entry and at the end of treatment. We also studied a control group of 20 healthy subjects (13 males, 7 females, mean age 53 years, range 22-71 years).
RESULTS: Oro-cecal transit time (OCTT) was delayed in 67/90 patients (74.44%) (range 115-210 min, mean 120 min). Fifty-three of ninety patients (58.88%) showed SIBO, while OCTT was normal in 23/90 patients (25, 56%). In the control group, the mean OCTT was 88.2 min (range 75-135 min). The difference between diverticulitic patients and healthy subjects was statistically significant (P<0.01). OCTT was longer in constipation-prevalent disease than in diarrhea-prevalent disease [180.7 min (range 150-210 min) vs 121 min (range 75-180 min) (P<0.001)], but no difference in bacterial overgrowth was found between the two forms of diverticulitis.After treatment with rifaximin plus mesalazine for 10 d, followed by mesalazine alone for 8 wk, 70 patients (81.49%) were completely asymptomatic, while 16 patients (18.60%) showed only slight symptoms. Two patients (2.22%) had recurrence of diverticulitis, and two other patients (2.22%) were withdrawn from the study due to side-effects. Seventy-nine of eighty-six patients (91.86%) showed normal OCTT (range 75-105 min, mean 83 min), while OCTT was longer, but it was shorter in the remaining seven (8.14%) patients (range 105-115 min, mean of 110 min). SIBO was eradicated in all patients, while it persisted in one patient with recurrence of diverticulitis.
CONCLUSION: SIBO affects most of the patients with acute diverticulitis. SIBO may worsen the symptoms of patients and prolong the clinical course of the disease, as confirmed in the case of persistence of SIBO and diverticulitis recurrence. In this case, we can hypothesize that bacteria from small bowel may re-colonize in the colon and provoke recurrence of symptoms.
- Citation: Tursi A, Brandimarte G, Giorgetti GM, Elisei W. Assessment of small intestinal bacterial overgrowth in uncomplicated acute diverticulitis of the colon. World J Gastroenterol 2005; 11(18): 2773-2776
- URL: https://www.wjgnet.com/1007-9327/full/v11/i18/2773.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i18.2773
Diverticular disease of the colon is the most common disease affecting the large bowel in the Western world[1]. This disease is correlated with the aging process and a low-fiber diet and bears a considerable amount of morbidity[2]. The continuous aging process of the population also leads to an increase of this disease. To refer to an acquired deformity present in perhaps two-thirds of the elderly as a “disease” may be inaccurate, particularly as a large majority of those affected will remain entirely asymptomatic. Nonetheless, 20% of patients may manifest clinical illness[3].
The true incidence of colonic diverticulosis is difficult to measure, mainly because most patients are asymptomatic. The incidence clearly increases with age, varying from less than 10% in those under 40 years, to 50-66% of patients over 80 years[4-6]. Only a small proportion (5-10%) of patients who develop diverticulitis are younger than 50 years[7], and the course of the disease in these patients does not seem more aggressive than that in older patients[8].
It is commonly thought that multiple factors (anatomic features intrinsic to the colon, alterations in colonic wall with aging, dietary fiber, motor dysfunction, abnormal intraluminal pressure, and possible genetic influences) including altered motility of the large bowel play a great role in the genesis of colonic diverticula. Motility disorders of the gut are a predisposing factor in development of small intestinal bacterial overgrowth (SIBO)[9] that may contribute to the appearance of several gastrointestinal nonspecific symptoms, such as bloating, abdominal pain, flatulence and diarrhea[10]. Since acute diverticulitis is affected by some similar symptoms[3], and diverticulitis is affected by bacterial colonic overgrowth, the aim of this study was to assess the prevalence of SIBO in acute uncomplicated diverticulitis and its influence on the clinical course of the disease.
A prospective study was conducted on 90 consecutive patients (39 males, 51 females, mean age 67.2 years, range 32-91 years) with acute uncomplicated diverticulitis of the colon to assess the oro-cecal transit time (OCTT) and SIBO.
Diagnosis of diverticulitis, defined as inflammation and/or infection associated with diverticula of the colon[11], was performed by colonoscopy.
We assessed the following symptoms in all the enrolled patients: constipation, diarrhea, abdominal pain, rectal bleeding, and mucus passage with the stools. The intensity of the symptoms was quantified with a quantitative scale (0-10 according to increasing worsening of symptoms): 0: absence; 1-2: slight; 3-5: mild; 6-7: moderate; 8-10: severe.
In order to assess the prevalence of SIBO, all subjects were studied after an overnight fast for 24 h before the test. They were requested not to smoke on the morning of the test. End expiratory samples were collected before the patients drank the test solution (10 g of lactulose suspended in 100 mL of tap water) and at 15 min-intervals thereafter, for 240 min. Hydrogen concentrations in each collected sample were measured with a breath-hydrogen analyzer (EC60 gastrolyzer breath hydrogen monitor, Bedfont Scientific Ltd, Upchurch, Kent, UK). OCTT was defined as the time elapsing between lactulose ingestion and a sustained increase of 10 ppm or more of H2 excretion above the baseline value, which was about 75±15 min[12]. We also evaluated the presence of bacterial overgrowth, which was defined by the presence of a peak >20 ppm occurring >15 min before the colonic peak. The patients with an elevated fasting H2 combined with an early increase in H2 after lactulose ingestion were considered positive for bacterial overgrowth[13]. We compared the results obtained in a control group, comprising of 20 healthy subjects (13 males, 7 females, and mean age 53 years, range 22-71 years).
All patients were treated with rifaximin (Rifacol®, Formenti SpA, Milano, Italy) 800 mg/d plus mesalazine (Pentacol® 800, Sofar SpA, Trezzano Rosa [MI], Italy) 2.4 g/d for 10 d, followed by mesalazine 1.6 g/d for 8 wk.
Medical control visit and a new lactulose H2-breath test (H2-BT) were performed at the end of the 8th wk of treatment with mesalazine alone, and the presence of possible side-effects was evaluated. Moreover, the patients were invited to a control visit whenever they considered necessary.
Data were analyzed by χ2 test. P<0.05 was considered statistically significant.
Diverticulitis was localized in the overall colon of 10 patients (11.11%), in the transverse-descending-sigma of 13 patients (14.45%), in the left-sided colon of 12 patients (13.33%), in the descending colon-sigma of 45 cases (50%), in the sigma-rectum of 7 cases (7.78%) and in the rectum of 3 patients (3.33%). Sixty-one patients (67.78%) and 29 patients (32.22%) were affected by constipation-or diarrhea-prevalent diverticulitis respectively.
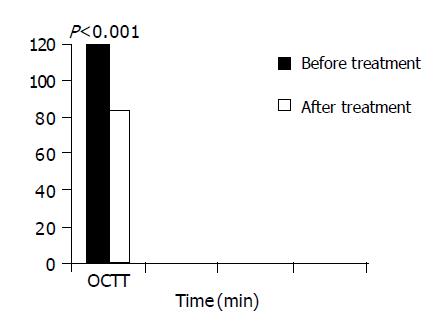
OCTT was delayed in 67/90 patients (74.44%), ranging from 115 to 210 min, averaged 120 min (Figure 1). Fifty-three of ninetypatients (58.88%) showed bacterial overgrowth, while OCTT was normal in 23/90 CD patients (25, 56%), ranging from 75 to 90 min averaged 82.5 min.
In the control group, the mean OCTT was 88.2 min, ranging from 75 to 135 min. The difference between patients with diverticulitis and healthy subjects was statistically significant (P<0.01).
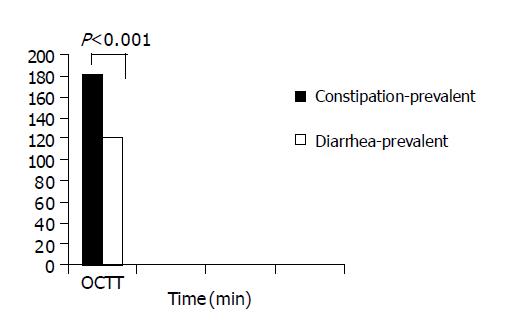
When we subdivided the studied population according to bowel movements (constipation-or diarrhea-prevalent colonic diverticulitis), we could note that OCTT was longer in constipation-prevalent disease than in diarrhea-prevalent disease. OCTT was 180.7 min (range 150-210 min), 121 min (range 75-180 min) in constipation- and diarrhea-prevalent colonic diverticulitis, respectively with a statistically significant difference (P<0.001, Figure 2).
Interestingly, we did not find any difference in bacterial overgrowth between patients. In fact, 26/53 (49.05%) patients and 27/53 (50.95%) patients with SIBO were affected by constipation-prevalent and diarrhea- prevalent colonic diverticulitis, respectively.
Seventy patients (per-protocol: 81.49% [CI: 67-94%]; on intention-to-treat: 77.78% [CI: 60-85%]) were completely asymptomatic after the 8th wk of treatment with mesalazine alone (overall symptomatic score: 0), while 16 patients (per-protocol: 18.60%; on intention-to-treat: 17.77%) showed only mild symptoms (overall symptomatic score: 44). Two patients (2.22%) had recurrence of diverticulitis (abdominal pain, constipation, and fever) after 4 and 6 wk of treatment with mesalazine alone, and two other patients (2.22%) showed severe side-effects (severe diarrhea [more than 8 bowel movements/day]), and they were withdrawn from the study. The overall score of patients decreased from 1439 to 44 (P<0.001).
Lactulose H2-BT was re-evaluated at the end of the 8th wk of treatment with mesalazine alone. Seventy-nine of eighty-six (91.86%) patients showed normal OCTT, ranging from 75 to 105 min, averaged 83 min, while OCTT was longer but it was shorter in the remaining seven (8.14%) patients, ranging from 105 to 115 min, averaged 110 min. SIBO was eradicated in all patients. In contrast, a new lactulose H2-BT showed persistence of SIBO in one patient with recurrence of diverticulitis.
Abnormal intraluminal pressure and disordered colonic motility have been implicated as pathogenetic factors in diverticulosis. In particular, alteration of colonic motility has been described as the pathophysiological mechanism in diverticular disease. It has been reported that colonic motility is influenced by the aging process, as shown by the decrease of high-amplitude propagated contraction frequency with the age, whereas segmental contractile activity increases[14].
This study showed clearly that most of the patients with acute diverticulitis showed a high prevalence of SIBO. The mechanisms underlying the genesis of SIBO in uncomplicated diverticulitis of the colon may be as follows. The first involved mechanism may be the fecal stasis. In fact, the muscle thickening observed in affected bowel segments was thought to be obstructive, and to contribute to the delayed transit of feces[15]. Studies with intracolonic displacement tools suggested that an accentuation of segmentary motor activity (as observed in diverticular disease) could abolish oro-aboral progression of contents[16], thereby facilitating retropulsion and drying of the semiliquid fecal matter. These findings have led to the second mechanism causing SIBO that may be the colonic bacterial overgrowth. Changes in intestinal microflorae may be one of the putative mechanisms responsible for colonic inflammation, and could be the key point in the development of symptoms in acute uncomplicated diverticulitis. Acute diverticulitis is a condition characterized by abnormal bacterial colonic overgrowth. This last condition, associated with the reverse peristalsis affecting the colon in diverticular disease, may then favor a small bowel colonization by colonic bacterial florae, provoking SIBO. This hypothesis was confirmed by this study as most patients with acute diverticulitis of the colon showed delayed OCTT (74.44%) and SIBO (58.88%).
The reason why SIBO evaluation is important in acute uncomplicated diverticulitis of the colon is that SIBO is a small bowel disease that has never been investigated in patients with acute uncomplicated diverticulitis, but it may play a role in the genesis of the symptoms experienced by these patients. SIBO is characterized by nonspecific GI complaints, ranging from mild symptoms such as bloating, abdominal pain and flatulence to a severe malabsorption syndrome with diarrhea, steatorrhea and weight loss, and small intestinal mucosal lesions in some cases[10]. Bacteria are responsible for intraluminal sugar fermentation with the production of a great amount of H2 and CH4 (causing bloating, abdominal pain and flatulence). Furthermore, they could cause bile salt deconjugation and dehydroxylation of fatty acids with consequent fat malabsorption and impaired ileal resorption of bile acids, which have irritative and cathartic effects on colonic mucosa. The final consequence of these events is the development of diarrhea, abdominal pain and mucus passage with stools. These symptoms are indistinguishable from those of acute uncomplicated diverticulitis, and may then worsen patient symptoms. Moreover, it may prolong the clinical course of the disease. This last hypothesis has been confirmed by the patients with diverticulitis recurrence and persistence of SIBO. In this case we can hypothesize that bacteria from the small bowel may re-colonize in the colon and provoke recurrence of symptoms.
Fortunately, the main treatment for SIBO and acute uncomplicated diverticulitis is the same. In fact, rifaximin has been effectively used both in the treatment of diverticular disease[17] and in the treatment of SIBO[18]. On the other hand, delayed colonic motility persisted despite resolution of acute episodes. This colonic alteration may then persist as a risk factor for SIBO recurrence in patients with colonic diverticulitis. Persistence or recurrence of symptoms often indistinguishable from those of diverticulitis, may lead to unnecessary diagnostic examinations to exclude recurrence of diverticulitis. However, a correct exclusion of SIBO by lactulose breath test may contribute to the correct diagnosis and exclusion of diverticulitis recurrence in most of the cases.
Science Editor Li WZ Language Editor Elsevier HK
| 1. | Jun S, Stollman N. Epidemiology of diverticular disease. Best Pract Res Clin Gastroenterol. 2002;16:529-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 81] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Almy TP, Howell DA. Medical progress. Diverticular disease of the colon. N Engl J Med. 1980;302:324-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 176] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Tursi A. Acute diverticulitis of the colon--current medical therapeutic management. Expert Opin Pharmacother. 2004;5:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2:450-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 538] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterol. 1975;4:53-69. [PubMed] |
| 6. | Painter NS, Burkitt DP. Diverticular disease of the colon, a 20th century problem. Clin Gastroenterol. 1975;4:3-21. [PubMed] |
| 7. | Eusebio EB, Eisenberg MM. Natural history of diverticular disease of the colon in young patients. Am J Surg. 1973;125:308-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 61] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Biondo S, Parés D, Martí Ragué J, Kreisler E, Fraccalvieri D, Jaurrieta E. Acute colonic diverticulitis in patients under 50 years of age. Br J Surg. 2002;89:1137-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Husebye E. Gastrointestinal motility disorders and bacterial overgrowth. J Intern Med. 1995;237:419-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 60] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Haboubi NY, Lee GS, Montgomery RD. Duodenal mucosal morphometry of elderly patients with small intestinal bacterial overgrowth: response to antibiotic treatment. Age Ageing. 1991;20:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110-3121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 252] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Hirikawa M, Iida M, Korogi N, Fujishima M. Hydrogen breath test assessment of oro-cecal transit time: comparison with barium meal study. Am J Gastroenterol. 1988;83:1361-1363. |
| 13. | Kerlin P, Wong L. Breath hydrogen testing in bacterial overgrowth of the small intestine. Gastroenterology. 1988;95:982-988. [PubMed] |
| 14. | Di Lorenzo C, Flores AF, Hyman PE. Age-related changes in colon motility. J Pediatr. 1995;127:593-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Raguse T, Bubenzer J. Functional and morphological studies on diverticulosis of the large bowel. Chir Forum Exp Klin Forsch. 1979;3:138-143. [PubMed] |
| 16. | García-Olmo D, Sanchez PC. Patterns of colonic motility as recorded by a sham fecaloma reveal differences among patients with idiopathic chronic constipation. Dis Colon Rectum. 1998;41:480-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Papi C, Ciaco A, Koch M, Capurso L. Efficacy of rifaximin in the treatment of symptomatic diverticular disease of the colon. A multicentre double-blind placebo-controlled trial. Aliment Pharmacol Ther. 1995;9:33-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Tursi A, Brandimarte G, Giorgetti G. High prevalence of small intestinal bacterial overgrowth in celiac patients with persistence of gastrointestinal symptoms after gluten withdrawal. Am J Gastroenterol. 2003;98:839-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 129] [Article Influence: 5.9] [Reference Citation Analysis (0)] |