Published online May 7, 2005. doi: 10.3748/wjg.v11.i17.2681
Revised: September 22, 2004
Accepted: December 1, 2004
Published online: May 7, 2005
Pseudomembranous colitis (PMC) usually manifests as fever and diarrhea in hospitalized patients treated with systemic antibiotics. We described a case of PMC with intestinal obstruction but without diarrhea. A 60-year-old man was hospitalized for chemotherapy for the treatment of Burkitt lymphoma of the stomach. The patient became febrile and complained of crampy abdominal pain during the post-chemotherapy nadir. Plain abdominal radiography showed some intestinal gas and niveau. Because stool cytotoxin assay for clostridium difficile was positive and colon fiberscopic examination showed a pseudomembrane at the left side of the colon, and a diagnosis of PMC was made. Treatment with intracolonic vancomycin administration by colonoscopy and nasoileus tube was successful. Physicians should take into account the possibility of bowel obstruction due to PMC occurring in patients undergoing chemotherapy and perform emergency colonoscopy examination of suspected cases.
- Citation: Nomura K, Fukumoto K, Shimizu D, Okuda T, Yoshida N, Kamitsuji Y, Matsumoto Y, Konishi H, Ueda Y, Horiike S, Okanoue T, Taniwaki M. Pseudomembranous colitis presenting as acute colonic obstruction without diarrhea in a patient with gastric Burkitt lymphoma. World J Gastroenterol 2005; 11(17): 2681-2683
- URL: https://www.wjgnet.com/1007-9327/full/v11/i17/2681.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i17.2681
Pseudomembranous colitis (PMC) typically manifests as fever, crampy abdominal pain and diarrhea in hospitalized patients being treated with systemic antibiotics[1]. Some patients complain of a sensation of incomplete evacuation, nausea, and occasional vomiting[2-6]. The treatment of PMC requires discontinuation of therapy with the offending antibiotics and administration of oral vancomycin (VCM) or metronidazole.
This report concerns a patient with non-Hodgkin’s lymphoma (NHL) who complained of crampy pain during chemotherapy. He was diagnosed as having acute bowel obstruction provoked by PMC. To the best of our knowledge, this is a very rare case of PMC presenting as ileus without diarrhea during treatment for NHL. Intracolonic VCM administration by colonoscopy and nasoileus tube proved effective.
A 60-year-old man was admitted to our hospital in May 2004 for consolidation chemotherapy for the treatment of gastric Burkitt lymphoma, having t(8;14) confirmed by tissue-FISH method[7]. He was first treated with three courses of CHOP (cyclophosphamide, adriamycin, vincristine, and predonisolone) therapy, but since he proved to be refractory for this regimen, ESHAP (etoposide, methylprednisolone, high-dose cytarabine, and cisplatin) was introduced as salvage therapy and complete remission was obtained[8]. Hyper-CVAD (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone)/methotrexate (MTX) therapy was used for consolidation therapy[9]. After the first administration of hyper-CVAD chemotherapy, however, the patient became febrile. Sulbactam/cefoperazone and clindamycin hydrochloride were then administered and the symptoms improved, but this was followed by diarrhea. A diagnosis of PMC based on positivity for Clostridium difficile led to the discontinuation of antibiotics and subsequent administration of metronidazole was effective for diarrhea.
During the second course of high-dose MTX therapy, the patient became febrile again and experienced diarrhea on d 9. Administration of cefozopran hydrochloride, meropenem trihydrate, and amikacin sulfate resulted in rapid improvement of the diarrhea.
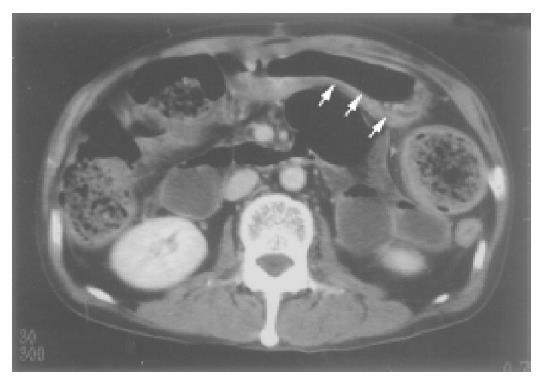
Crampy pain without diarrhea started on d 18 after the second hyper-CVAD therapy. On the same day, leukocytes started to recover from the nadir. Computed tomography showed swelling of the wall of the left side of the transverse colon (Figure 1) while plain abdominal radiography indicated the presence of some intestinal gas and niveau (Figure 2).
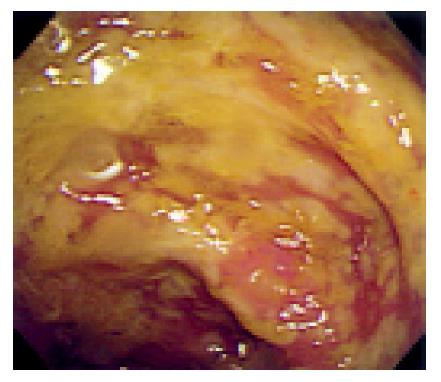
Emergency colonoscopic examination showed patchy, yellow-gray plaques at the left half of the transverse colon, which strongly suggested PMC (Figure 3).
Intracolonic VCM administration (1g) was started at that time[10,11]. An enzyme immunoassay performed on the same day detected C. difficile toxin A in the patient’s stool. Introduction of both metronidazole and VCM thr-ough a nasoileus tube resulted in improvement of these symptoms.
The NHL patient described here presented with ileus during chemotherapy. CT examination suggests that the obstruction of the lumen was caused by swelling of the wall of the intestine. Colonoscopy led to the detection of pseudomembranes. PMC without diarrhea is rare, being reported in patients with acute abdominal pain due to fulminant pancolitis, toxic megacolon, and perforation[12,13]. However, in our case, colitis was limited at the left half of the transverse colon. There are neither signs of toxic megacolon nor perforation. In our case, the increase in WBCs possibly provoked severe and rapid inflammation of the colon wall, resulting in bowel obstruction, because ileus occurred at the time WBCs started to increase rapidly after the nadir.
Successful treatment of our patient was achieved with decompression and intracolonic VCM administration by means of colonoscopy. However, since continuous drug delivery to the colon is difficult, we inserted a nasoileus tube for the administration of metronidazole and VCM, proving to be effective for our patient.
In conclusion, physicians should take into account the possibility of bowel obstruction due to PMC occurring in patients undergoing chemotherapy for NHL, especially during recovery period from the nadir.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Cleary RK. Clostridium difficile-associated diarrhea and colitis: clinical manifestations, diagnosis, and treatment. Dis Colon Rectum. 1998;41:1435-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Sheikh RA, Yasmeen S, Pauly MP, Trudeau WL. Pseudomembranous colitis without diarrhea presenting clinically as acute intestinal pseudo-obstruction. J Gastroenterol. 2001;36:629-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Elinav E, Planer D, Gatt ME. Prolonged ileus as a sole manifestation of pseudomembranous enterocolitis. Int J Colorectal Dis. 2004;19:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Binkovitz LA, Allen E, Bloom D, Long F, Hammond S, Buonomo C, Donnelly LF. Atypical presentation of Clostridium difficile colitis in patients with cystic fibrosis. AJR Am J Roentgenol. 1999;172:517-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Triadafilopoulos G, Hallstone AE. Acute abdomen as the first presentation of pseudomembranous colitis. Gastroenterology. 1991;101:685-691. [PubMed] |
| 6. | Boland GW, Lee MJ, Cats A, Mueller PR. Pseudomembranous colitis: diagnostic sensitivity of the abdominal plain radiograph. Clin Radiol. 1994;49:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Nomura K, Sekoguchi S, Ueda K, Nakao M, Akano Y, Fujita Y, Yamashita Y, Horiike S, Nishida K, Nakamura S. Differentiation of follicular from mucosa-associated lymphoid tissue lymphoma by detection of t(14; 18) on single-cell preparations and paraffin-embedded sections. Genes Chromosomes Cancer. 2002;33:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Velasquez WS, McLaughlin P, Tucker S, Hagemeister FB, Swan F, Rodriguez MA, Romaguera J, Rubenstein E, Cabanillas F. ESHAP--an effective chemotherapy regimen in refractory and relapsing lymphoma: a 4-year follow-up study. J Clin Oncol. 1994;12:1169-1176. [PubMed] |
| 9. | Kantarjian HM, O'Brien S, Smith TL, Cortes J, Giles FJ, Beran M, Pierce S, Huh Y, Andreeff M, Koller C. Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol. 2000;18:547-561. [PubMed] |
| 10. | Shetler K, Nieuwenhuis R, Wren SM, Triadafilopoulos G. Decompressive colonoscopy with intracolonic vancomycin administration for the treatment of severe pseudomembranous colitis. Surg Endosc. 2001;15:653-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Pasic M, Jost R, Carrel T, Von Segesser L, Turina M. Intracolonic vancomycin for pseudomembranous colitis. N Engl J Med. 1993;329:583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Sheth SG, LaMont JT. Toxic megacolon. Lancet. 1998;351:509-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 94] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Gerding DN, Johnson S, Peterson LR, Mulligan ME, Silva J. Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995;16:459-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 303] [Article Influence: 10.1] [Reference Citation Analysis (0)] |