Published online Apr 14, 2005. doi: 10.3748/wjg.v11.i14.2184
Revised: September 8, 2004
Accepted: November 19, 2004
Published online: April 14, 2005
AIM: We aimed to observe the expression of extracellular matrix (ECM) and cellular adhesion molecules (CAM) in cirrhotic liver tissues after hepatitis C virus (HCV) infection.
METHODS: Twelve patients with post HCV inflammatory liver cirrhosis were selected to evaluate their liver function and other virological, pathological parameters. Then three specimens of cirrhotic patients whose health assessment results and laboratory data were similar and three normal liver specimens explanted from liver grafts prepared for liver transplantation were chosen for investigating gene expression of ECM and CAM using cDNA expression array.
RESULTS: The cDNA array assay revealed 36.7% (36/96) of genes with changes, in which 26.3% (26/96) was up-regulated and 10.1% (10/96) was down-regulated. Integrin (ITGA), collagen (COL), ADAMTS were identified as the characteristic changes of ECM and CAM gene expression levels. ITGA were demonstrated β1 and β2 sub-section changed in liver cirrhosis.
CONCLUSION: ECM and CAM play an important role in the progression of liver cirrhosis after HCV infection. The capital mechanism is related to the inflammatory cells infiltration, the activation and transformation of ECM producing cells and the imbalance between production and elimination of ECM.
- Citation: Xu X, Li YM, Ji H, Hou CZ, Cheng YB, Ma FP. Changes of ECM and CAM gene expression profile in the cirrhotic liver after HCV infection: Analysis by cDNA expression array. World J Gastroenterol 2005; 11(14): 2184-2187
- URL: https://www.wjgnet.com/1007-9327/full/v11/i14/2184.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i14.2184
Hepatitis C virus (HCV) infection is the major cause of liver cirrhosis according to recent studies. Olga[1] reported that about 20-25% patients with HCV infection would become liver fibrosis or/and cirrhosis. Some studies reported that HCV infection would develop to chronic liver diseases for about 18.4 years later, liver cirrhosis after 20.6 years, and liver cancer after 28.3 years, respectively. The research of the mechanisms of development of liver cirrhosis after HCV infection and prevention of cirrhosis are very important health issues[2]. In this study, we emphasized on the ECM and cellular adhesion molecules (CAM) gene expression levels that changed during liver cirrhosis after HCV infection through DNA array. We can conclude that the alterations in the expression levels of these genes might be relevant to the progression of liver cirrhosis.
It is accepted that the key reason for liver fibrosis/cirrhosis is the maladjustment of production and elimination of ECM and CAM. Unfortunately, the functions and changes of ECM and CAM genes in cirrhotic liver tissues after HCV infection are not clear.
Normal liver specimens in control group were taken from liver grafts preparing for liver transplantation. According to the medical protocol, specimens from cirrhotic livers were collected from 12 patients with post HCV inflammatory liver cirrhosis undergoing devascularization of cardiac veins in the second hospital of Xi’an Jiaotong University from 2004 January-July. After the preoperative evaluation of liver function and judgment of apparent liver changes during operation, liver specimens were quickly obtained and conserved in liquid nitrogen. The GEArray Q Series Human Extracellular Matrix and Adhesion Molecules Gene Array and related kits were purchased from SuperArray Bioscience Corporation, which contains 96 genes encoding proteins important for the attachment of cells to their surroundings. The array includes various types of cell adhesion molecules as well as extracellular matrix (ECM) proteins, proteases and their inhibitors. These proteins play key roles in mediating cell-cell, cell-tissue and cell-extract ECM interactions and are involved in the normal processes of growth, division, differentiation and apoptosis. And these genes were important in many liver diseases, especially liver cirrhosis. Through a simple side-by-side hybridization using experimental samples and the array and reagent provided in the kit, we determine the expression profile of these matrix and adhesion molecules in our selected patients.
The three patients’ liver tissues, which were No. 1-3 in Table 1, were chosen according to the gross shape, sex and age and Child-Pugh classification in the operation.
| Sex (F/M) | Age (yr) | TBIL (mmol/L) | ALB (g/L) | Encephalopathy | Ascites | Nutritional state | Child class | Gross shape1 | |
| 1 | M | 40 | 17.7 | 36.0 | No | No | Fine | A | Great |
| 2 | F | 45 | 17.4 | 36.9 | No | No | Fine | A | Great |
| 3 | F | 49 | 19.8 | 41.6 | No | Small | Fine | B | Great |
| 4 | M | 41 | 52.3 | 31.2 | No | Mess | Weak | C | Diffuse |
| 5 | M | 37 | 39.1 | 40.6 | No | Small | Fine | B | Great |
| 6 | F | 41 | 26.1 | 43.9 | No | No | Fine | A | Less |
| 7 | M | 47 | 10.2 | 40.1 | No | No | Fine | A | Diffuse |
| 8 | M | 55 | 22.5 | 33.8 | No | Small | Fine | B | Less |
| 9 | F | 38 | 19.6 | 28.4 | No | Small | Fine | C | Less |
| 10 | F | 40 | 7.6 | 45.3 | No | Small | Fine | A | Diffuse |
| 11 | M | 59 | 70.3 | 35 | No | Small | Fine | C | Great |
| 12 | M | 48 | 46.5 | 45.4 | No | Small | Weak | B | Great |
Based on the diagnostic resolution of Fifth National Inflammatory and Parasitic Diseases in 1995, the clinical data and pathologic sections were assured by three more surgeons and pathologists.
mRNA isolation and assessing Tissue samples of liver in TRIzol were homogenized using a power homogenizer. The samples were homogenized by adding chloroform, then centrifuged at 4 °C, and the RNA was made to remain in the aqueous phase. The RNA was precipitated from the aqueous phase by mixing with isopropyl alcohol, and the RNA pellet was washed once with 75% ethanol. The RNA was air-dried, and redissolved in RNase-free water. The absorbance was read in a spectrophotometer at 260 and 280 nm to determine the concentration and purity of RNA, and the ratio of A260 to A280 values were calculated to measure the RNA purity.
Probe synthesis and hybridization RNA was reverse-transcribed by gene-specific primers with biotin-16-dUTP. The cDNA probes were denatured and hybridized to ECM and CAM gene-specific cDNA fragments spotted on the membranes. The membranes were then washed with Wash Solution and blocked with GEA blocking solution.
Chemiluminescent detection The hybridized biotinylated probes were detected by chemiluminescent method using the alkaline phosphatase substrate, CDP-Star. The results were analyzed using GEArray Analyzer software. Each membrane comprised 96 marker genes, negative controls (pUC18 DNA and blanks) and housekeeping genes, including β-actin, GAPDH, cyclophilin A and ribosomal protein L13a. All relative expression levels of different genes were estimated by comparing their signal intensity with that of internal control.
Data analysis Using GEArray Analyzer software for background subtraction and data normalization, each GEArrayTM Q Series membranes are spotted with negative controls and housekeeping genes. All raw signal intensities were corrected for background by subtracting the minimum value to avoid the appearance of negative numbers. All signal intensities were normalized to that of a housekeeping gene.
As shown in Table 2, the 3 of 12 in-hospital patients with post-HCV inflammatory liver cirrhosis were selected according to their sex, age, course and child score, and their liver were screened for further detection. During operation, the specimens were taken from at least two different regions on the liver surfaces and conserved appropriately for cDNA array assay.
| Patient | Sex | Age (yr) | Progress (yr) | Child score | Liver screen and appearance | |
| Test group | 1 | F | 45 | 11 | A | Greater tubercle liver cirrhosis portal vein: 1.1±0.1 cm in diameter |
| 2 | F | 49 | 10 | B | ||
| 3 | M | 40 | 4 | A | ||
| Control group | 1 | F | 35 | - | A | Normal |
| 2 | F | 46 | - | A | ||
| 3 | M | 31 | - | A |
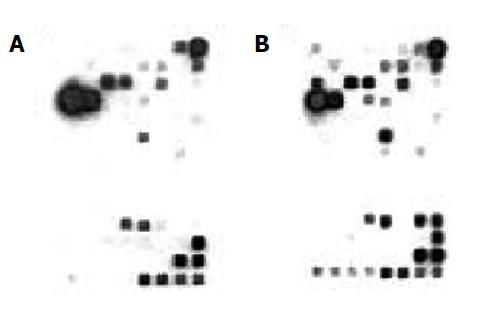
We carried out mRNA array assay in order to investigate the comprehensive changes in the gene expression of post HCV inflammatory liver cirrhosis. The mRNA array system, which can detect changes in the expression of 96 human genes, was used for this study. Two independent experiments: normal and cirrhotic, were conducted to clarify the role of HCV cirrhosis core protein. The results of the mRNA array are shown in Figure 1 (A) Exp.1 = normal liver/control group and (B) Exp.2 = cirrhotic liver/test group. 36.7% (36/99) genes were found to be changed in mRNA gene array assay, 26.3% was up-regulated as judged by the criterion of core signals intensity ration ≥3, and 10.1% was down-regulated as judged by the criterion of core signals intensity ration ≤0.3.
As Table 3 shows the up-regulated gene expression levels in cirrhotic and normal liver tissues, COL, ITGA, ADAMTS and MMP represent higher volume production of fibrosis, intense cells adhesion, disequilibrium between ECM and ICM. Especially, COL1A1 is a rare component in normal liver tissue, which is 5.947×10-4, but it increases 12.22 times to 7.266×10-3. At the same time, COL3, COL4 did not increase gene expression level. Some subunits of integrin families, ITGAα10, ITGA 7, ITGA L, ITGA M, ITGA V, ITGA X, and ITGAβ2 altered their gene expression levels. The metalloproteinase, ADAMTS and MMP, gene expression levels were 3 to 90-fold in liver cirrhosis than normal.
| Gene name | Exp.1 | Exp.2 | Exp.2-Exp.1 | Exp.2/Exp.1 |
| CAM | ||||
| ITGAa10 | 3.531E-4 | 5.751E-3 | 5.398E-3 | 1.63E+01 |
| ITGA 7 | -0.000E-1 | 1.722E-5 | 1.722E-5 | N/A |
| ITGA L | 2.639E-3 | 7.921E-3 | 5.282E-3 | 3.00E+00 |
| ITGA M | 6.690E-4 | 7.043E-3 | 6.374E-3 | 1.05E+01 |
| ITGA V | 2.416E-4 | 2.635E-3 | 2.393E-3 | 1.09E+01 |
| ITGA X | -0.000E-1 | 2.497E-3 | 2.497E-3 | N/A |
| ITGAb2 | -0.000E-1 | 1.877E-3 | 1.877E-3 | N/A |
| ICAM1 | 4.296E-2 | 3.695E-1 | 3.265E-1 | 8.60E+00 |
| CD44 | 3.847E-3 | 9.706E-2 | 9.322E-2 | 2.52E+01 |
| CTNN1 | 1.728E-1 | 5.052E-1 | 3.324E-1 | 2.92E+00 |
| CST3 | 1.057E-1 | 3.735E-1 | 2.678E-1 | 3.53E+00 |
| ECM | ||||
| CAV1 | 5.017E-4 | 5.699E-3 | 5.198E-3 | 1.14E+01 |
| COL1A1 | 5.947E-4 | 7.266E-3 | 6.672E-3 | 1.22E+01 |
| LAMb1 | 1.301E-4 | 8.969E-2 | 8.956E-2 | 6.90E+02 |
| LAMC1 | -0.000E-1 | 3.444E-5 | 3.444E-5 | N/A |
| SPP1 | 2.973E-4 | 7.781E-1 | 7.778E-1 | 2.62E+03 |
| THBS1 | 1.639E-2 | 7.918E-1 | 7.754E-1 | 4.83E+01 |
| Metalloproteinases | ||||
| ADAMTS1 | -0.000E-1 | 1.860E-1 | 1.860E-1 | N/A |
| ADAMTS 8 | 7.433E-5 | 7.404E-4 | 6.661E-4 | 9.96E+00 |
| MMP15 | 1.858E-5 | 6.888E-5 | 5.029E-5 | 3.71E+00 |
| MMP 16 | -0.000E-1 | 3.788E-4 | 3.788E-4 | N/A |
| MMP 17 | -0.000E-1 | 6.888E-5 | 6.888E-5 | N/A |
| MMP 2 | 3.717E-5 | 2.411E-4 | 2.039E-4 | 6.49E+00 |
| MMP 8 | -0.000E-1 | 4.305E-4 | 4.305E-4 | N/A |
Table 4 shows the down-regulated genes in cirrhotic liver. Combined with the up-regulated genes from the same family of Table 3, the different expression levels may suggest different functions of integration, promotion or inhibition.
| Gene name | Exp.1 | Exp.2 | Exp.2-Exp.1 | Exp.2/Exp.1 |
| CAM | ||||
| Integrin | ||||
| ITGA3 | 3.529E-1 | 9.885E-2 | -2.541E-1 | 2.80E-01 |
| ITGA5 | 1.388E-2 | 4.546E-3 | -9.336E-3 | 3.28E-01 |
| ITGA8 | 1.067E-2 | 2.927E-4 | -1.037E-2 | 2.74E-02 |
| Cadherin | 2.604E-1 | 5.863E-2 | -2.018E-1 | 2.25E-01 |
| CTNND2 | ||||
| ECM protein: | 6.948E-2 | 3.960E-3 | -6.552E-2 | 5.70E-02 |
| SPARC | ||||
| Serine proteinases | ||||
| CTSG | 1.468E-2 | 8.954E-4 | -1.379E-2 | 6.10E-02 |
| TMPRSS4 | 1.191E-2 | -0.000E-1 | -1.191E-2 | 0.00E+00 |
| HPSE | 2.531E-1 | 3.306E-2 | -2.201E-1 | 1.31E-01 |
| Tissue inhibitor of metalloproteinases | ||||
| TIMP2 | 2.895E-2 | -0.000E-1 | -2.895E-2 | 0.00E+00 |
| TIMP 3 | 6.168E-2 | 3.960E-4 | -6.128E-2 | 6.42E-03 |
Shimizu[3] reported that HCV infection is the “most common” cause of liver fibrosis. The production of ECM is increased in liver tissue in which HSCs are activated.
ECM in the liver is composed of protein and glycosaminoglycan. Biologically, ECM protein is divided into two types: constructive and adhesive ECM[4]. The stability of ECM and ICM is attributed with the production and elimination of ECM in normal liver, but this balance would be disturbed if the components produced more, or eliminated less[5,6].
The major part of constructive ECM is collagen, which is about 5-8 mg/1 g in normal liver tissue and the ratio of collagen1/collagen3 is less than 1. In cirrhotic liver, however, the content of collagen protein is 4 to 7-fold than that of normal liver. At the same time, and the ratio of collagen1/collagen3 is larger than 1. Our results showed that the content of collagen was 12.22-fold in cirrhotic liver than that of control group. The ratio changes of collagens in the cirrhotic liver may be the key to liver cirrhosis progression. Some researchers reported that COL2 was the most abundant collagen components in the newly formed fibrotic tissues and then COL1 increased to be the main components in mature fibrotic tissues. It is implied that the change of collagen types, concentration and the disturbance of balance between producing and elimination of collagen may produce a marked effect in the developmental period of liver cirrhosis[7]. In this study, the gene expression levels of COL1 and COL2 were up-regulated and that of TIMP2 and TIMP3 were down-regulated. It suggests the contribution of TNFβ1 to the development of cirrhosis because these changes were similar to the recent researches that TNFβ1 could promote the formation of ECM and inhibit its elimination[8].
Laminin (LAM) is the main type of adhesive ECM and performs many important biological functions. Acting as the important factor of basement membrane (BM), LAM is associated with the BM formation in liver microvascular tissue during cirrhosis. It also adjusts the pressure between Disse sinus and hepatic sinusoids. This phenomenon may be related to the by-pass blood reserve in cirrhotic liver. Our study shows that LAMB1 and LAMC1 were increased 10-fold in cirrhotic liver tissue.
CAM is believed to perform multiple functions in liver cirrhosis. This is clarified by the following factors: ITGA, cadherin, CD44 ICAM, and selectin, which promote the activation and homing of T, B lymph cells, infiltration of leukocytes and deposition of collagens and concentration of HA and so on. Integrin family has been classified to be over 20 kinds of dimers and 14 kinds of αsubunits and 9βsubunits. This specific membrane protein can transmit the signals of ECM and intracellular matrix (ICM), and act as an acceptor of ECM on membrane[9].
ADAMTS is one kind of medial enzyme that can help cells secrete different kinds of matrix enzymes, such as TNFα, TNFβ and so on. In our research, 7 of 19 genes were identified as core response of ADAMTS and MMPs family in HCV cirrhotic liver tissues. The up-regulated genes of MMPs were believed to be induced by down-regulated TIMP, which controlled the activity of MMPs[10].
Except for integrin family, CAM also includes the following members: cadherin, CD44 family, ICAM, immunoglobulin superfamily and selectin. We found that the expression level of cadherin was responsibly down-regulated, which indicated the cellular polarity and microstructure damages. Recently reports show that cadherin plays an important role in regulating cell adhesion and linkage formation.
Some cytokines secreted by platelets, macrophageal cells in inflammatory tissues, perform different modulatory effects on the development of liver cirrhosis[11]. It is also noteworthy that cytokines can alter the gene expression of ECM and CAM in cirrhotic liver tissue after HCV infection by producing activated oxidative components[12].
Science Editor Li WZ Language Editor Elsevier HK
| 1. | Olga OZ, Nikolai DY. Invasive and non-invasive monitoring of hepatitis C virus-induced liver fibrosis: alternatives or complements? Curr Pharm Biotechnol. 2003;4:195-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Smith MW, Yue ZN, Korth MJ, Do HA, Boix L, Fausto N, Bruix J, Carithers RL, Katze MG. Hepatitis C virus and liver disease: global transcriptional profiling and identification of potential markers. Hepatology. 2003;38:1458-1467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Shimizu I. Impact of oestrogens on the progression of liver disease. Liver Int. 2003;23:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 143] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 4. | Raines EW. The extracellular matrix can regulate vascular cell migration, proliferation, and survival: relationships to vascular disease. Int J Exp Pathol. 2000;81:173-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 242] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 5. | Kozłowska J, Łoch T, Jabłońska J, Cianciara J. Biochemical markers of fibrosis in chronic hepatitis and liver cirrhosis of viral origin. Przegl Epidemiol. 2001;55:451-458. [PubMed] |
| 6. | Sobel RA. The extracellular matrix in multiple sclerosis: an update. Braz J Med Biol Res. 2001;34:603-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Shimizu I. Antifibrogenic therapies in chronic HCV infection. Curr Drug Targets Infect Disord. 2001;1:227-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Calabrese F, Valente M, Giacometti C, Pettenazzo E, Benvegnu L, Alberti A, Gatta A, Pontisso P. Parenchymal transforming growth factor beta-1: its type II receptor and Smad signaling pathway correlate with inflammation and fibrosis in chronic liver disease of viral etiology. J Gastroenterol Hepatol. 2003;18:1302-1308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Quondamatteo F, Kempkensteffen C, Miosge N, Sonnenberg A, Herken R. Ultrastructural localization of integrin subunits alpha3 and alpha6 in capillarized sinusoids of the human cirrhotic liver. Histol Histopathol. 2004;19:799-806. [PubMed] |
| 10. | Oda T, Jung YO, Kim HS, Cai X, López-Guisa JM, Ikeda Y, Eddy AA. PAI-1 deficiency attenuates the fibrogenic response to ureteral obstruction. Kidney Int. 2001;60:587-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 222] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 11. | Bedossa P, Paradis V. Approaches for treatment of liver fibrosis in chronic hepatitis C. Clin Liver Dis. 2003;7:195-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Powell EE, Edwards-Smith CJ, Hay JL, Clouston AD, Crawford DH, Shorthouse C, Purdie DM, Jonsson JR. Host genetic factors influence disease progression in chronic hepatitis C. Hepatology. 2000;31:828-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 305] [Article Influence: 12.2] [Reference Citation Analysis (0)] |