Published online Apr 14, 2005. doi: 10.3748/wjg.v11.i14.2142
Revised: September 22, 2004
Accepted: November 29, 2004
Published online: April 14, 2005
AIM: To retrospectively establish the diagnostic criteria of gallstone ileus on CT, and to prospectively apply these criteria to determine the diagnostic accuracy of CT to confirm or exclude gallstone ileus in patients who presented with acute small bowel obstruction (SBO). Another purpose was to ascertain whether the size of ectopic gallstones would affect treatment strategy.
METHODS: Fourteen CT scans in cases of proved gallstone ileus were evaluated retrospectively by two radiologists for the presence or absence of previously reported CT findings to establish the diagnostic criteria. These criteria were applied in a prospective contrast enhanced CT study of 165 patients with acute SBO, which included those 14 cases of gallstone ileus. The hard copy images of 165 CT studies were reviewed by a different group of two radiologists but without previous knowledge of the patient’s final diagnosis. All CT data were further analyzed to determine the diagnostic accuracy of gallstone ileus when using CT in prospective evaluation of acute SBO. The size of ectopic gallstone on CT was correlated with the clinical course.
RESULTS: The diagnostic criteria of gallstone ileus on CT were established retrospectively, which included: (1) SBO; (2) ectopic gallstone; either rim-calcified or total-calcified; (3) abnormal gall bladder with complete air collection, presence of air-fluid level, or fluid accumulation with irregular wall. Prospectively, CT confirmed the diagnosis in 13 cases of gallstone ileus with these three criteria. Only one false negative case could be identified. The remaining 151 patients are true negative cases and no false positive case could be disclosed. The overall sensitivity, specificity and accuracy of CT in diagnosing gallstone ileus were 93%, 100%; and 99%, respectively. Surgical exploration was performed in 13 patients of gallstone ileus with ectopic stones sized larger than 3 cm. One patient recovered uneventfully following conservative treatment with an ectopic stone sized 2 cm in the long axis.
CONCLUSION: Contrast enhanced CT imaging offered crucial evidence not only for the diagnosis of gallstone ileus but also for decision making in management strategy.
- Citation: Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS, Tyan YS, Hwang JI, Liou CH, Chang WC, Chen CY. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol 2005; 11(14): 2142-2147
- URL: https://www.wjgnet.com/1007-9327/full/v11/i14/2142.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i14.2142
Gallstone ileus resulted from recurrent attacks of cholecystitis and erosion of gallstone through adjacent duodenal wall into small intestine, which may lead to bowel obstruction. It accounts for 1-2% per cent of mechanical small bowel obstruction (SBO). In geriatric population, the incidence could be as high as 25%[1].
Gallstone ileus presented a challenging surgical dilemma clinically. Misdiagnosis is common and it also carries a significant rate of complications with a mortality rate ranging from 12% to 27% in most series reported[2]. High morbidity and mortality rate could be attributed to delayed diagnosis, senile patient, and coexisting concomitant medical disease. Early diagnosis is therefore pivotal to improve morbidity, mortality and post-operative complications.
Traditionally, plain abdominal radiography remained a mainstay for the assessment of SBO. However, the sensitivity of plain film varies from 40% to 70% in diagnosing gallstone ileus[3,4].
Recent literatures have shown that ultrasonography (US) was more helpful in diagnosing gallstone ileus than plain abdominal radiography[5,6]. But the sensitivity of detection rate in a large-scale US study was 74% at best[6].
Most case reports on CT had also proven its value for diagnosing gallstone ileus[7-11] but still lack prospective study in large patient population thus far to verify the diagnostic accuracy if clinician chooses CT to evaluate acute SBO.
The aim of the present article is to retrospectively establish CT diagnostic criteria of gallstone ileus, and to prospectively apply these criteria to determine the diagnostic accuracy of CT to confirm or exclude gallstone ileus in patients who presented with acute SBO.
Advantages and limitations of different CT protocols were also assessed from our findings and previous reports to verify whether oral or IV contrast administration post any helpful in patients with suspected gallstone ileus and other etiology of SBO.
Another aim of this work is to determine whether the size of ectopic gallstones would affect treatment strategy.
From our radiology database between November 1994 and 2002, 14 patients of gallstone ileus were identified for inclusion in this study. There were nine women and five men with mean age of 74 years (range 38-94 years). Ten patients were older than 70 years. All patients were documented by surgery (n = 13) or by classic CT criteria with spontaneous recovery after conservative treatment (n = 1). The CT images were evaluated retrospectively with two board-certified radiologists (CYY, CHL) for published or unpublished CT findings to establish the diagnostic criteria.
During the same period, 151 consecutive patients with other etiology of acute SBO were included in this study. There were 82 males and 69 females with mean age of 63 years (range 20-89 years). Acute SBO was suspected by the clinical symptoms and plain abdominal radiography. The final diagnosis was established by surgery (n = 128), clinical follow up (n = 21), and US-guide aspiration and drainage (n = 2). The etiology of clinical follow up patients included adhesive band (n = 19) and intramural hematoma (n = 2). Adhesive band was inferred from CT when no mass or other abnormality was noted around the site of obstruction. Intramural hematoma of small intestine following blunt abdominal injury was also inferred from CT on the basis of demonstration of transition zone with a focal homogeneous wall thickening and higher attenuation than the adjacent normal bowel wall. The clinical symptom of all these patients showed complete resolution within 2 wk.
All patients accepted CT examination and the hardware included either a conventional CT (Somatom Hi-Q, Simens Medical System, Germany) or a spiral CT (Somatom plus-4, Siemens Medical System, Germany). Oral contrast material was administered with 2% iodinated water-soluble contrast medium at least 1 h before scanning if patient could tolerate. One hundred milliliters of 60% iodinated nonionic or ionic IV contrast was delivered by a power injector or by hand injection at a rate of 2 cm3/s if patient showed no history of contrast allergy or renal function impairment. No rectal contrast was given simultaneously. Scanning was performed in the craniocaudal direction, beginning at the dome of the right hemidiaphragm to the symphysis pubis.
In gallstone ileus patients group, only one patient did not accept IV contrast due to renal function impairment. Oral contrast was given to six patients, who presented with intestinal obstruction; however, clinical symptom still could tolerate oral contrast.
In the rest of SBO patients group, 151 patients accepted IV contrast and only 32 patients received oral contrast administration.
CT images were obtained at portal venous phase (70 s after contrast injection). A beam collimation of 8 mm, pitch 1.5, and reconstructed at 8 mm intervals were used in spiral CT. Conventional CT used 10 mm slice thickness and 10 mm table incremental scan.
The hard copy images of 165 CT studies were reviewed retrospectively by a different group of two board-certified radiologists (YST, JIH), whom were blinded to the final diagnosis. All CT data were further analyzed to determine the diagnostic accuracy of gallstone ileus when using CT in prospective evaluation acute SBO.
The etiology of SBO in our 165 patients is described in Table 1. Detailed plain film, CT findings, and clinical data of these 14 patients of gallstone ileus are listed in Table 2. Duration of symptom onset prior to admission in patients with gallstone ileus varied from 1 to 5 d. Time interval between admission and CT was less than 24 h. The time lag between CT and operation was also less than 24 h. Plain abdominal radiography was taken routinely on admission and only five patients matched the full criteria of Rigler’s triad (5/14 = 36%). In the individual criterion analysis, pneumobilia presented on plain film of five cases (5/14 = 36%) and on CT of seven cases (7/14 = 50%). Mechanical SBO was suggested by plain film (n = 10, 10/14 = 71%) and by clinical symptoms (n = 4). These latter four patients demonstrated massive fluid accumulation within bowel lumen, which made invaluable of plain film. Ectopic gallstone could be diagnosed using plain film on six patients (6/14 = 43%).
| Cause of SBO | Number of patients |
| Gallstone ileus | 14 |
| Phytobezoar | 7 |
| Intussusception | 13 |
| Inguinal hernia | 10 |
| Spigelian hernia | 7 |
| Obturator hernia | 3 |
| Transmesosigmoid hernia | 1 |
| Appendicitis | 6 |
| Perforated appendicitis | 4 |
| Periappendiceal abscess | 2 (21) |
| Diverticulitis with rupture | 2 |
| Ischemic bowel disease | 5 |
| Eosinophilic enteritis | 1 |
| Intramural hematoma | 3 (22) |
| Adhesive band | 57 (192) |
| Malignant lymphoma | 3 |
| Adenocarcinoma of jejunum | 1 |
| Adenocarcinoma of ileum | 1 |
| Adenocarcinoma of ileo-cecal valve | 9 |
| Adenocarcinoma of ascending colon | 17 |
| Adenocarcinoma of hepatic flexure colon | 2 |
| Case | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
| Plain film | ||||||||||||||
| Pneumobilia | - | - | + | - | + | - | + | - | + | + | - | - | - | |
| - Gas in gall bladder fossa | - | - | - | - | - | + | - | - | - | - | - | - | - | + |
| Small bowel obstruction | - | - | + | + | + | + | + | + | + | + | + | + | - | - |
| Ectopic gallstone | + | - | - | + | + | + | + | - | - | + | - | - | - | - |
| CT | ||||||||||||||
| Pneumobilia | - | - | + | + | + | - | + | - | + | + | - | - | + | - |
| Gall bladder content | Air | Fluid | Air | Air | Air-fluid | Air | Air-fluid | Air | Air | Air | Air | Air | Fluid | Air-fluid |
| Small bowel obstruction | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Ectopic gallstone | TC | RC | RC | TC | TC | RC | TC | RC | RC | TC | RC | RC | RC | RC |
| Other CT findings | ||||||||||||||
| Cholecysto-duodenal fistula | - | - | - | + | - | + | - | - | - | + | - | - | - | - |
| Thickened duodenum (>1cm) | + | + | + | - | - | - | - | - | - | - | - | - | - | - |
| Ascites | + | + | + | + | + | + | - | + | - | + | - | - | - | - |
| Thickened small intestine (>1cm) | - | + | - | - | - | + | - | - | - | - | - | - | - | - |
| Clinical data | ||||||||||||||
| Symptom onset duration (d) | 1 | 1 | 1 | 2 | 3 | 3 | 3 | 4 | 5 | 5 | 5 | 5 | 5 | 5 |
| WBC(×109/L) upon admission | 24.70 | 24.50 | 21.70 | 16.50 | 13.90 | 13.50 | 12.40 | 10.25 | 10.90 | 5.30 | 7.30 | 6.60 | 9.50 | 8.30 |
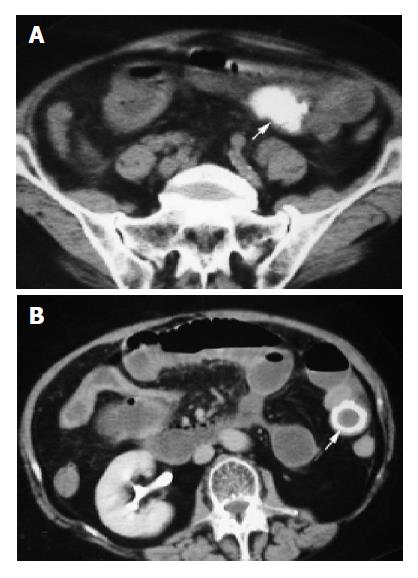
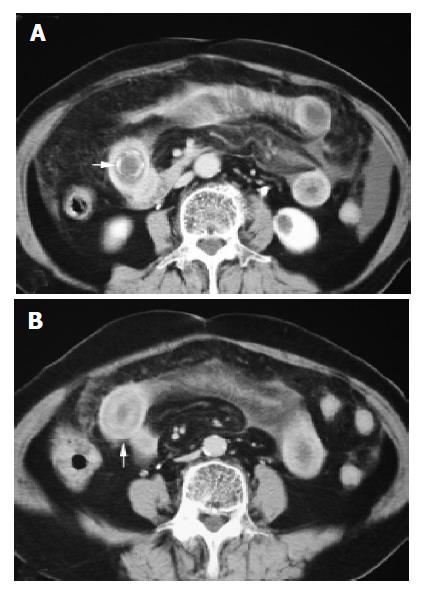
The diagnostic criteria of gallstone ileus on CT were established retrospectively, which included: (1) SBO (n = 14); (2) ectopic gallstone; either rim-calcified (n = 9) (Figure 1A) or total-calcified (n = 5) (Figure 1B); (3) abnormal gall bladder with complete air collection (n = 9) (Figure 2A), presence of air-fluid level (n = 3) (Figure 2B), or fluid accumulation with irregular wall (n = 2) (Figure 2C).
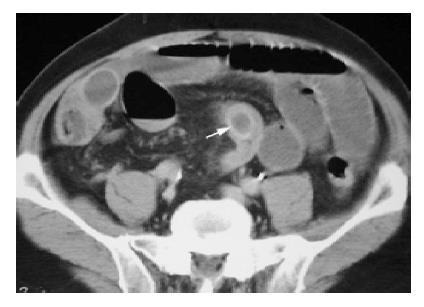
All three criteria were utilized in a prospective evaluation of 165 patients with acute SBO. Gallstone ileus was confirmed pre-operatively with CT in 13 cases. Only one false negative case could be identified and it showed less calcification in the rim-calcified ectopic gallstone, which rendered poor differentiation from the enhanced small bowel wall with similar density and without clear space between each other (Figure 3).
No false positive case could be disclosed, which means positive predictive value is 100%. The remaining 151 patients are true negative cases. The overall sensitivity, specificity and accuracy of CT to diagnosing gallstone ileus was 93% (13/14), 100% (151/151); and 99% (164/165), respectively.
Two low sensitivity CT findings also could be identified in our study, which included cholecystoduodenal fistula (n = 3) and wall thickening (>1 cm) of the second portion duodenum (n = 3) (Figure 4). The latter three patients had symptom onset duration that lasted less than 1 d with leukocytosis over 20.00×109/L and ascites (Table 2).
Another low sensitivity finding on CT showed segmental edematous wall thickening (>1 cm) over ileum, just prior to the transition zone (n = 2) (Figures 5A and 5B). During operation, peal formation and edematous change could be identified. However, there was a lack of evidence of perforation or ischemia in these patients, who recovered uneventfully following surgery.
The size of ectopic gallstone by CT imaging showed to be larger than 3 cm in 13 cases. All of them accepted surgical intervention. Only one patient achieved spontaneous recovery following conservative treatment, which presented with an ovoid ectopic gallstone sized 2 cm in the long axis (Figure 6).
Clinical manifestation and plain abdominal radiographic findings of gallstone ileus are rarely specific, often similar to other causes of mechanical SBO, and more than one-third of patients presented no history of biliary symptoms[12]. Several case reports have shown accuracy of CT in the diagnosis of gallstone ileus[7-11]. However, larger patient population is needed to establish the diagnostic CT criteria and to verify the diagnostic accuracy if clinician chooses CT to evaluate acute SBO. Based on our study, the diagnostic CT criteria include: (1) SBO; (2) ectopic gallstone; either rim-calcified or total-calcified; (3) abnormal gall bladder with complete air collection, presence of air-fluid level, or fluid accumulation with irregular wall. Our study also demonstrated that contrast enhanced CT have high sensitivity (93%), specificity (100%), and accuracy (99%) to diagnose gallstone ileus in patients who presented with acute SBO.
Gallstone ileus takes an insidious course, presented symptoms of intermittent intestinal obstruction. Duration of symptoms prior to admission was varied from 6 h to 22 d[2,7]. The longest in our series is 5 d. Duration from admission to operation ranged from 5 h to 14 d and overall mortality rate was 19%[2,7,12-14]. According to these reports, delayed diagnosis plus concomitant geriatric disease could lead to severe complications, including fatality. All of our patients had CT study within 24 h upon admission, which made early diagnosis possible. Therefore, we were not able to observe classical tumbling phenomenon in any of our cases. All of our patients showed full recovery and the key issue here is to be able to obtain prompt diagnosis with CT imaging and early surgical intervention.
The classic Rigler’s triad for diagnosis of gallstone ileus on plain abdominal radiography was reported to be present about 30-35% cases[1,15]. In our study, only 36% cases (5/14) presented full criteria.
When single criterion was used for evaluation, pneumobilia could be detected on plain film in five patients (5/14 = 36%) and on CT in seven patients (7/14 = 50%). The rare incidence may be secondary to persistent obstruction of cystic duct even with cholecystoduodenal fistula presence to decompress the gallbladder.
Air collection within the gall bladder can be easily misdiagnosed and misinterpreted as colon gas by plain film alone. However, CT could easily detect complete air collection, air-fluid level, or fluid accumulation with irregular wall within the diseased gall bladder in all fourteen cases of our study.
Only six cases with ectopic gallstones could be identified by plain film but CT picked up 13 cases. Possible etiology for this limitation of plain film may be related that ectopic gallstone superimposed with bony structures or fluid-filled bowel, obscured by obesity, or lack of identifiable calcification.
Recent works suggested that CT has high sensitivity and accuracy for pre-operative evaluation of patient with suspected intestinal obstruction or acute abdomen[16-19]. The promptness and capability of contrast-enhanced CT to reveal the cause of SBO and acute abdomen makes it essential for emergency use[20].
When dealing with CT, the first issue is whether oral water-soluble contrast is needed in SBO evaluation? In CT evaluation of high grade obstruction, oral contrast administration should be prohibited on account of: (1) vomiting always precluding excessive fluid intake; (2) suffocation likely while patient changes position from sitting to supine if excessive fluid accumulation within the stomach; (3) existing intestinal fluid offered natural negative contrast effect to differentiate the location and wall thickness of the transition zone[19]. However, if patient posed with partial intestinal obstruction or intermittent high grade obstruction as in cases of gallstone ileus, oral contrast could be used to further dilate the proximal small intestine, which allows better evaluation of the transition zone[3].
Rim-or totally calcified ectopic gallstone could be easily detected by CT without oral contrast administration. But based on our study (n = 6) and previous reports[10], oral contrast administration may not interfere with the diagnosis of ectopic gallstone because: (1) most oral contrast did not reach the transition zone due to obstruction; (2) diluted oral contrast consists of relatively low density as compared to the high density of rim or totally calcified stone.
Non-enhanced (free IV) CT can serve as a diagnostic imaging tool to prompt identification of ectopic gallstone despite the presence of any degree of calcification, based on our study (n = 1) and previous reports[8-11]. It also offers two advantages: (1) no risk of contrast allergy, and (2) routine application to all patient population, including those with renal function impairment.
Contrast-enhanced CT, on the other hand, is more difficult to identify rim-calcified stone than total calcified ones. Rim-calcified component would be easily missed as normal bowel wall appears without clear space in-between to separate each other. In addition, less calcification in ectopic rim-calcified gallstone could be neglected when equal enhancement is achieved in the small bowel wall[7,21,22]. Only one false negative case could be identified in our study and the remaining 13 could be diagnosed well before operation.
Intravenous contrast material is valuable for improved detection of edema, inflammation, and ischemia of the small intestine[19]. Therefore contrast enhanced CT may help to establish alternate diagnosis of SBO and to predict the presence of complications. In our study, edematous wall thickening of the small intestine prior to transition zone could be clearly identified by CT in two cases and it was proved to be transient ischemic change from distended bowel loops.
Another two low sensitivity CT findings, cholecystoduodenal fistula and wall thickening of duodenum second portion, also could be clearly identified by contrast-enhanced CT. These two findings existed concomitantly in a previous report[7] but our result did not. Previous report did not define the criteria of thickening duodenum or offer any graphic evidence for this finding. Wall thickening of the duodenum second portion in our study correlated well with symptom onset duration less than 24 h, leukocytosis over 20.00×109/L, and ascites, which were suggestive of acute inflammatory process in progress. However, the presence of cholecystoduodenal fistula did not parallel with the acute inflammatory status in our study and it may well be due to pressure generated by incomplete evacuation of the gallbladder contents and/or high-grade SBO persistent but we can only hypothesize this for lack of direct evidence.
Accurate diagnosis of the location and etiology of small-bowel obstruction is essential for therapeutic planning[20]. Precision surgical incision for gallstone ileus with open or laparoscopic enterolithotomy need detailed anatomical correlation[23,24]. Previous report suggested primary surgical intervention is mandatory for all cases with gallstone ileus[13]. But one patient in our series demonstrated spontaneous recovery and his ectopic gallstone size was 2 cm in long axis, which others also witnessed[11]. It is the second case in the literature to validate conservative treatment was also effective in the management of gallstone ileus[11]. Then, we proposed that when prospective CT estimation of ectopic gallstone sized less than 2 cm in size, patients should receive conservative treatment with constant monitoring of vital signs until complete clinical recuperation. If conservative measures affected resolution of gallstone ileus accordingly, better prognosis could be achieved especially in elderly and debilitating patients.
In conclusion, contrast enhanced CT evaluation of acute SBO offers prompt and rapid diagnosis of gallstone ileus before operation. CT also has the capability to estimate the size of ectopic gallstone, which rendering decision making in management strategy.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Hudspeth AS, McGuirt WF. Gallstone ileus. A continuing surgical problem. Arch Surg. 1970;100:668-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Clavien PA, Richon J, Burgan S, Rohner A. Gallstone ileus. Br J Surg. 1990;77:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 247] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 3. | Maglinte DD, Reyes BL, Harmon BH, Kelvin FM, Turner WW, Hage JE, Ng AC, Chua GT, Gage SN. Reliability and role of plain film radiography and CT in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol. 1996;167:1451-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 151] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | Shrake PD, Rex DK, Lappas JC, Maglinte DD. Radiographic evaluation of suspected small bowel obstruction. Am J Gastroenterol. 1991;86:175-178. [PubMed] |
| 5. | Lasson A, Lorén I, Nilsson A, Nirhov N, Nilsson P. Ultrasonography in gallstone ileus: a diagnostic challenge. Eur J Surg. 1995;161:259-263. [PubMed] |
| 6. | Ripollés T, Miguel-Dasit A, Errando J, Morote V, Gómez-Abril SA, Richart J. Gallstone ileus: increased diagnostic sensitivity by combining plain film and ultrasound. Abdom Imaging. 2001;26:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Swift SE, Spencer JA. Gallstone ileus: CT findings. Clin Radiol. 1998;53:451-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Grumbach K, Levine MS, Wexler JA. Gallstone ileus diagnosed by computed tomography. J Comput Assist Tomogr. 1986;10:146-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Leen GL, Finlay M. CT diagnosis of gall stone ileus. Acta Radiol. 1990;31:497-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Lobo DN, Jobling JC, Balfour TW. Gallstone ileus: diagnostic pitfalls and therapeutic successes. J Clin Gastroenterol. 2000;30:72-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Ihara E, Ochiai T, Yamamoto K, Kabemura T, Harada N. A case of gallstone ileus with a spontaneous evacuation. Am J Gastroenterol. 2002;97:1259-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kurtz RJ, Heimann TM, Beck AR, Kurtz AB. Patterns of treatment of gallstone ileus over a 45-year period. Am J Gastroenterol. 1985;80:95-98. [PubMed] |
| 13. | Syme RG. Management of gallstone ileus. Can J Surg. 1989;32:61-64. [PubMed] |
| 14. | Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60:441-446. [PubMed] |
| 15. | Rigler LG, Borman CN, Noble JF. Gallstone obstruction. Pathogenesis and roentgen manifestations. JAMA. 1941;117:1753-1759. [RCA] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 186] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Megibow AJ, Balthazar EJ, Cho KC, Medwid SW, Birnbaum BA, Noz ME. Bowel obstruction: evaluation with CT. Radiology. 1991;180:313-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 162] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Fukuya T, Hawes DR, Lu CC, Chang PJ, Barloon TJ. CT diagnosis of small-bowel obstruction: efficacy in 60 patients. AJR Am J Roentgenol. 1992;158:765-769; discussion 771-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 136] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Siewert B, Raptopoulos V, Mueller MF, Rosen MP, Steer M. Impact of CT on diagnosis and management of acute abdomen in patients initially treated without surgery. AJR Am J Roentgenol. 1997;168:173-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 76] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Balthazar EJ. George W. Holmes Lecture. CT of small-bowel obstruction. AJR Am J Roentgenol. 1994;162:255-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 146] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Maglinte DD, Balthazar EJ, Kelvin FM, Megibow AJ. The role of radiology in the diagnosis of small-bowel obstruction. AJR Am J Roentgenol. 1997;168:1171-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 123] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Machi J, Ikeda A, Yarofalir J, Yahara T, Miki N. Gallstone ileus with cholecystoduodenal fistula. Am J Surg. 2002;183:56-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Abou-Saif A, Al-Kawas FH. Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol. 2002;97:249-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 175] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 23. | Kasahara Y, Umemura H, Shiraha S, Kuyama T, Sakata K, Kubota H. Gallstone ileus. Review of 112 patients in the Japanese literature. Am J Surg. 1980;140:437-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 94] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Allen JW, McCurry T, Rivas H, Cacchione RN. Totally laparoscopic management of gallstone ileus. Surg Endosc. 2003;17:352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |