Published online Apr 7, 2005. doi: 10.3748/wjg.v11.i13.2039
Revised: August 30, 2004
Accepted: November 29, 2004
Published online: April 7, 2005
The case of a 22-year-old patient with symptomatic hypokalemia caused by rhabdomyolysis is presented as a rarely reported complication of gluten-sensitive enteropathy (GSE) and dermatitis herpetiformis Duhring. The patient’s myopathy ceased on potassium supplementation and her other complaints resolved while on gluten-free diet. Recovery was otherwise uneventful with a rapid decline in serum CPK level. At the time of her last follow-up a few months later, she was free of symptoms and CPK remained stable. Patients with GSE may present with hypokalemia in association with diarrhea and emesis, and if potassium loss is rapid, rhabdomyolysis may occur.
- Citation: Barta Z, Miltenyi Z, Toth L, Illes A. Hypokalemic myopathy in a patient with gluten-sensitive enteropathy and dermatitis herpetiformis Duhring: A case report. World J Gastroenterol 2005; 11(13): 2039-2040
- URL: https://www.wjgnet.com/1007-9327/full/v11/i13/2039.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i13.2039
Symptomatic hypokalemia caused by diarrhea is uncommon in adults. Rhabdomyolysis is an acute skeletal muscle disorder characterized by altered integrity of the cell membranes of muscle fiber cells and can be caused by a variety of factors whose nature is not necessarily traumatic. Hypokalemia is one of the most common metabolic causes, accounting for about 14-28% of rhabdomyolytic syndromes. Isolated cases of hypokalemic myopathy have been described in infections (salmonella, strongyloides, yersinia or giardia) or in patients with malabsorption[1-4]. We present a case of hypokalemic myopathy as a rarely reported complication in a patient with gluten-sensitive enteropathy and dermatitis herpetiformis Duhring treated at our department.
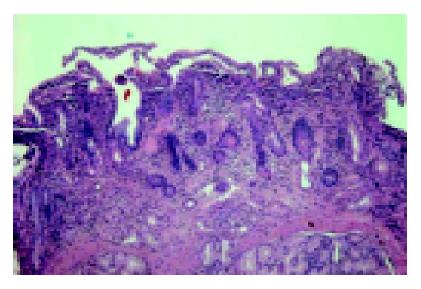
A 22-year-old female patient with chronic diarrhea, frequent vomiting, weight loss, fatigue and progrediating proximal type muscle weakness in her extremities was admitted to our clinic. There was no family history of renal or musculoskeletal disease nor had she experienced any trauma, drug abuse or vigorous exercise. She presented with bullous, intensely itching cutaneous lesions which clinically resembled Herpes zoster or dermatitis herpetiformis (Duhring’s disease) (Figure 1).
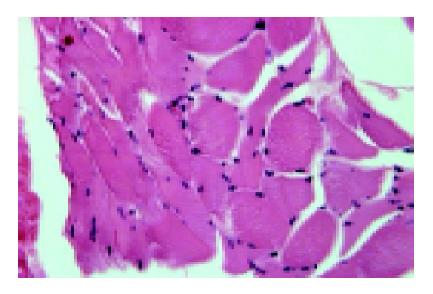
On physical examinations she was found undernourished. Laboratory findings confirmed hypokalemia (2.1 mmol/L) and high creatine phosphokinase, raised aldolase and lactic acid dehydrogenase levels. Other biochemical and hematological laboratory values were normal or in the normal range. She had no fever, fecal cultures were all negative, and serology for viruses was also negative, so no recent infection was to be suspected. There was a symmetrical and dominantly proximal muscular weakness of all four extremities. Mentation, cranial nerves and the results of sensory examination were normal. She developed symptoms suggestive of polymyositis, which is an autoimmune disease characterized by muscle weakness progressing over weeks or months with myalgia, muscle fiber necrosis, regeneration and mononuclear cellular infiltrate and myopathy, but further investigations (muscle biopsy, EMG and immunological investigations) excluded the disease (Figure 2).
Jejunal biopsy confirmed the typical histological findings of GSE; both IgG and IgA type antigliadin, antiendomysial and anti-tissue transglutaminase antibodies were positive (Figure 3).
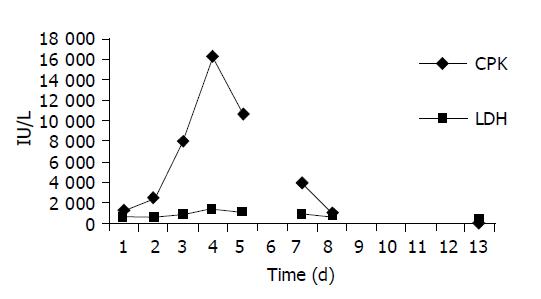
The dermatologist confirmed Duhring’s disease (diagnosis was made by skin biopsy). Both ECG and motor- as well as sensory-nerve conduction studies were normal but tests for urinary myoglobin were positive. Blood-chemical findings on admission and during hospitalization are shown in Figure 4.
The patient’s myopathy ceased on potassium supplementation and her other complaints resolved while on gluten-free diet. Recovery was otherwise uneventful with a rapid decline in serum CPK level. At the time of her last follow-up 18 mo later, she was symptom-free and CPK remained stable.
Dissolution of striated muscle fiber with leakage of muscle enzymes, myoglobin, potassium, calcium and other intracellular constituents can occur in anyone under particular circumstances and the consequences can be severe and sometimes fatal[5]. There are no studies on the incidence of rhabdomyolysis in the literature and many mild cases probably go unrecognized. Rhabdomyolysis is defined as an acute increase in serum concentrations of creatine kinase to more than five times the upper normal limit after myocardial infarction has been excluded as a cause (CK-MB fraction less than 5%). Visible myoglobinuria occurs when urinary myoglobin exceeds 250 µg/mL (normal <5 µg/mL), corresponding to the destruction of more than 100 g of muscle.
The causes of rhabdomyolysis are diverse but all lead to a critical increase in sarcoplasmic calcium and intracellular damage by activation of calcium-dependent proteases and phospholipases. Risk is increased by pre-existing metabolic factors such as hypokalemia, hypophosphatemia, and hyponatremia. Single episodes are most commonly caused by infections (viral, bacterial or other), drugs, or physical factors such as compartment syndromes, ischemia, reperfusion (including surgical procedures) and pressure from hard surfaces in comatose patients.
We present here a rare case of rhabdomyolysis. No symptoms of recurrent rhabdomyolysis were present suggesting that an inherited disorder of muscle metabolism was highly improbable. In addition, other precipitating factors (e.g., alcohol, trauma, strenuous exercise or - less frequently - hypothyroidism, metabolic myopathies or drugs) were either absent or could be excluded.
Two different possible interpretations for the pathophysiology of the myopathy were raised at start-up: polymyositis in which an infection played an indirect role as a trigger; and infection per se, both of which were excluded. In our patient, the clinical and histopathological features entirely met the diagnostic criteria for celiac disease with the co-existence of dermatitis herpetiformis.
Dermatitis herpetiformis or as formerly described in the literature, Duhring’s disease is an important associated disorder or complication of celiac disease which is manifested in the form of a skin rash and has a typical onset in the teens or in the third or fourth decades of life. Dermatitis herpetiformis is often referred to as “celiac disease of the skin”, while CD is referred to as “celiac disease of the gut.”
Patients with GSE may present with hypokalemia in association with diarrhea and emesis; if potassium loss is rapid, rhabdomyolysis may occur. As severe progressive neuromuscular symptoms do not seem to result from acute hypokalemia, unless there is preexisting potassium depletion, chronic diarrhea or malabsorption may be crucial for the development of hypokalemic myopathy. Malabsorption-associated hypokalemic rhabdomyolysis may be a severe complication and should be considered as a potential cause of rhabdomyolysis in GSE.
Science Editor Li WZ Language Editor Elsevier HK
| 1. | Guardino JM, Hix JK, Seidner D. A case of hypokalemia and rhabdomyolysis in a patient with short bowel syndrome. JPEN J Parenter Enteral Nutr. 2003;27:305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Williams SG, Davison AG, Glynn MJ. Hypokalaemic rhabdomyolysis: an unusual presentation of coeliac disease. Eur J Gastroenterol Hepatol. 1995;7:183-184. [PubMed] |
| 3. | Ertekin V, Selimoğlu MA, Tan H, Kiliçaslan B. Rhabdomyolysis in celiac disease. Yonsei Med J. 2003;44:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Cervelló A, Alfaro A, Chumillas MJ. Hypokalemic myopathy induced by Giardia lamblia. N Engl J Med. 1993;329:210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Criner JA, Appelt M, Coker C, Conrad S, Holliday J. Rhabdomyolysis: the hidden killer. Medsurg Nurs. 2002;11:138-143, 155. [PubMed] |