Published online Mar 21, 2005. doi: 10.3748/wjg.v11.i11.1728
Revised: September 23, 2004
Accepted: November 23, 2004
Published online: March 21, 2005
Of 5% of patients who develop liver cysts, only 10-15% of them come for medical attention, typically because of dull right upper quadrant pain, abdominal bloating or early satiety. We treated a 77-year-old female with a rare complication of inferior vena cava thrombosis. The patient expired due to septic shock and multiple organ failure.
- Citation: Leung TK, Lee CM, Chen HC. Fatal thrombotic complications of hepatic cystic compression of the inferior vena: A case report. World J Gastroenterol 2005; 11(11): 1728-1729
- URL: https://www.wjgnet.com/1007-9327/full/v11/i11/1728.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i11.1728
A 77-year-old female patient presented at a local emergency room with complaint of epigastric and abdominal fullness of 1-week’s duration. The patient had a history of endometrial carcinoma 10 years prior, treated with total hysterectomy. She had completed a course of chemotherapy and radiation therapy at that time. Bilateral ureteral strictures were noted. Subsequently, she did well except for episodic upper urinary tract infection.
One week prior to admission, the patient noted dull abdominal pain and nausea, aggravated by food intake, as well as, dyspnea. Temperature was 38 °C. She was referred to our hospital for further evaluation and management.
An ultrasound study revealed a large cystic lesion occupying most of the right lobe and segment IV of the liver, with an echogenic shadow layer[1-4] measuring 15 cm×12 cm. The patient was treated with antibiotics for presumed sepsis due to a hepatic abscess.
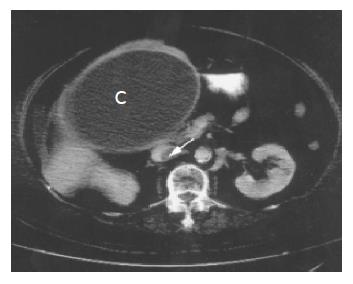
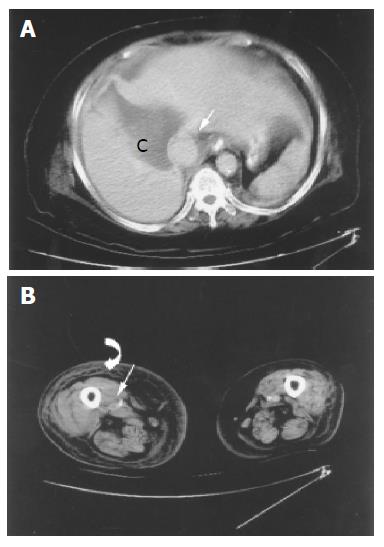
Progressive, bilateral swelling of the lower extremities was followed by cyanosis of the right foot. The foot was cool and pulseless. Abdominal spiral CT with and without contrast medium showed a 15-cm hepatic cyst with non-enhancing homogeneous low density (about 15 HU). There was a mild bilateral dilatation of the intrahepatic ducts. The cyst was associated with a mass compression effect on the inferior vena cava, with a 20-cm segment of thrombus extending from the inferior aspect of the porta hepatis through the right renal vein to the right femoral vein. Minimal ascites, bilateral basal pleural effusions and atelectasis were also noted. A sonographically guided drainage tube was inserted into the hepatic cyst[3,4]. The aspirate was grossly purulent and culture yielded E. coli (Figures 1, 2).
Cellulitis of the right lower extremity persisted in spite of ongoing heparin therapy. Despite the risks of conservative treatment[5-7], the patient’s general condition precluded surgical intervention. Though follow-up CT scan done a few days later, showed decrease in size of the cyst to approximately 9×4 cm2, with relief of mass effect, segmental thrombi continued to occupy the venous trunk and bilateral renal, right common iliac, right femoral and right popliteal veins. Cellulitis progressed with involvement of the buttocks and bilateral lower extremities. There was no evidence of pulmonary embolization. However, the patient expired 10 d later from multiple organ failure (Figure 3).
In general, inferior vena cava thrombosis (IVCT) results from deep vein thrombosis. However, isolated IVCT may occur. Examples include complication of malignancy (most often renal cell carcinoma, other genitourinary tumors, or hepatoma), extrinsic compression (most often due to retroperitoneal tumors and aneurysms of the abdominal aorta), post-traumatic hematoma (most often psoas muscle or common iliac artery injury), coagulopathy, iatrogenic causes, pregnancy or use of oral contraceptives and miscellaneous causes (including developmental anomalies and retroperitoneal fibrosis). Compression of the inferior vena cava by an intra-abdominal or pelvic mass has been associated with leiomyoma[8,9], adult polycystic kidney[10,11] and hepatic abscess[12].
A solitary liver cyst formation IVCT is very rare[13]. There are only three cases reported in the literature[1,2,13]. Reports of successful therapies for IVCT have included anticoagulation[1,2], placement of an inferior vena cava filter[2,13], or surgical intervention (resection)[5-7]. Such cysts, reported previously, have been even larger than this patient’s[1,2,13], whose cyst was not recognized prior to the onset of acute epigastric pain and nausea. Unfortunately, anti-coagulation was not successful and her condition precluded surgical intervention.
Because of her past history of endometrial cancer, the possibility of malignant recurrence was excluded by clinical, laboratory and imaging studies. The extent of thrombosis led us to suspect an underlying coagulopathy. In addition, normal venous return and lymphatic drainage of the pelvic cavity were possibly already distorted or damaged, perhaps by prior irradiation, resulting in venous stasis and turbulent flow. This hypothesis is supported by the evidence of post-irradiation sequelae of bilateral ureteral strictures and repeated urinary infection.
Medical management of IVCT includes anti-coagulation and thrombolytic agents[1,2]. Surgical therapy[1,2] involves vena cava interruption and thrombectomy. Both of these modalities are gradually being replaced by use of the relatively non-invasive venous filters. In this case, although shrinkage of the hepatic cyst occurred after sonographically guided drainage, the patient’s condition deteriorated due to septic shock and multiple organ failure, limiting surgical intervention.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Torzilli G, Santambrogio R, Vellini S, Palmisano A, Donadon M, Cornalba G, Montorsi M. Inferior vena cava thrombosis: an unusual complication of a large simple non-parasitic liver cyst requiring an integrated approach. Hepatogastroenterology. 2003;50:2188-2191. [PubMed] |
| 2. | Lermite E, Pessaux P, Jousset Y, Aubé C, Regenet N, Hennekinne-Mucci S, Arnaud JP. Compression of the inferior vena cava with thrombus: a rare complication of solitary liver cyst. Ann Chir. 2002;127:776-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 487] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 4. | Tokunaga K, Teplick SK, Banerjee B. Simple hepatic cysts. First case report of percutaneous drainage and sclerosis with doxycycline, with a review of literature. Dig Dis Sci. 1994;39:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Sanchez H, Gagner M, Rossi RL, Jenkins RL, Lewis WD, Munson JL, Braasch JW. Surgical management of nonparasitic cystic liver disease. Am J Surg. 1991;161:113-118; discussion 118-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 72] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Morino M, De Giuli M, Festa V, Garrone C. Laparoscopic management of symptomatic nonparasitic cysts of the liver. Indications and results. Ann Surg. 1994;219:157-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 109] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Ortega AE, Richman MF, Hernandez M, Peters JH, Anthone GJ, Azen S, Beart RW. Inferior vena caval blood flow and cardiac hemodynamics during carbon dioxide pneumoperitoneum. Surg Endosc. 1996;10:920-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Stanko CM, Severson MA, Molpus KL. Deep venous thrombosis associated with large leiomyomata uteri. A case report. J Reprod Med. 2001;46:405-407. [PubMed] |
| 9. | Dekel A, Rabinerson D, Dicker D, Ben-Rafael Z. Thrombosis of the pelvic veins associated with a large myomatous uterus. Obstet Gynecol. 1998;92:646-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Iguchi S, Kasai A, Kishimoto H, Suzuki K, Ito S, Ogawa Y, Nishi S, Gejyo F, Ohno Y. Thrombosis in inferior vena cava (IVC) due to intra-cystic hemorrhage into a hepatic local cyst with autosomal dominant polycystic kidney disease (ADPKD). Intern Med. 2004;43:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Peces R, Gil F, Costero O, Pobes A. Massive inferior vena cava thrombosis in a patient with autosomal dominant polycystic hepatorenal disease. Nefrologia. 2002;22:75-78. [PubMed] |
| 12. | Sharma MP, Sarin SK. Inferior vena caval obstruction due to amoebic liver abscess. J Assoc Physicians India. 1982;30:243-244. [PubMed] |
| 13. | Frisell J, Röjdmark S, Arvidsson H, Lundh G. Compression of the inferior caval vein--a rare complication of a large non-parasitic liver cyst. Acta Med Scand. 1979;205:541-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |