Published online Oct 1, 2004. doi: 10.3748/wjg.v10.i19.2922
Revised: June 15, 2004
Accepted: June 22, 2004
Published online: October 1, 2004
- Citation: Tacke F, Luedde T, Manns MP, Trautwein C. Regulation of plasma erythropoietin in chronic liver disease. World J Gastroenterol 2004; 10(19): 2922-2923
- URL: https://www.wjgnet.com/1007-9327/full/v10/i19/2922.htm
- DOI: https://dx.doi.org/10.3748/wjg.v10.i19.2922
In a May-issue of the World Journal of Gastroenterology, there is a very interesting study by Bruno et al[1] on erythropoietin (EPO) levels in patients with chronic liver disease. We have very recently reported a similar, but much larger study by Tacke et al[2] on the role of EPO in chronic liver disease. By comparing Bruno's results with our patient cohort and applying their criteria in a re-evaluation of our study population, we uncovered interesting differences between the two studies and could answer some of the key questions in the article raised by Bruno et ale.g. on the correlation of EPO with liver dysfunction and potential regulating factors in the clinical setting of liver cirrhosis.
Therefore, we would like to briefly present our data and compare the results with Bruno's recent study. We think the role of EPO is important in the pathophysiology of chronic liver disease, and the recent studies provided new insights into its regulation in liver cirrhosis.
Chronic anemia is a common clinical complication in patients with liver cirrhosis and is regarded as an important prognostic factor[3]. The great progress in the understanding of cytokine alterations in chronic liver diseases as well as the discovery and clinical application of different hematopoietic growth factors have raised attention to the potential pathophysiological role of erythropoietin (EPO) in liver diseases[4,5]. In a recent issue of the World Journal of Gastroenterology, Bruno et al[1] reported that increased EPO plasma levels were only detected in cirrhotic patients with hemoglobin concentrations below 12 g/dL and that this EPO response was inadequate compared to patients with iron-deficiency anemia. Furthermore, the authors did not observe an association between EPO levels and the stage of liver cirrhosis or liver synthesis function. The regulating factors in the pathophysiological setting of advanced liver diseases as well as possible clinical consequences remained an open question.
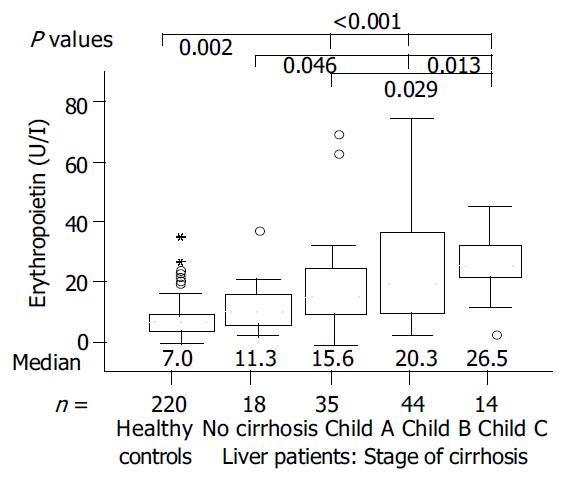
We analyzed 111 patients with chronic liver diseases who were evaluated for potential liver transplantation and 220 healthy (non-anemic) controls with the same EPO ELISA (R&D Systems, Wiesbaden, Germany) kit. In contrast to Bruno et al who studied mainly patients with viral hepatitis and advanced stages of cirrhosis, our much larger cohort comprised all Child's stages of cirrhosis in a fairly equal number of patients as well as different etiology subgroups. As we reported recently, EPO plasma levels clearly increased with Child's stage of liver cirrhosis[2], independent of the disease etiology (Figure 1). EPO also correlated directly with the markers of liver synthesis function, e.g. cholinesterase activity (r = -0.448, P < 0.001), albumin concentration (r = -0.358, P < 0.001), or prothrombin time (r = 0.300, P = 0.001). Interestingly, the absolute values of measured EPO levels in Bruno et al and our studies were relatively similar (e.g. mean EPO 11.6 U/L for chronic hepatitis by Bruno et al median EPO 11.3 U/L for our “non cirrhosis" group), thereby raising the question whether the clear association between EPO and stage of liver cirrhosis could have been observed if the number of patients included in Bruno et al study was high enough. Furthermore, it is hard to believe that EPO was normally distributed in anemic or non-anemic cirrhotic patients as the mean ± SD values suggested by Bruno et al, thus a different statistical analysis using median and U-test could possibly uncover these important correlations.
We also found a significant inverse correlation between EPO levels and hemoglobin in patients with chronic liver diseases (r = -0.498, P < 0.001, Spearman rank correlation analysis). As this was described by Bruno et al only for patients with iron-deficiency anemia, this correlation could not be observed when we divided our liver disease patient group by the criteria of Bruno et al into so-called anemic or non-anemic patients (hb ≤ 12, n = 48, vs hb > 120 g/L, n = 63). However, in accordance with Bruno et al, we also found significantly elevated EPO levels in anemic vs non-anemic liver disease patients (median EPO 29.3 vs 11.4 U/L, P < 0.001, U-test). In contrast, the non-anemic liver disease patients also had elevated EPO levels as compared with controls (P < 0.05), which could be possibly explained by the much larger control group in our study.
In further investigating the potential regulating factors, one should consider the complex clinical picture of advanced liver cirrhosis. As we could show, the degrees of anemia and liver dysfunction not only were independent parameters associated with elevated EPO in chronic liver disease, but also impaired pulmonary function[2]. Changes in pulmonary function test and blood gas analysis were commonly found in our study population, and EPO was inversely correlated with carbon dioxide tension (pCO2) and elevated in patients with reduced (carbon monoxide) diffusion capacity. In addition, we noticed a positive correlation between interleukin-6 and EPO, thereby possibly linking the EPO response to a common protective cytokine response usually seen in liver cirrhosis[6].
In conclusion, the recent studies by Bruno et al and our group provide some new important insights in the regulation of plasma EPO in chronic liver diseases. EPO plasma levels are apparently upregulated in patients with liver cirrhosis, and one might speculate whether this increase is sufficient in the setting of chronic anemia when compared with other forms of anemia, e.g. iron-deficiency. However, the regulation of plasma EPO is complex and multifactorial, and the degrees of anemia, liver dysfunction, impaired pulmonary function and cytokine alterations are the major factors in regulating plasma erythropoietin in patients with chronic liver diseases.
Edited by Xu XQ, Wang XL and Zhang JZ
| 1. | Bruno CM, Neri S, Sciacca C, Bertino G, Di Prima P, Cilio D, Pellicano R, Caruso L, Cristaldi R. Plasma erythropoieti. n levels in anaemic and non-anaemic patients with chronic liver diseases. World J Gastroenterol. 2004;10:1353-1356. [PubMed] |
| 2. | Tacke F, Schöffski P, Luedde T, Meier PN, Ganser A, Manns MP, Trautwein C. Analysis of factors. contributing to higher erythropoietin levels in patients with chronic liver disease. Scand J Gastroenterol. 2004;39:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Orrego H, Israel Y, Blake JE, Medline A. Assessment of progno. stic factors in alcoholic liver disease: toward a global quantitative expression of severity. Hepatology. 1983;3:896-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 129] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Pirisi M, Fabris C, Falleti E, Soardo G, Toniutto P, Gonano F, Bartoli E. Evidence for a multi. factorial control of serum erythropoietin concentration in liver disease. Clin Chim Acta. 1993;219:47-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Yang YY, Lin HC, Lee WC, Huang YT, Hou MC, Lee FY, Chang FY, Lee SD. Plasma erythropoieti. n level in patients with cirrhosis and its relationship to the severity of cirrhosis and renal function. J Gastroenterol Hepatol. 2003;18:1156-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Streetz KL, Tacke F, Leifeld L, Wüstefeld T, Graw A, Klein C, Kamino K, Spengler U, Kreipe H, Kubicka S. Interleukin 6/gp130-. dependent pathways are protective during chronic liver diseases. Hepatology. 2003;38:218-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 130] [Article Influence: 5.9] [Reference Citation Analysis (0)] |