INTRODUCTION
Malignant gastric tumors are still considered a contraindication for laparoscopic surgery by many surgeons. However, the removal of benign tumors laparoscopically has been widely accepted as a feasible alternative to laparotomy[1-6]. The most frequent benign gastric tumor is leiomyoma, and extensive resection is indicated because it is difficult to differentiate it from leiomyosarcoma only by biopsy. When a gastric submucosal tumor is laparoscopically removed, it is recommended to resect a sufficient margin of the surrounding normal tissues in the event that the tumor is malignant[5,7-14].
Laparoscopic resection of a gastric fundus tumor on the anterior wall is relatively easy, in which a wedge of stomach can be resected under laparoscopic vision using an Endo GIA after the lesion is marked endoscopically. However, laparoscopic resection of tumors on the posterior wall of gastric fundus, especially when they are next to the esophagocardiac junction (ECJ), is both difficult and time-consuming. Furthermore, it can lead to inadvertent esophagus stenosis and injury to the spleen[14-18]. In order to overcome these difficulties, we proposed a new technique for the management of submucosal tumors located on the posterior wall of gastric fundus and next to ECJ, which was laparoscopically extraluminal resection of the gastric fundus.
MATERIALS AND METHODS
Materials
From January 2001 to September 2003, 15 procedures of laparoscopically extraluminal resection of the gastric fundus were carried out for the submucosal tumors located on the posterior wall of gastric fundus and next to EJC. There were 11 male and 4 female patients with an average age of 58 years (range, 38 to 78 years). The complaints at admission included upper gastrointestinal bleeding (10 cases, 66.7%) and abdominal pain (4 cases, 26.7%). The remaining one (6.7%) was diagnosed when having a physical checkup. Preoperative examinations included gastroscopy, ultrasonic gastroscopy, and barium swallow examination of the upper gastrointestinal tract, all of which revealed a submucosal lesion on the posterior wall of gastric fundus near the ECJ with a regular margin. Since these tumors could not be lifted by intrasubmucosal injection of normal saline, gastroscopic local tumor resections were not indicated. Besides, gastroscopy suggested the presence of ulcers at the center of tumor surfaces in 11 patients. The neoplasm diameter ranged 3.0-6.5 cm with a mean value of 4.8 cm. The distance of the neoplasm margin from ECJ was about 1.5-2.5 cm (Figure 1).
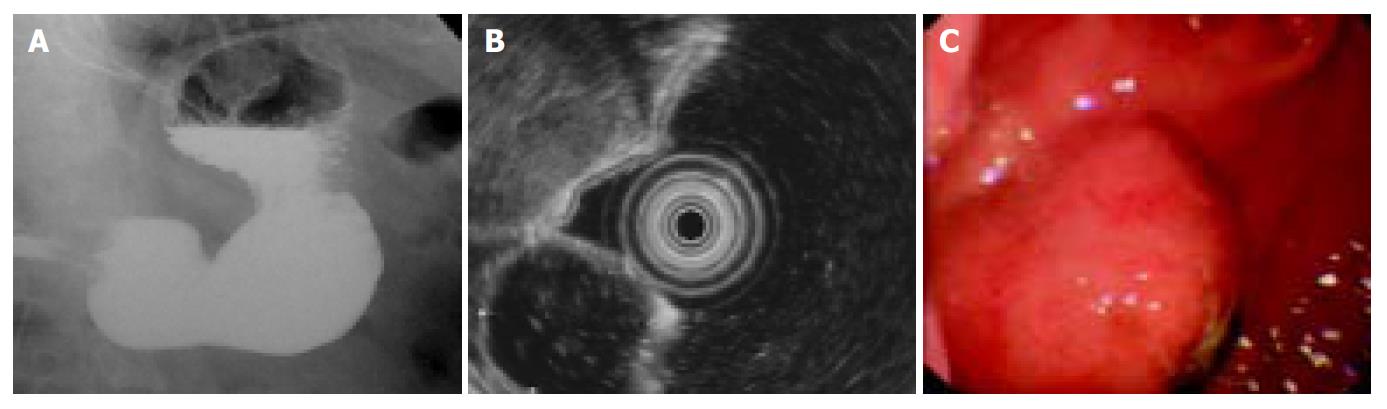
Figure 1 Submucosal tumors on gastric fundus diagnosed in preoperative examinations.
A: A lesion near to ECJ with a clear-cut margin shown in barium swallow examination of upper gastrointestine; B: A lesion with a clear-cut margin protruded into gastric lumen shown in ultrasonic gastroscopy; C: A hemisphere-like projection in the posterior wall of gastric fundus and an ulcer in its center shown in gastroscopy.
Surgical Methods
Anesthesia and position After general anesthesia under bronchial intubation, the patient was placed in a supine position with both legs abducted 30o. The surgeon stood between the patient’s legs while the laparoscopic holder and the operative assistant on the right and left sides of the patient, respectively.
Portal positions Trocars with 5 mm or 10-12 mm in diameter were placed in the umbilicus, the left or right midclavicular line, and under the xiphoid (Figure 2).
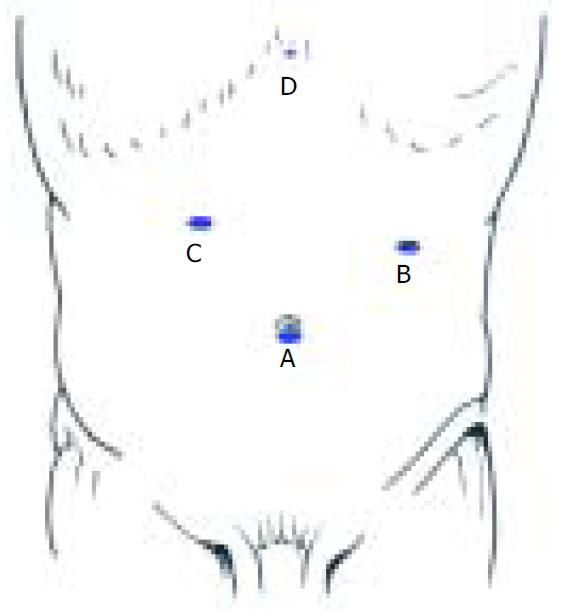
Figure 2 Trocar positions for laparoscopically extraluminal resection of gastric fundus.
A: Endoscope portal (10 mm); B, C: Main working portals (10-12 mm); D: Assisting working por-tal (5 mm).
Localization of tumors Under laparoscopy, three methods could be used for neoplasm localization: naked eye inspection, instrument exploration, and intra-operative gastroscopy[19]. In this series, the neoplasms had a relative large diameter. So the localization was realized via naked eye inspection and instrument exploration except in four cases under the help of gastroscopy. To perform this operation, it was also important to confirm the distances between tumors and ECJ after the tumors were localized.
Dividing omentum, entering omental bursa, and dividing splenogastric ligament Omentum dissection was begun from the middle-inferior pole of spleen and proceeded along outside of gastroepiploic vascular arch. After entering the omental bursa, the gastric posterior wall was turned to right by three-finger forceps. Next, the short gastric vessels were coagulated and cut with the ultrasonically activated scalpel to completely divide the gastric fundus from the superior pole of spleen.
Dissection of the left side of cardiac orifice to expose ECJ
Resection of gastric fundus using Endo GIA Figure 3A shows the cutting line of Endo GIA. The firing times of Endo GIA depended on the size of tumors. Complete resection of tumors with a sufficient margin usually required 2-3 sequential firings. When Endo GIA was placed near the left side of cardia, special care was taken to ensure that ECJ was not involved to avoid postoperative esophagus stenosis (Figure 3B).
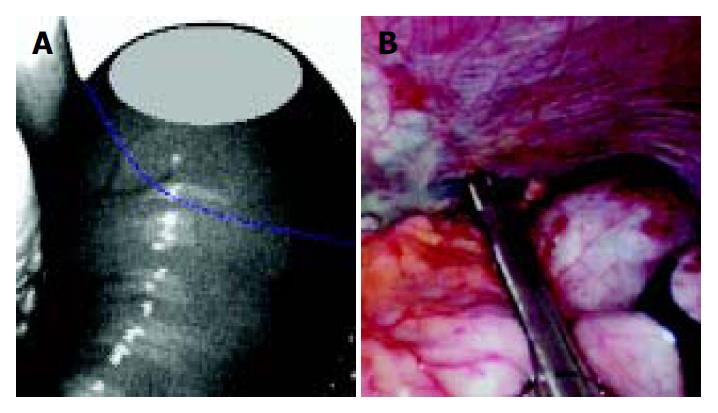
Figure 3 Resection of gastric fundus with Endo GIA.
A: The blue line represents the Endo GIA resection line; B: When Endo GIA was placed near the cardia, special care was taken to ensure that ECJ was not involved.
Taking out of specimens Specimens were taken out through portal B after they were put in the specimen bag. Pathological examination was routinely carried out during the procedure.
The surgical field was irrigated and drainage tube was placed under the left diaphragm.
RESULTS
In this series, the mean operative time, blood loss, and postoperative hospital stay were 66.2 ± 10.4 min (range, 55 to 90 min), 89.4 ± 21.7 mL (range, 50-200 mL), and 5.3 ± 1.1 d (range, 4-7 d), respectively. On the first postoperative day, the abdominal drainage was 40-180 mL (average, 60.7 ± 14.3 mL). Of all the patients, 73.3% recovered their gastrointestinal function within 36 h after operation and began to eat and to walk. The slowest recovery of gastrointestinal function occurred 60 h post-operation.
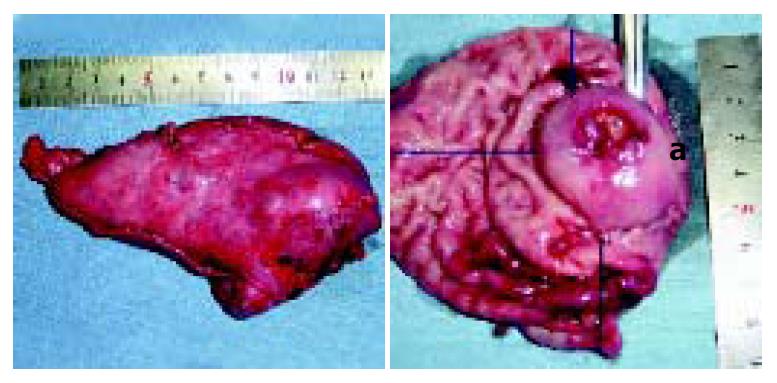
Figure 4 shows the resected specimens. The distance of the tumor to the section edge was: (1) 1-1.5 cm to ECJ, with an average of 1.1 ± 0.3 cm; (2) 2.5-6 cm to the other three edges, with an average of 3.9 ± 1.2 cm. The intra-operative frozen sections suggested that all the tumors were benign. But the postoperative paraffin-embedded sections revealed two cases of mesenchymoma with a low malignancy. In these two cases, the distance of the tumor to ECJ was 1.3 cm and 1.5 cm respectively, and the distance to the other three edges was greater than 3 cm. The extensive salvage operation was not carried out, and a follow-up period of 18 mo and 22 mo, respectively, did not find any recurrence and metastasis. In the other 13 cases, leiomyoma was diagnosed in 8 cases, mesenchymoma in 4 cases, and neurofibroma in 1 case.
Figure 4 Resected specimens.
Line a: the distance of the tumor to ECJ.
All the 15 laparoscopic surgeries were carried out successfully with no apparent lesion left, and no complication and conversion to open surgery occurred. Follow-up was continued for 3.5-33 mo and revealed no abnormality.
DISCUSSION
Clinically, gastric benign tumors are difficult to differentiate into malignancy. Even in benign tumors, canceration and severe complications of obstruction and bleeding may take place latter. So, active measures should be taken to surgically resect the tumors. As to the resection depth, the tendency was to remove the total layer of gastric wall[20-22]. Under gastroscopy, some gastric tumors could be excised via the intrasubmucosal injection of normal saline. However, this technique is applied mainly to the resection of mucosal tumors and not effective on submucosal neoplasms. Furthermore, the whole thickness of gastric wall could not be removed using this method. In the past, laparotomy was primarily performed to resect gastric submucosal tumors. With the advent of minimally invasive surgery, laparoscopic resection has become the first choice of many surgeons[23-26].
Submucosal tumors in the fundus or cardia of stomachs can be managed via laparoscopic proximal gastrectomy. However, postoperative reflux esophagitis is common. For most benign gastric submucosal tumors, the range of excision is too large and the procedure is too invasive[27-31]. Laparoscopic wedge resection of stomachs is the most commonly seen procedure for submucosal tumors of gastric fundus[31-34]. The tumor on the anterior wall of fundus is easy to excise with Endo GIA[20]. But for submucosal tumors on the posterior wall of gastric fundus, especially when next to ECJ, the wedge resection of stomachs is quite difficult, and caution should be taken to protect ECJ from postoperative esophageal stenosis and the spleen from injury, especially its superior polar.
In our early experience, we managed to resect submucosal tumors on the posterior wall of gastric fundus through the window of gastrotomy on the anterior gastric wall. The procedure was performed as follows: to cut open the anterior wall of the gastric body or fundus firstly (gastrotomy on the anterior gastric wall), to extract the posterior wall of gastric fundus through this cut, and to excise the tumor on the posterior gastric wall with Endo GIA or the method of stripping plus endoscopic suturing[35]. This method, though relatively easy to carry out and with quite a good outcome, has the disadvantage of seriously intra-operative abdominal contamination of gastric juice. Furthermore, this method cannot achieve good exposure of ECJ and has not been used in the excision of tumors on the posterior wall near ECJ. Sekimoto et al[20] reported that intraluminal resection of the full thickness of posterior gastric wall lesion was performed to manage submucosal tumors on the posterior wall of gastric fundus near ECJ. In this study, balloon-tip trocars were inserted directly into the gastric lumen and gas was charged into the stomach through the trocars, then wedge resection of the posterior wall tumor was completed under direct vision with Endo GIA. The authors believe that the procedure has fewer traumas to patients and less opportunity of intraperitoneal contamination by gastric juice than gastrotomy on the anterior gastric wall. ECJ was always in the surgeon’s sight, so the distance between the resection line and ECJ could be continously monitored, which means less morbidity of postoperative esophageal stenosis. However, we think that the above two methods have the same disadvantage of a limited range of resection and a higher incidence of spleen injury in that the short gastric vessels were not cut and especially that the superior pole of the spleen was not completely divided from gastric fundus. Moreover, care must be taken that the lateral tension to the gastric wall from gas inflation cannot be excessive, otherwise, injury of splenic capsule or gastric wall laceration might occur[15-18,20].
In order to solve these problems, we proposed a new laparoscopic approach to surgical resection of submucosal tumors on the posterior wall of gastric fundus. In this technique, the omentum is dissected to get access to the omental bursa. So, the splenogastric ligament could be severed to completely dissect the gastric fundus away from the superior pole of spleen. Then the left side of cardiac orifice is dissected to expose ECJ, and the gastric fundus is resected with the Endo GIA. Through these measures, the newly designed approach, laparoscopically extraluminal resection of gastric fundus, could avoid intraperitoneal contamination, the spleen injury and the postoperative esophagus stenosis. Meanwhile, it could also provide a sufficient range of gastric resection. The main disadvantage is the increased steps required. However, with necessary training and skills in the laparoscopic surgery, the procedure can be accomplished not quite both difficult and time consuming. The average operation time in our series was only 66.2 ± 10.4 min. The procedure, we think, is both safe and effective in that the ECJ and the superior pole of spleen are under the continuous supervision of the operator when resecting the gastric fundus, and that the procedure can provide a more sufficient range of resection.
When the laparoscopically extraluminal resection of gastric fundus is performed, two key points must be stressed. One is that the interspace between gastric fundus and superior pole of spleen must be adequately dissected. The other is that when Endo GIA is placed near the cardia, special care must be taken to ensure that ECJ is not involved. So long as the above key points are fulfilled, our method is safe, easy and beneficial to the laparoscopic resection of submucosal tumors on the posterior wall of gastric fundus.