Published online Oct 1, 1995. doi: 10.3748/wjg.v1.i1.60
Revised: June 20, 1995
Accepted: August 20, 1995
Published online: October 1, 1995
- Citation: Yu GH, Su ZG, Zou J, Wang YB. Esophageal Crohn's disease: A case report. World J Gastroenterol 1995; 1(1): 60-61
- URL: https://www.wjgnet.com/1007-9327/full/v1/i1/60.htm
- DOI: https://dx.doi.org/10.3748/wjg.v1.i1.60
Crohn’s disease is relatively rare and may occur in any part of the digestive tract. However, according to domestic reports, less than 10% of the disease is found in the upper digestive tract and even less in the esophagus. Here, we report the case of an 81-year-old man who was originally diagnosed with esophageal cancer because of progressive dysphagia. After he was admitted to our hospital, we carried out a series of examinations and diagnosed him with esophageal Crohn’s disease. We discuss the differential diagnosis of esophageal cancer and esophageal Crohn’s disease.
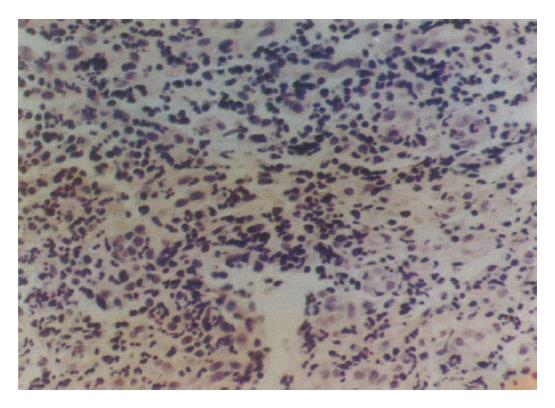
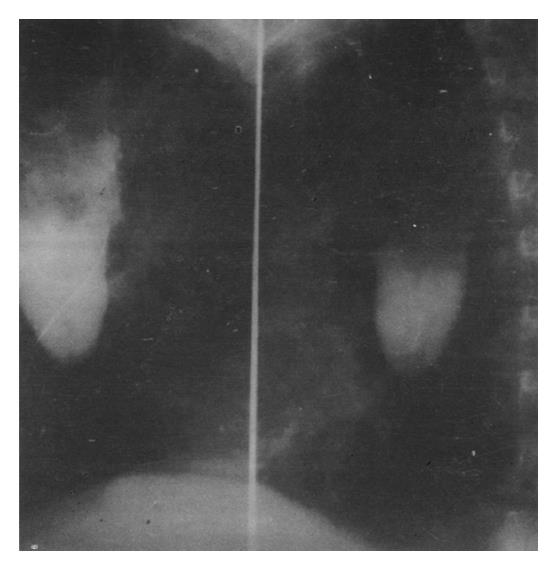
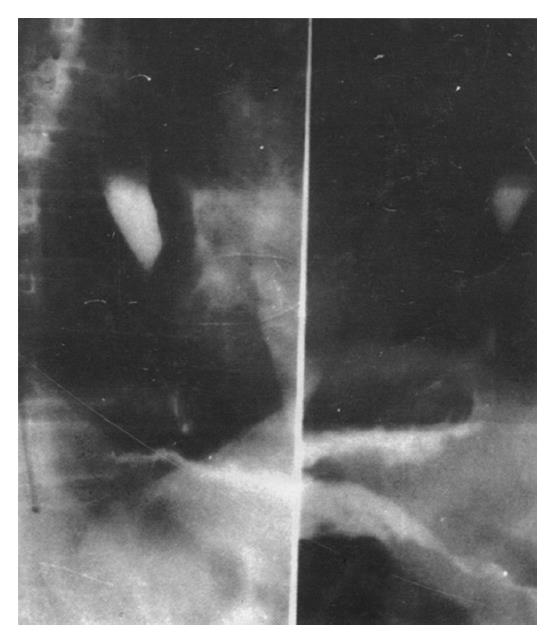
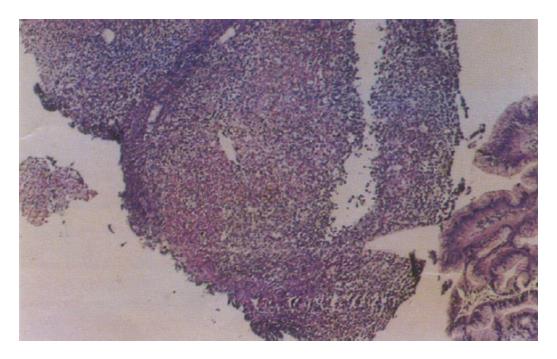
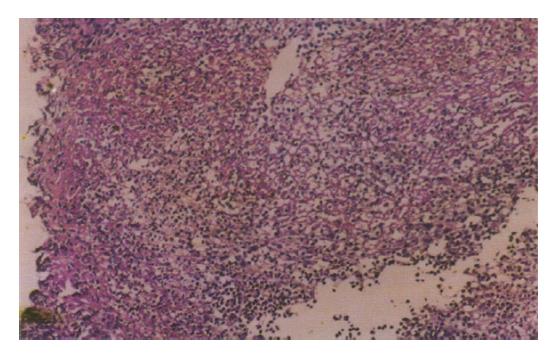
An 80-year-old man began to have progressive dysphagia in Feb 1992. In June, he was able to take only a small amount of liquid food without any other symptoms. The evident esophageal stenosis, located 30 cm from incisor teeth, was found by gastroscopy, and the gastroscope could not be passed through it. There was about 5 cm esophageal mucosa stiffness, and the area above the stenosis appeared dirty. Biopsy revealed that the mucosa had congestion and edema, and granulation tissue was found in the submucosa. A clinical diagnosis of esophageal cancer was made. Since then, his dysphagic symptoms gradually subsided without any treatment, and the patient was asymptomatic for the next 26 mo. At this time, his condition began to rapidly deteriorate until 1994. He had difficulty drinking water and vomited mucous secretion frequently. Weight loss amounted to 10 kg. The results from a second gastroscopy were similar to those of the first. Clinical diagnosis was still esophageal cancer. General treatment was of no use, and he was admitted to our hospital for endoscopic treatment on June 20, 1994. During history taking, he said: “I am healthy” and denied having any suffering or other symptoms. Physical examination revealed that his temperature, pulse, and blood pressure were normal; and no obvious positive findings were found on systemic examination, except for some weight loss and a narrowing of his chest. Laboratory examination of blood, urine, and stool was routine; and plasma albumin and globulin, alanine aminotransferase (ALT), blood urea nitrogen (BUN), creatine, blood sugar, serum potassium, and sodium chloride were all normal. Erythrocyte sedimentation rate (ESR) was slightly elevated, being 22 mm/h. Stool occult blood was negative. There was fungus present in the esophageal mucosa. X-ray chest film, electrocardiogram, and ultrasonic electrocardiogram were normal. B type ultrasonic examination showed one 3.5 cm × 3.5 cm stone in his gallbladder. The third gastroscopy done on June 29 revealed evident esophageal stenosis 32 cm distal to the incisor teeth, with a luminal diameter of approximately 1 mm. Findings proximal to the stenosis were the same as that on first examination. Biopsy reported an abundance of inflammatory necrotic tissue that contained fibrotic cells and granulation tissues, with blood capillaries and inflammatory cells. Normal esophageal mucosa was not found (Figure 1). In order to understand the condition of the stenosis in the lower esophagus, we used 38% biligrafin to examine the esophagus both by mouth and through gastroscope pouring. X-ray film revealed an almost complete obstruction. Its margin was smooth and complete, and there was no mucosal destruction (Figure 2). There was a 4 cm string like stenosis below the obstruction; but its margin was complete, and the cardia opened normally (Figure 3). Initial differential diagnosis: 1. esophageal Crohn's disease; 2. esophageal cancer; or 3. gallbladder stone (inactive stage). On July 7, a trial treatment was carried out to target esophageal Crohn's disease under careful observation by intramuscular injection of dexamethasone (10 mg twice daily). The patient's dysphagic symptoms gradually improved after 3 d. He could take solid food after 6 d. However, on day 6 of treatment, he felt epigastric pain and suddenly vomited blood. Emergency gastroscopy revealed that the original esophageal stenosis disappeared. The mucosa of the middle and lower part of the esophagus appeared whitish, thickened, and coarse. There were superficial erosions and an ulcer. A ring like stenosis, approximately 5 cm above the cardia, was found; but the gastroscope could not get to the stomach smoothly, and there was a lot of retained bloody fluid. After the fluid was cleared away, many small erosions and blood oozing sites were found spread over the stomach fundus and body, with atrophic changes over the whole stomach, including the fundus, body, and antrum. The pylorus was slightly deformed, and there was evident congestion at the duodenal bulb. Blood oozing stopped after spraying with mansa's solution and thrombin. Endoscopic differential diagnosis: 1. esophageal Crohn's disease; 2. acute gastric mucosal disease; and 3. chronic atrophic gastroduodenitis. After emergency gastroscopy, dexamethasone was reduced to 5 mg twice daily by intramuscular injection. Then, the patient instead received prednisone 50 mg/d and a proton pump inhibitor and De Nal. The patient had no symptoms afterwards. Barium meal examination was performed, and no evident diseases were found below the esophagus 30 d after treatment. The fifth gastroscopy revealed that the ring-like stenosis still existed 32 cm distal to the incisor teeth, but the gastroscope could not pass through. There were a few superficial ulcers on the esophagus, but erosions of the stomach fundus and body disappeared, leaving some atrophic change. Biopsies from the antrum, fundus, and body of the stomach and esophagus found: (1) chronic atrophic gastritis; (2) presence of inflammation and granulation tissue on the mucosa of the lower esophagus. Ulceration was considered, and some parts seemed to crack like ulcers. These findings were consistent with esophageal Crohn's disease (see Figures 4 and 5). The patient took prednisone continuously and left the hospital without any symptoms. The total hospital stay was 52 d. After discharge from the hospital, he continued to take prednisone, and his condition remained very good. The symptoms only reappeared when he stopped taking medicine, and they disappeared when the patient continued to take medicine. Follow-up has been done for one year, and the patient is still healthy.
Pathological diagnosis is considered the gold standard for detection of Crohn’s disease. During their research on 41 children suffering from Crohn’s disease and 47 children from ulcerative colitis with pathological changes in the upper digestive tract, Runska et al found that only 12 children developed Crohn's disease granuloma (one case in the esophagus, eight in the stomach, and three in the duodenum), all of which were confirmed by pathological diagnosis. Therefore, symptoms only cannot rule out Crohn's disease and ulcerative colitis, and pathological diagnosis is crucial. Based on medical records of 24 children of the same age with Crohn's disease, Schmidt-Sommerfeld et al pointed out that if a patient is suspected of suffering from Crohn's disease, biopsy and pathological examination were required even though the mucosa looked normal during gastroscopy. Otherwise, the histological changes of the disease might be neglected, and a definite diagnosis would be delayed. In our case, the reason why the patient was misdiagnosed as esophageal cancer three times was that changes of the stenosis of the esophageal mucosa initially could not be detected because of the severe degree of stenosis of the esophageal lumen. It was only after trial treatment when the esophageal obstruction disappeared was a biopsy of the stenosis taken, allowing for the final diagnosis of Crohn's disease to be established. It is only by pathological diagnosis that Crohn's disease can be definitely differentiated from esophageal cancer, especially in elderly patients.
Original title: China National Journal of New Gastroenterology (1995-1997) renamed World Journal of Gastroenterology (1998-).
S- Editor: Filipodia L- Editor: Jennifer E- Editor: Zhang FF