Published online Oct 1, 1995. doi: 10.3748/wjg.v1.i1.48
Revised: June 20, 1995
Accepted: August 20, 1995
Published online: October 1, 1995
AIM: To investigate the pathogenesis of abnormal gallbladder (GB) emptying and the effect of domperidone (Dom) on GB emptying in patients with irritable bowel syndrome (IBS).
METHODS: The effects of DOM on GB emptying were studied in 20 IBS patients and 18 healthy controls by real time ultrasonography, using randomized, double-blind, and controlled methods.
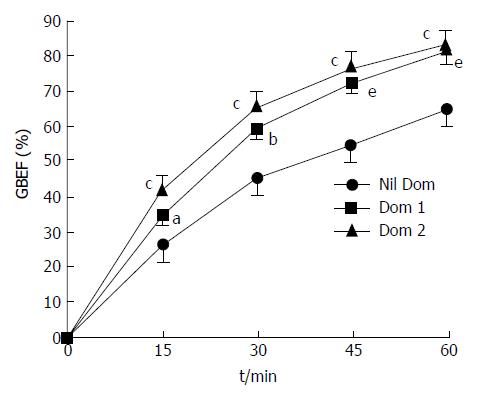
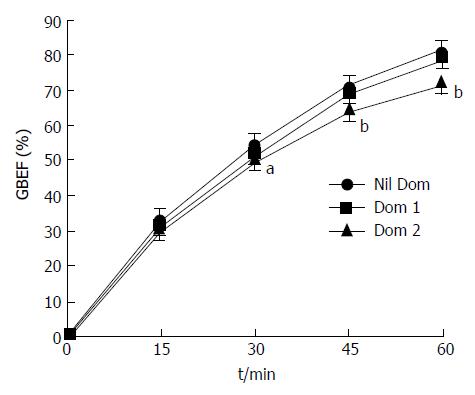
RESULTS: Fasting GB volume was significantly higher in IBS patients than in controls (24.136 ± 1.38 cm3vs 19.793 ± 1.487 cm3, x-± sx-, p < 0.01). In controls, 30 min after 10 mg Dom orally, the GB ejection fraction (GBEF) was decreased significantly (p < 0.005), and the magnitude of this decrease was greater after 20 mg Dom. The difference between these two doses was not significant (p > 0.05). In IBS patients, GBEF was significantly increased 15 min after 10 mg Dom orally (p < 0.01), and the magnitude of this increase was greater with 20 mg Dom (p < 0.001). This difference was even more marked with prolongation of time after oral Dom. The GBEF in IBS patients with segmental contraction was significantly less than that with hypermotility (p < 0.01), and the increase of GBEF was more marked after oral Dom in IBS patients with segmental contraction than those with hypermotility (p < 0.01).
CONCLUSION: GB emptying function is abnormal in patients with IBS. The feeble contractility of the GB and/or the incomplete relaxation of Oddi sphincter may be factors that directly affect GB emptying in IBS patients. Dom can significantly improve GB emptying function and may decrease the risk of forming GB stones in these patients.
- Citation: Chen SZ, Chen XC, Liu WX, Yang ZS, Guo XL. Domperidone improves gallbladder emptying function in patients with irritable bowel syndrome. World J Gastroenterol 1995; 1(1): 48-51
- URL: https://www.wjgnet.com/1007-9327/full/v1/i1/48.htm
- DOI: https://dx.doi.org/10.3748/wjg.v1.i1.48
Irritable bowel syndrome (IBS) is a chronic disease with smooth muscle dysfunction in many organs[1-4]. In IBS patients, abnormal gallbladder (GB) emptying function, increased fasting GB volume (GBV), and incomplete postprandial GB emptying have been found[5,6]. Nevertheless, the pathogenesis of abnormal GB emptying remains unknown, and there is no reasonable treatment strategy for improving GB emptying in IBS patients. Domperidone (Dom), a dopamine receptor antagonist, can promote stomach emptying[7], but it is not clear whether it can improve GB emptying in IBS patients. There are adrenergic and cholinergic receptors in the smooth muscle of the GB and the Oddi sphincter (OS)[8], and it is assumed that there may be dopamine receptors in these sites, thereby explaining the effect of Dom on GB emptying. Because decreased GB emptying is a predisposing factor for GB stone formation, it is necessary to investigate the pathogenesis of abnormal GB emptying in patients with IBS and to observe the effect of Dom on GB emptying. Here, we performed a randomized, double-blind, controlled study using ultrasonography to measure GBV and to investigate the effect of Dom on GB emptying.
Twenty patients with IBS (IBS group) and 18 healthy controls (control group) were included in this study, and these two groups were comparable for age, sex, height, and body weight (Table 1).
| Characteristics | Patients (n = 20) | Controls (n = 18) |
| Mean age (a) | 33.15 ± 2.16 | 32.85 ± 2.25 |
| (Range) | (18-56) | (22-54) |
| Males/Females | 11/9 | 9/9 |
| Mean weight (kg) | 59.45 ± 1.47 | 57.77 ± 1.26 |
| (Range) | (46.5-70.4) | (47.0-67.5) |
| Mean height (cm) | 165.50 ± 1.13 | 166.80 ± 1.21 |
| (Range) | (155.5 ± 178.2) | (154.6 ± 179.0) |
| Mean body index (kg/m2) | 22.24 ± 1.21 | 22.07 ± 1.26 |
| mass (Range) | (16.24 ± 26.21) | (17.69 ± 24.82) |
All patients were randomly selected inpatients, and their disease courses were between 2 to 28 (mean 8.7) yr without any operation history. Clinical, laboratory, and other examinations revealed no organic pathologic process and no gastrointestinal disorders induced by diabetes mellitus, etc., and IBS was diagnosed in accordance with the criteria[9]. According to criteria[10] based on main manifestations of the digestive tract, nine patients were classified with hypermotility type (in which the main manifestations were diarrhea or accompanied by abdominal pain), seven patients were classified as segmental contraction of intestine type (in which the main symptoms were abdominal pain and dry feces, the frequency of bowel movement might not decrease), and the remaining four cases could not be classified into the other two categories and were included in a separate group. All drugs were stopped 3 d before ultrasonographic examination.
Healthy subjects (Table 1) were randomly selected healthy volunteers who had no disease in the livers, GB, pancreas, or gastrointestinal tract, and all had normal tests for blood sugar and lipids. Alcohol was avoided 3 d before and during the study.
All subjects fasted for 12 h and were examined using the same real time ultrasonographic unit (SSD-630, Hitachi Aloka Medical Ltd., Tokyo, Japan). GBV was determined according to the method of Jonderko et al[11] by the same investigator who did not know the aims and contents of the study and the diagnosis of the patients. The examination was carried out in the same position, same place (skin guide marks were used in each case), and same phase of respiration each time for each subject. GBV was calculated by the formula.
V = 1/6π·L·W·H
Where: V is GBV, L is GB length (sagittally), W is width, and H is GB height. The GB ejection fraction (GBEF) was calculated by the formula for each considered interval after the meal stimulus:
GBEFt = (Vf - Vt)/Vf × 100%
where: GBEFt is GB ejection fraction at time t (t = 15, 30, 45, 60 min), Vf is before the meal GBV, Vt is GBV at time t.
Drug preparation: The powder of 10 mg (Dom1) and 20 mg (Dom2) (product of Janssen Pharmaceutical Ltd, Xi’an, China) was filled in a separate capsule of the same color and size by a pharmacist, and bottled and labeled as “three” and “four”.
GBV measurement: All subjects received ultrasonography separately at 8:30 AM in the recumbent position, and the fasting GBV was determined three times and the mean values were taken to be a reference value. Then, a fatty meal (260 mL cream and egg containing 35 g fat) was given to the subject to take within 2 min. The GBV was determined at 15 min intervals for 60 min. On a separate day, the fasting GBV was determined in the same way as above. Afterwards, an investigator, who did not know the name of the drug in the capsule, randomly took a capsule (the number and order were recorded) and gave it to the subject to take. Ten minutes later, the fatty meal was given as previously. A small drink of water (50 mL) was allowed to facilitate the passage of the capsule along the esophagus. The subjects lay on a couch while the GBV measurement was being taken, and they were allowed to move freely between measurements.
GBV (cm3) and GBEF (%) are expressed as x-± s. Paired Student's t test was used to compare the difference between two groups, and linear regression was used to analyze the relationship between variables. p < 0.05 (two sides) was considered to be statistically significant.
All subjects completed the study. The fasting GBV in the IBS group (24.136 ± 1.138 cm3) was significantly higher than that in controls (19.793 ± 1.487 cm3) (p < 0.01). GB emptying function and the effect of Dom on GB emptying in IBS patients and controls are shown in Figures 1 and 2, Table 2.
| Drug | Subjects | 15 min | 30 min | 45 min | 60 min |
| No drug | patients | 25.93 ± 2.06b | 44.54 ± 2.49b | 54.16 ± 1.87b | 65.11 ± 2.10b |
| controls | 32.63 ± 2.34 | 53.79 ± 2.32 | 70.32 ± 1.85 | 80.13 ± 1.81 | |
| Dom 1 | patients | 34.26 ± 1.42a | 58.37 ± 1.77b | 71.22 ± 1.50a | 79.66 ± 1.09e |
| controls | 30.63 ± 2.40 | 50.68 ± 3.05 | 67.72 ± 1.95 | 77.74 ± 1.09 | |
| Dom 2 | patients | 41.10 ± 1.55e | 64.98 ± 1.03b | 74.81 ± 1.45a | 82.74 ± 1.32b |
| controls | 29.63 ± 1.38 | 49.34 ± 2.24 | 63.26 ± 1.69 | 70.95 ± 1.45 |
| Drug Type | 15 min | 30 min | 45 min | 60 min |
| Nil Hypermotility | 26.68 ± 2.83 | 47.61 ± 2.62 | 58.18 ± 2.31 | 69.80 ± 1.87 |
| Type Segmental contraction | 29.20 ± 2.68a | 40.98 ± 2.39b | 49.49 ± 2.51c | 60.96 ± 1.92c |
| Others | 24.42 ± 1.82b | 24.42 ± 1.82b | 48.43 ± 1.64 | 55.43 ± 1.72b |
| Dom 1 Hypermotility | 33.34 ± 2.15 | 62.04 ± 2.11 | 73.99 ± 1.76 | 82.27 ± 1.86 |
| Segmental contraction | 35.11 ± 1.66 | 57.90 ± 1.63 | 69.34 ± 1.87 | 77.45 ± 1.59b |
| Others | 31.34 ± 2.63b | 55.89 ± 2.51 | 68.29 ± 2.03 | 77.64 ± 1.83 |
| Dom 2 Hypermotility | 40.09 ± 2.22 | 66.02 ± 1.91 | 79.69 ± 1.70 | 84.78 ± 1.70 |
| Segmental contraction | 38.87 ± 1.81a | 62.93 ± 1.65b | 74.62 ± 1.64b | 81.38 ± 1.78a |
| Others | 43.91 ± 2.06 | 69.71 ± 1.81b | 77.91 ± 1.55b | 83.01 ± 1.58 |
The present study found that there was a significant abnormality in GB emptying function and an increased fasting and postprandial GBV in IBS patients compared to healthy controls. These measures were also remarkably different among the different subtypes of IBS. Oral Dom treatment improved GB emptying and increased GBEF, and these effects were more remarkable for Dom2 than for Dom1. In healthy controls, oral Dom1, and especially Dom2, decreased GB emptying Dom2; and the decrease at 60 min after the meal reached the level of IBS patients who did not take the drug. This suggests that dysfunction of GB smooth muscle or OS and intestinal smooth muscle is similar in IBS; and that the factors that are inhibited by Dom in healthy patients may be the same as those affected in IBS patients. Sood et al[5] observed that there was no significant difference in GB emptying between patients with predominant diarrhea and those with constipation. This is in contrast to our results, and this difference may result from either (1) variance with sampling or (2) classification of our IBS patients by not only symptoms but also the mechanism of inducing symptoms[10] because the underlying mechanisms may be different in different subtypes[12,13]. In addition, our patients were randomly collected, and the number was limited. Not all subtypes were included, and the number of cases of some subtypes was relatively small. Therefore, the GB emptying function in patients with IBS of different subtypes and the exact effects of Dom on GB emptying in them remain to be determined.
GB emptying is a complex process involving many factors with many components, being controlled by nerves, regulated by hormones[14,15], and influenced directly by the functional conditions of GB and OS. Of these, the most important is the GB contraction, OS relaxation, and coordination of the two. There are α and β cholinergic receptors, cholecystokinin (CCK) receptors, and others[16]in the wall of GB and OS. Immunohistochemical studies have documented the presence of dense concentrations of neuropeptide containing myenteric nerves in the OS[17]. Physiologic studies have confirmed that these peptides exert significant effects on biliary motility. In healthy people, the entry of a fatty meal into the duodenum results in release of CCK, which causes the GB to contract, the OS to relax, and the GB to empty; GBEF can reach 80% or more 60 min after the meal. The mechanism by which GBEF decreases after oral Dom may be via Dom-induced OS contraction or inhibition of relaxation of OS, making OS relaxation weak. Dom antagonism of the β or dopamine receptors in OS blocks the excretion of bile from the biliary duct. In the present study, we did not determine the concentrations of CCK and other neuropeptides in blood and the pressure of OS before and after oral Dom. Also, we do not know if there were changes of CCK release from intestinal mucosa or differences in the number and sensitivity of the receptors, such as β, CCK, etc., in GB and OS[18] because there were abnormal changes in these aspects in IBS patients. In addition, the disorder of gastrointestinal motility was frequent in IBS patients. Since it is known that Dom promotes stomach emptying[7], it is possible that changes in GB emptying occur after oral Dom in our patients. According to reports by Duan et al[19] and Guelrud et al[20] and the results gained in the present study, healthy persons and IBS patients respond differently to Dom, so the effect of stomach emptying on GB emptying function can be excluded. Our main finding is that Dom can strengthen the contraction of weakened GB smooth muscle in IBS patients and at the same time may cause the OS to relax through stimulating dopamine receptors.
The present study demonstrates that IBS is a chronic systematic dysfunctional disease involving all smooth muscles[1] and that its pathogenesis may differ within the subtypes. Oral Dom can significantly improve GB emptying in IBS patients. Our study has revealed a role for abnormal GB emptying function in the pathogenesis of IBS, providing support for the use of Dom clinically in the treatment of IBS.
Original title: China National Journal of New Gastroenterology (1995-1997) renamed World Journal of Gastroenterology (1998-).
S- Editor: Filipodia L- Editor: Jennifer E- Editor: Zhang FF
| 1. | Chen SZ, Lu JW, Jin WK, Zhang Q. Effects of nifedipine in 73 patients with irritable bowel syndrome. Zhonghua Neike Zazhi. 1991;30:111. |
| 2. | Braverman DZ. Gallbladder contraction in patients with irritable bowel syndrome. Isr J Med Sci. 1987;23:181-184. [PubMed] |
| 3. | Thompson WG. A strategy for management of the irritable bowel. Am J Gastroenterol. 1986;81:95-100. [PubMed] |
| 4. | Whorwell PJ, McCallum M, Creed FH, Roberts CT. Non-colonic features of irritable bowel syndrome. Gut. 1986;27:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 340] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Sood GK, Baijal SS, Lahoti D, Broor SL. Abnormal gallbladder function in patients with irritable bowel syndrome. Am J Gastroenterol. 1993;88:1387-1390. [PubMed] |
| 6. | Keshavarziam A, Anagnostides A, Chadwick VS, Fitzpatrick ML. Gallbladder function in the irritable bowel syndrome. J Clin Gastroenterol. 1987;9:366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Koch KL, Stern RM, Stewart WR, Vasey MW. Gastric emptying and gastric myoelectrical activity in patients with diabetic gastroparesis: effect of long-term domperidone treatment. Am J Gastroenterol. 1989;84:1069-1075. [PubMed] |
| 8. | Fisher RS, Rock E, Malmud LS. Cholinergic effects on gallbladder emptying in humans. Gastroenterology. 1985;89:716-722. [PubMed] |
| 9. | Fisher RS; Editorial. Criteria of irritable bowel syndrome for scientific research worked out by national scientific congress on chronic diarrhea. Zhonghua Xiaohua Zazhi. 1987;7:cover 3. |
| 10. | Chen SZ, Liu JY, Zhang Q. Clinical analysis, diagnosis and type divison in 1125 patients with irritable bowel syndrome (IBS) (abstract). Am J Gastroenterol. 1993;88:1569. |
| 11. | Jonderko K, Nowak A, Kasicha-Jonderko A, Sliwi nski Z, Kucio C. Effect of nifedipine on interdigestive gallbladder volume and postprandial gallbladder emptying in man. Dig Dis Sci. 1991;36:1434-1440. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Chen SZ, Jin WK, Pan BR, Zhang Q. Abnormal blood pressure: An important non-gastrointestinal manifestation in patients with the irritable bowel syndrome. Proc R Coll Physician Edinburgh. 1989;19:39-42. |
| 13. | Christopher DL. Motility disorders in the irritable bowel syndrome. Gastroenterol Clin North Am. 1991;20:291-292. |
| 14. | Tierney S, Pitt HA, Lillemoe KD. Physiology and pathophysiology of gallbladder motility. Surg Clin North Am. 1993;73:1267-1290. [PubMed] |
| 15. | Sand J, Tainio H, Nordback I. Peptidergic innervation of human sphincter of Oddi. Dig Dis Sci. 1994;39:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Fiorucci S, Santucci L, Morelli A. 5-hydroxytryptamine 3-receptor antagonist modulates gallbladder emptying and motilin release induced by erythromycin. Dig Dis Sci. 1993;38:2236-2240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Becker JM, Parodi JE. Basic control mechanisms of sphincter of Oddi motor function. Gastrointest Endosc Clin North Am. 1993;3:41-46. |
| 18. | Kellow JE, Miller LJ, Phillips SF, Zinsmeister AR, Charboneau JW. Altered sensitivity of the gallbladder to cholecystokinin octapeptide in irritable bowel syndrome. Am J Physiol. 1987;253:G650-G655. [PubMed] |
| 19. | Duan LP, Zheng ZT, Li YN. [A preliminary study of gallbladder emptying in non-ulcer dyspepsia]. Zhonghua Neike Zazhi. 1994;33:11-14. [PubMed] |
| 20. | Guelrud M, Mendoza S, Rossiter G, Ramirez L, Barkin J. Effect of nifedipine on sphincter of Oddi motor activity: studies in healthy volunteers and patients with biliary dyskinesia. Gastroenterology. 1988;95:1050-1055. [PubMed] |