Copyright
©The Author(s) 2025.
World J Gastroenterol. Mar 14, 2025; 31(10): 100194
Published online Mar 14, 2025. doi: 10.3748/wjg.v31.i10.100194
Published online Mar 14, 2025. doi: 10.3748/wjg.v31.i10.100194
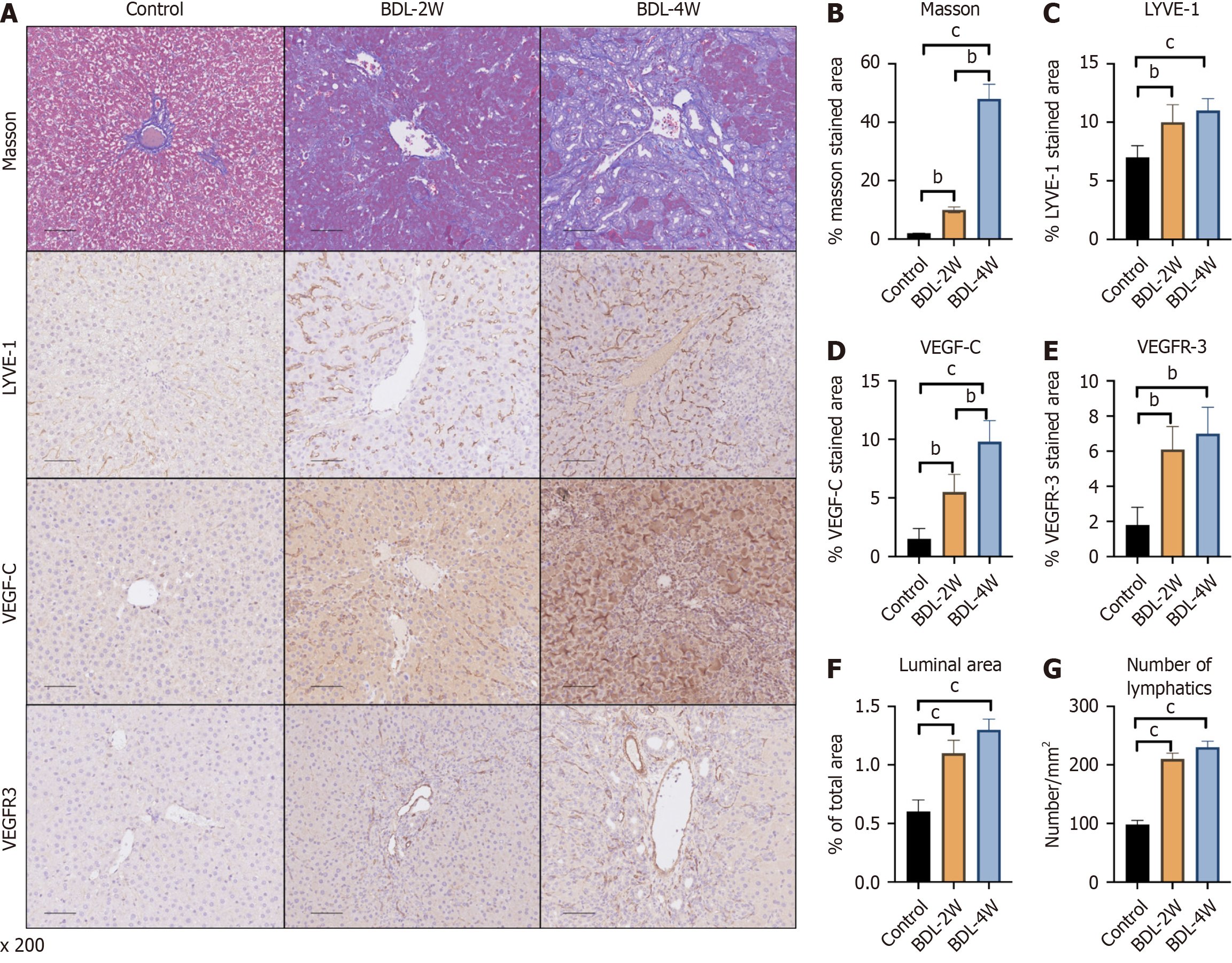
Figure 1 Trends in the number of rat lymphatic vessels at 2 weeks and 4 weeks after bile duct ligation.
A: Representative immunohistochemistry images of Masson’s trichrome, lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1), vascular endothelial growth factor C (VEGF-C) and VEGF receptor 3 (VEGFR-3) staining in the livers of the different groups; B: Quantitative analysis of Masson’s trichrome; C: Quantitative analysis of LYVE-1; D: Quantitative analysis of VEGF-C; E: Quantitative analysis of VEGFR-3 staining; F: Luminal area of lymphatic vessels were also measured; G: The number of lymphatic vessels was also measured. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. BDL: Bile duct ligation; W: Week.
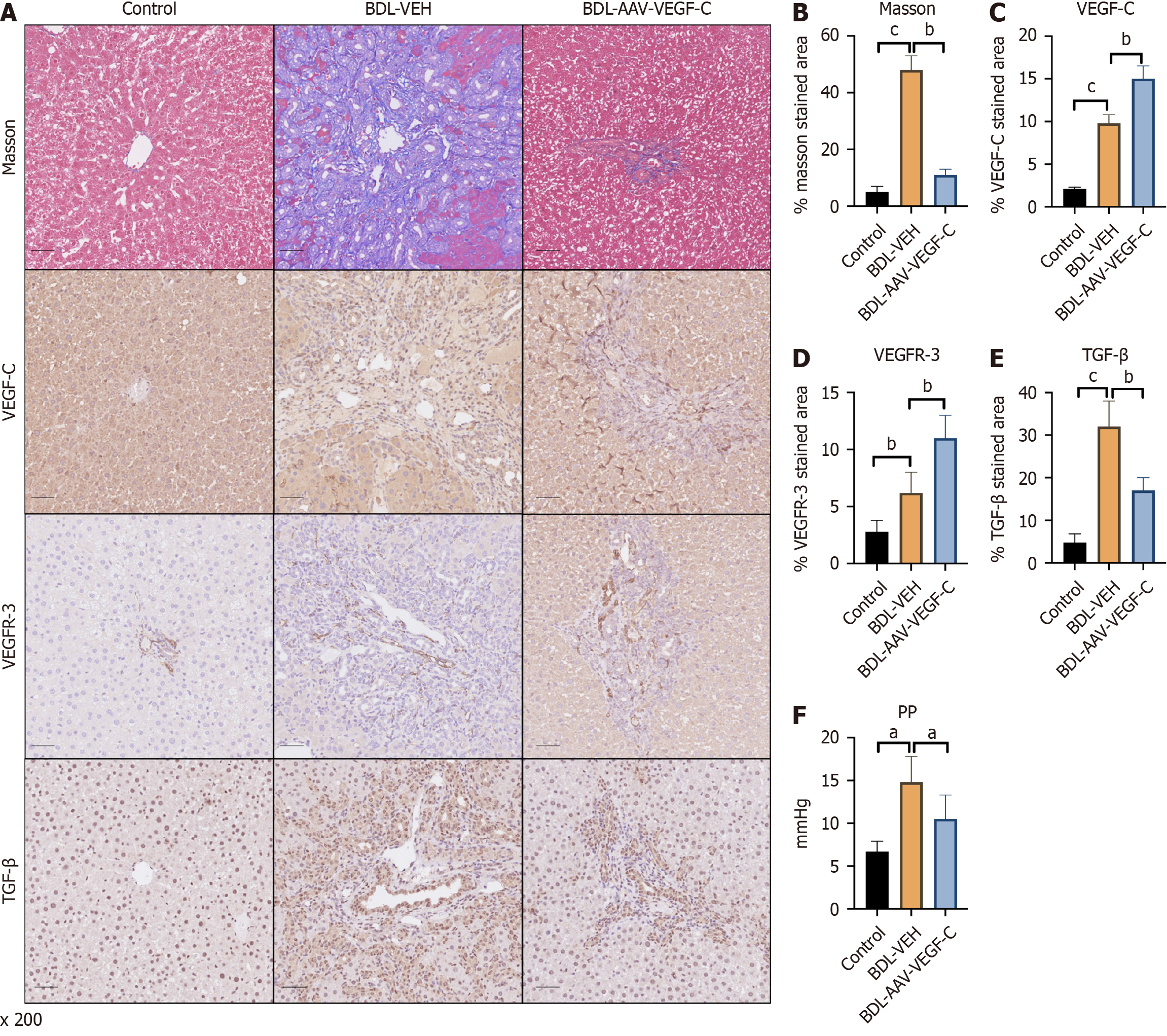
Figure 2 Intervention with adeno-associated virus-vascular endothelial growth factor C relieves liver fibrosis and portal hypertension by increasing the number of lymphatic vessels involved in bile duct ligation.
A: Representative immunohistochemistry images of Masson’s trichrome, virus-vascular endothelial growth factor C (VEGF-C), vascular endothelial growth factor receptor 3 (VEGFR-3) and transforming growth factor beta (TGF-β) staining in the livers of the different groups; Quantitative analysis of B: Masson’s trichrome; C: VEGF-C; D: VEGFR-3; E: TGF-β staining; F: The levels of portal pressure were also measured. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. AAV: Adeno-associated virus; BDL: Bile duct ligation; PP: Portal pressure; TGF-β: Transforming growth factor beta; VEGF-C: Vascular endothelial growth factor C; VEGFR-3: Vascular endothelial growth factor receptor 3; VEH: Vehicle.
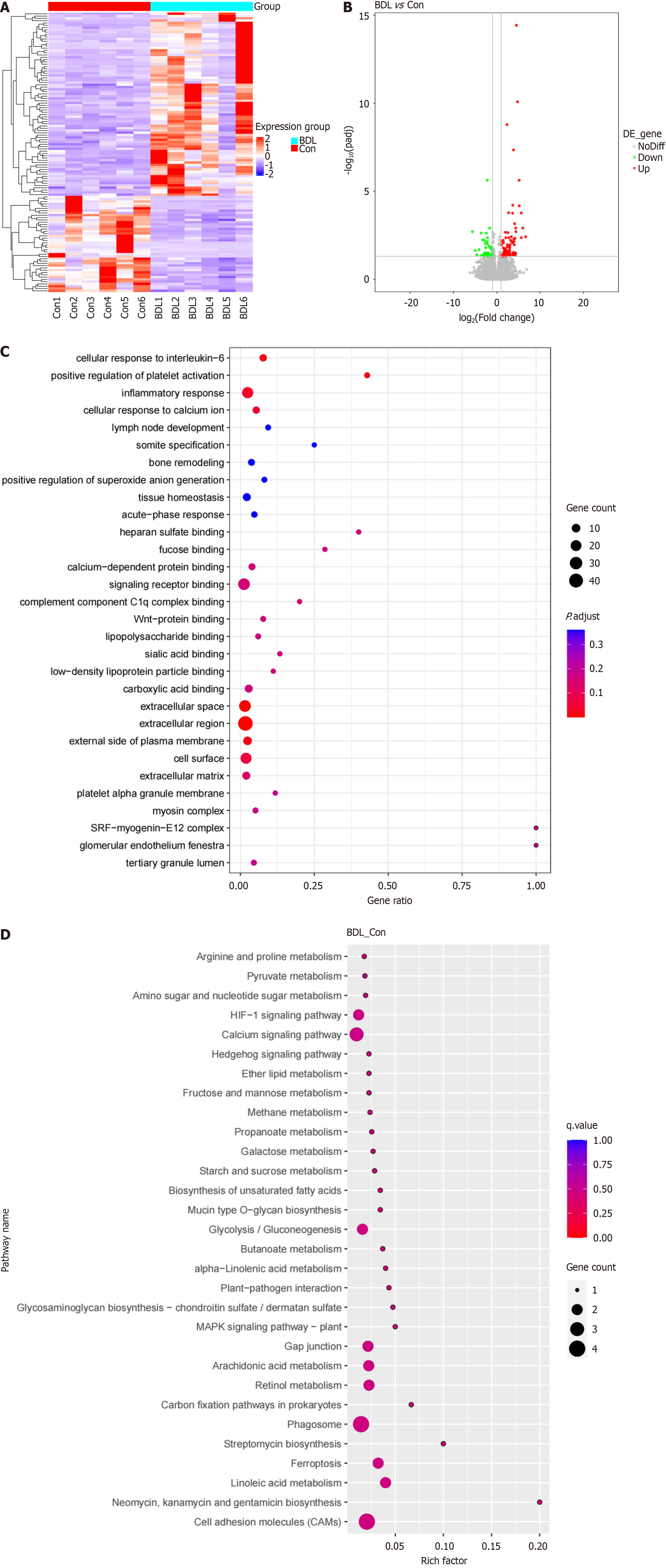
Figure 3 Identification of the differentially expressed genes in the bile duct ligation lymphatic system and related biological processes.
A: Heatmap comparison of differentially expressed genes (DEGs) in the lymphatic system in the bile duct ligation (BDL) and control groups; B: Volcano map of DEG expression in the lymphatic system between the BDL and control groups; C: Bubble plot for gene ontology enrichment of DEGs; D: Bubble plot for Kyoto encyclopaedia of genes and genomes enrichment of DEGs. BDL: Bile duct ligation; Con: Control.
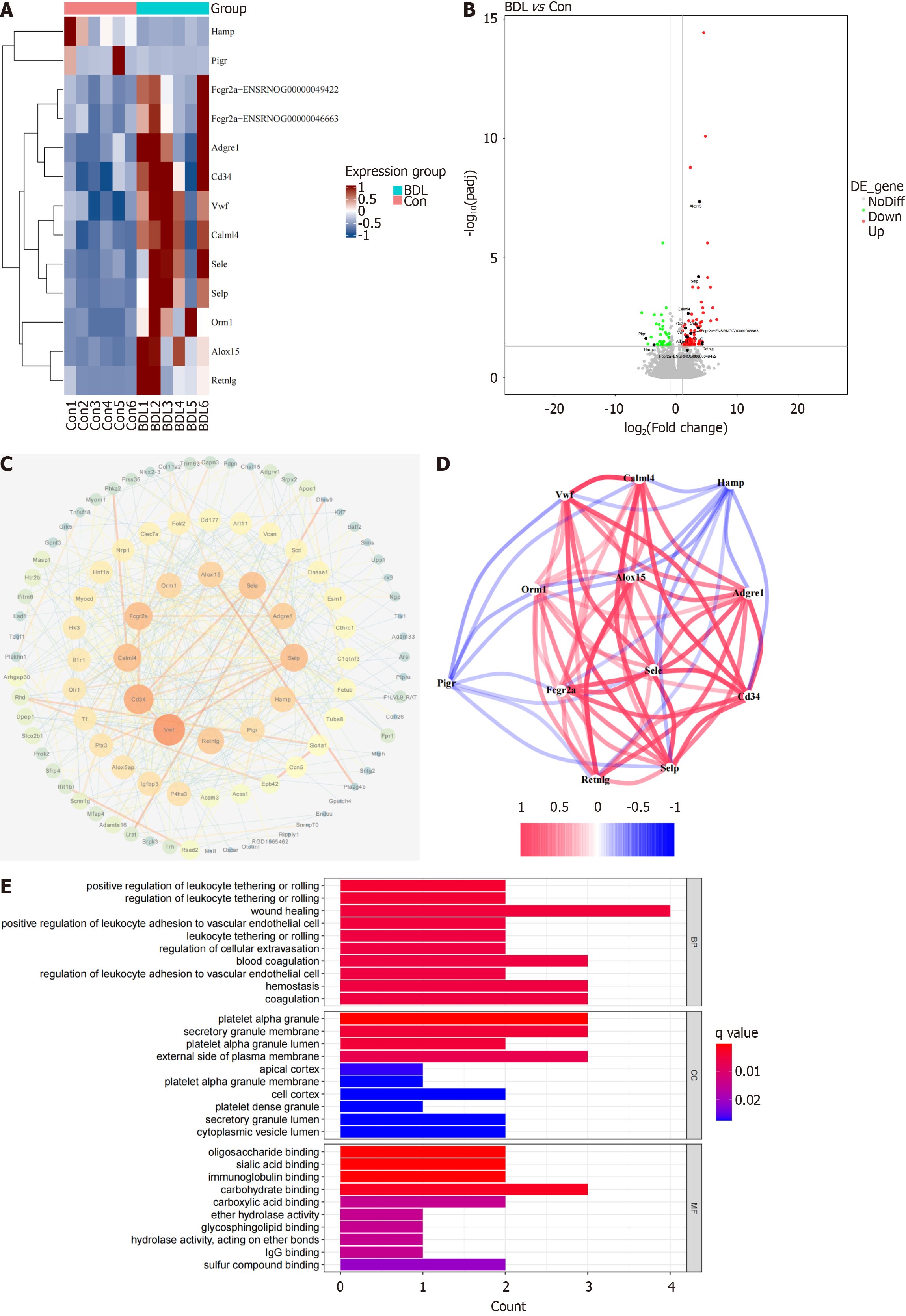
Figure 4 Twelve core differentially expressed genes in the bile duct ligation lymphatic system and their related biological processes.
A: Heatmap of 12 core differentially expressed genes (DEGs) in the lymphatic system between the bile duct ligation (BDL) and control groups; B: Volcano map of core DEGs in the lymphatic system between the BDL and control groups; C: Protein-protein interaction network between the DEGs and the 12 core DEGs; D: Co-expression of these core DEGs; E: Bar plot of the gene ontology enrichment of the core DEGs. BDL: Bile duct ligation; BP: Biological process; CC: Cellular component; Con: Control; MF: Molecular function.
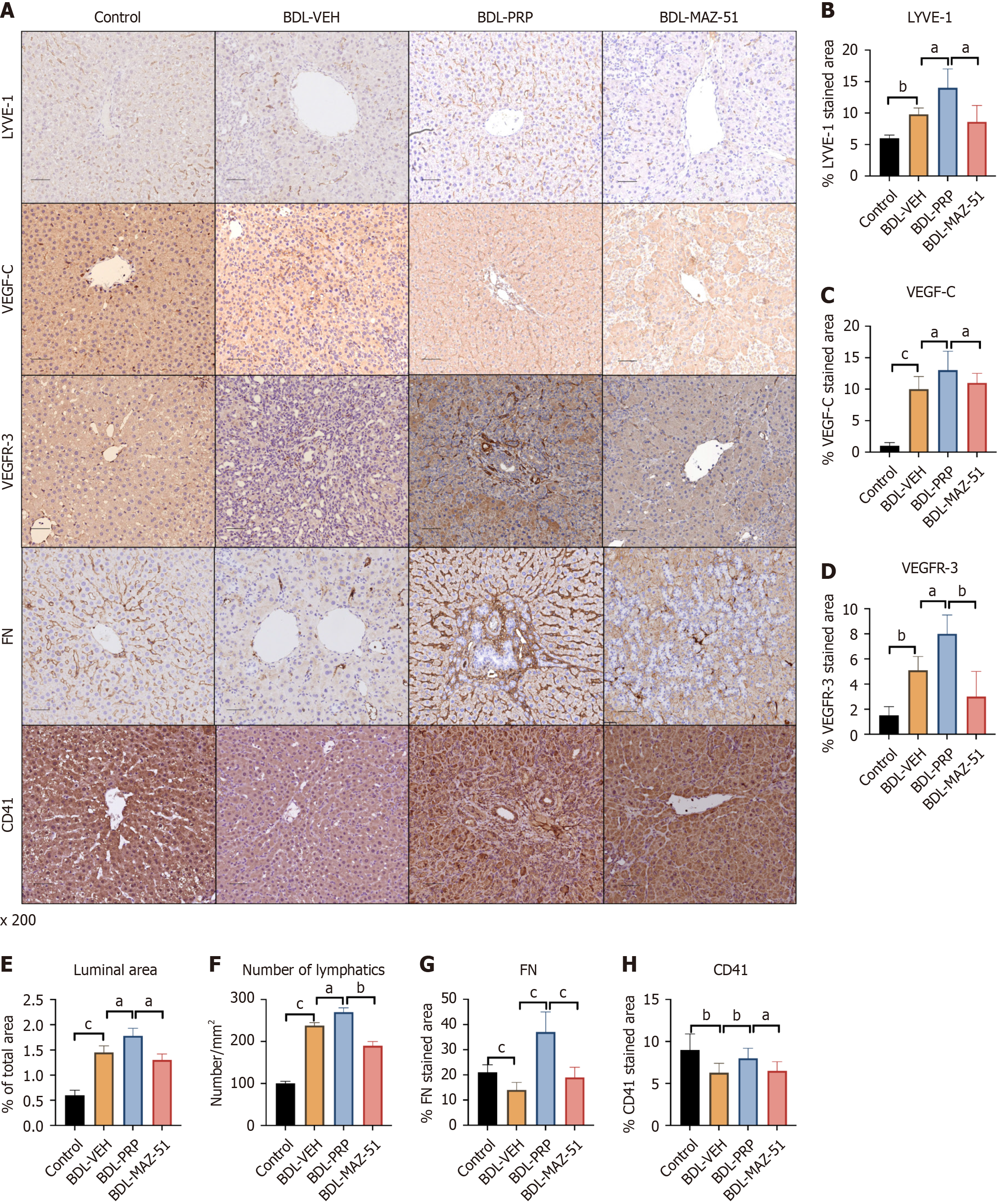
Figure 5 Platelet-rich plasma-induced platelets increase intrahepatic lymphatic vessels via the vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 pathway.
A: Representative immunohistochemistry images of lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1), vascular endothelial growth factor C (VEGF-C) and vascular endothelial growth factor receptor 3 (VEGFR-3), fibronectin (FN) and cluster of differentiation 41 (CD41) in the livers of the different groups; Quantitative analysis of B: LYVE-1; C: VEGF-C; D: VEGFR-3; E: The luminal area; F: The number of lymphatic vessels were also measured; G: FN; H: CD41 expression. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. BDL: Bile duct ligation; PRP: Platelet-rich plasma; VEH: Vehicle.
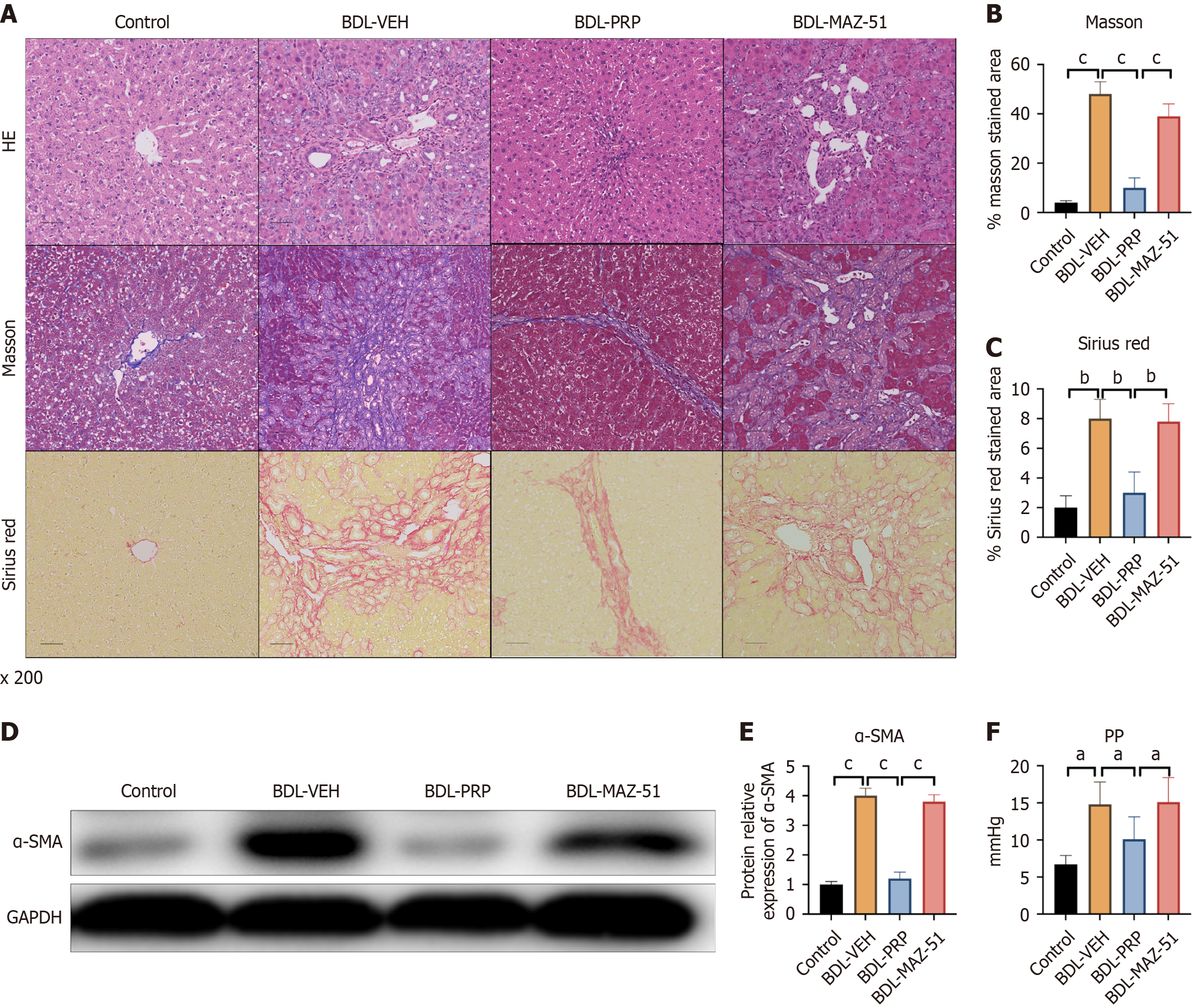
Figure 6 Inhibition of vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 reversed the amelioration of liver fibrosis and portal hypertension in platelet-rich plasma-induced platelets.
A: Representative immunohistochemistry images of hematoxylin and eosin (H&E), Masson’s trichrome, and Sirius red staining in liver samples from the different groups; Quantitative analysis of B: Masson’s trichrome; C: Sirius Red; D: Protein expression of alpha smooth muscle actin (α-SMA) in the different groups; Quantitative analysis of E: α-SMA staining; F: The levels of portal pressure were also measured. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. BDL: Bile duct ligation; GAPDH: Glyceraldehyde-3-phosphate dehydrogenase; PP: Portal pressure; PRP: Platelet-rich plasma; VEH: Vehicle.
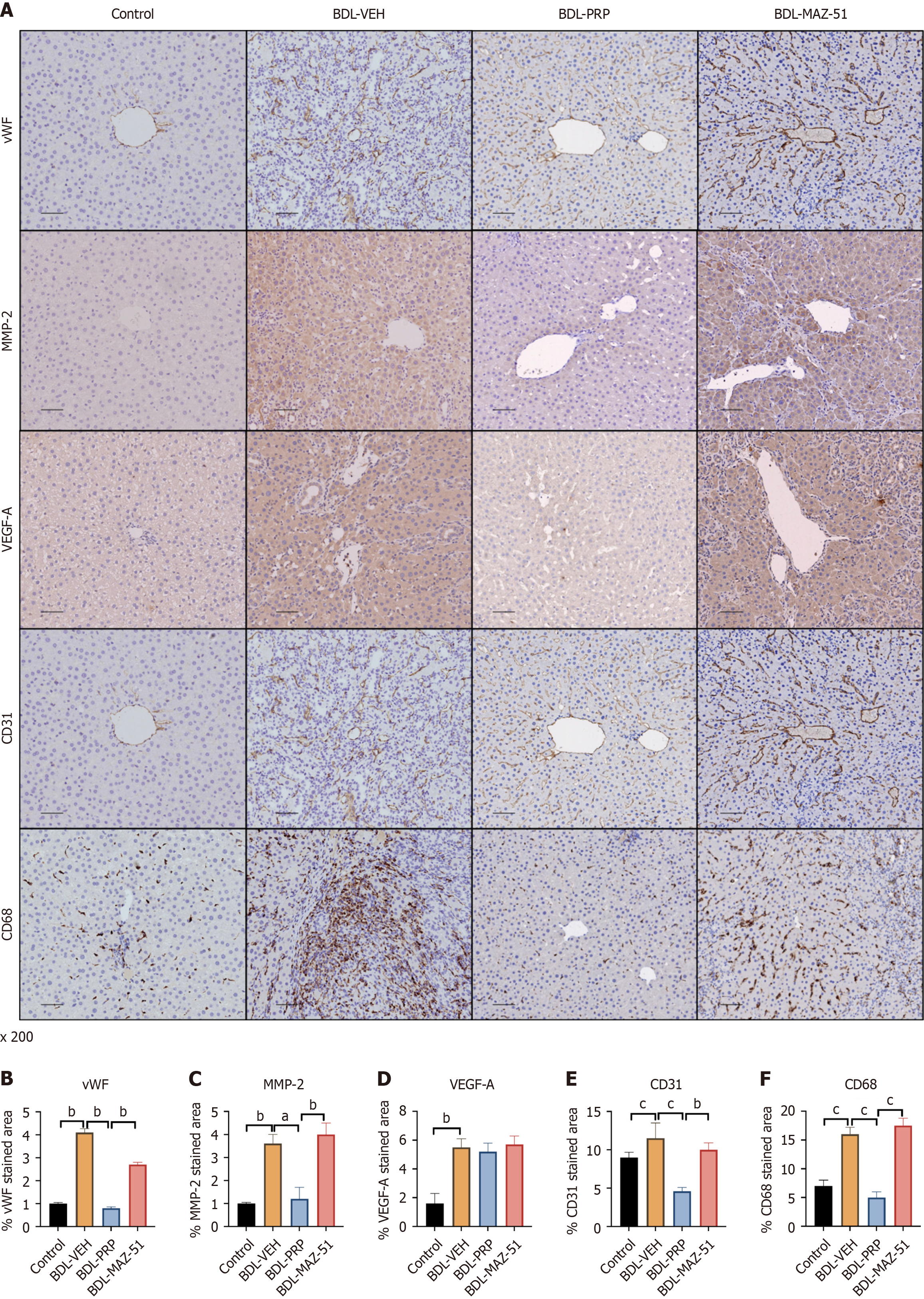
Figure 7 Inhibition of vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 reverses the amelioration of intrahepatic angiogenesis and inflammation by platelet-rich plasma-induced platelets.
A: Representative immunohistochemistry images of von Willebrand factor (vWF), matrix metalloproteinase 2 (MMP2), vascular endothelial growth factor A (VEGF-A), cluster of differentiation 31 (CD31) and CD68 in the livers of different groups; Quantitative analysis of B: vWF; C: MMP2; D: VEGF-A; E: CD31; F: CD68. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. BDL: Bile duct ligation; PRP: Platelet-rich plasma; VEH: Vehicle.
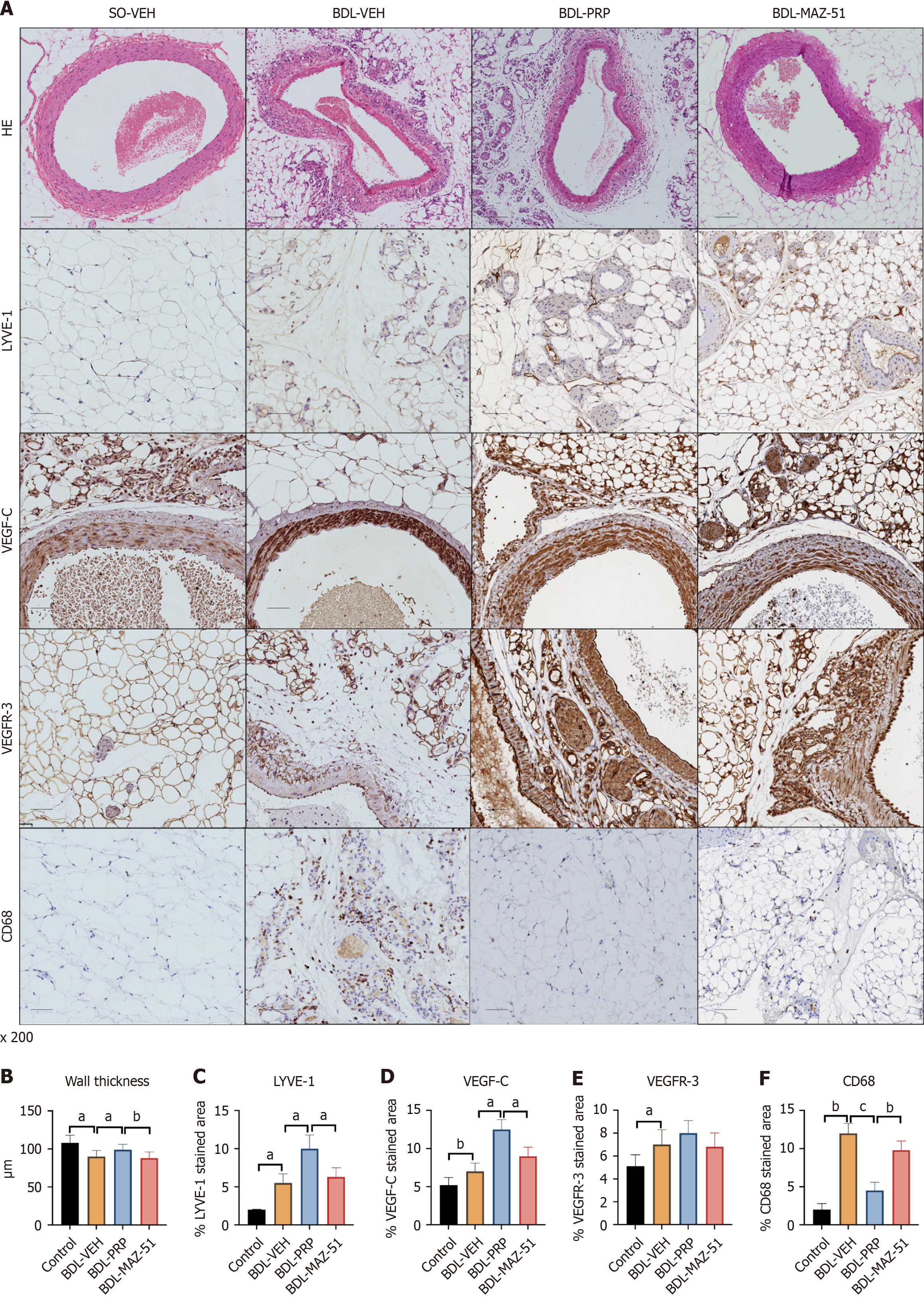
Figure 8 Inhibition of vascular endothelial growth factor C/vascular endothelial growth factor receptor 3 reverses the amelioration of mesenteric angiogenesis and inflammation by platelet-rich plasma-induced platelets.
A: Representative immunohistochemistry images of hematoxylin and eosin, lymphatic vessel endothelial hyaluronan receptor-1 (LYVE-1), vascular endothelial growth factor C (VEGF-C) and vascular endothelial growth factor receptor 3 (VEGFR-3) and cluster of differentiation 68 (CD68) in the mesentery of the different groups; Quantitative analysis of B: Wall thickness; C: LYVE-1; D: VEGF-C; E: VEGFR-3; F: CD68. The data represent the mean ± SD. aP < 0.05. bP < 0.01. cP < 0.001. BDL: Bile duct ligation; PRP: Platelet-rich plasma; SO-VEH: Sham-operated-vehicle; VEH: Vehicle.
- Citation: Chen M, Zhao JB, Wu GB, Wu ZH, Luo GQ, Zhao ZF, Zhang CH, Lin JY, Li HJ, Qi XL, Huo HZ, Tuersun A, Fan Q, Zheng L, Luo M. Platelet activation relieves liver portal hypertension via the lymphatic system though the classical vascular endothelial growth factor receptor 3 signaling pathway. World J Gastroenterol 2025; 31(10): 100194
- URL: https://www.wjgnet.com/1007-9327/full/v31/i10/100194.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i10.100194