Copyright
©The Author(s) 2025.
World J Gastroenterol. Jan 7, 2025; 31(1): 98561
Published online Jan 7, 2025. doi: 10.3748/wjg.v31.i1.98561
Published online Jan 7, 2025. doi: 10.3748/wjg.v31.i1.98561
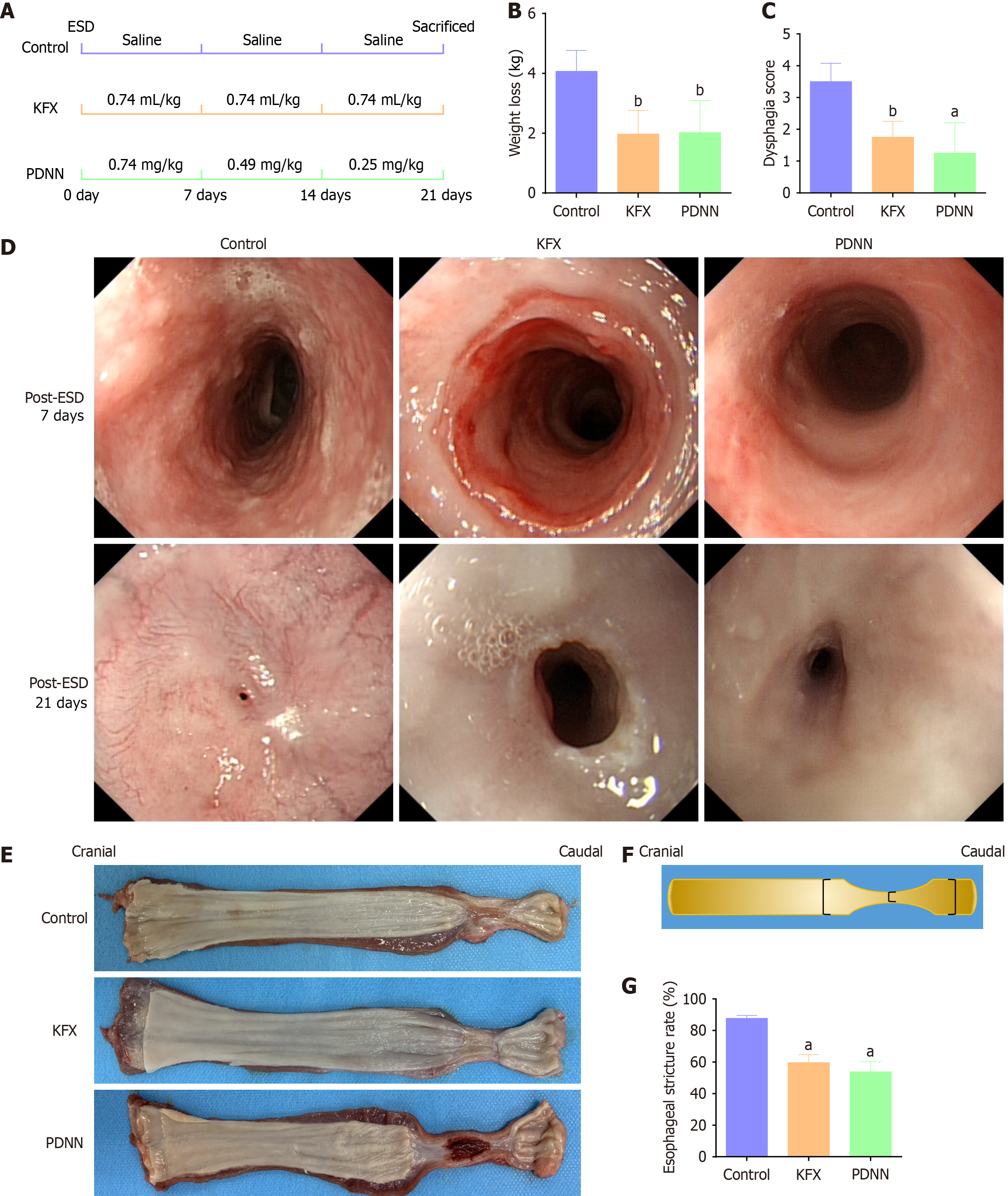
Figure 1 Kangfuxin solution treatment improved the esophageal stricture after full circumferential endoscopic submucosal dissection.
A: The schematic graph shows the design of animal experiments (n = 4); pigs in each group were treated for 21 days with saline, Kangfuxin solution (KFX), and PDNN, respectively; B: The weight loss of pigs in each group; reduction in weight loss was observed post-treatment with KFX and PDNN (n = 4); C: Swallowing difficulty score for pigs in each group on day 21 post- endoscopic submucosal dissection (ESD) (n = 4); after KFX and PDNN treatment, pigs showed improved tolerance to semi-liquid diets compared to the Control group; D: Representative digestive endoscopic images of esophageal artificial ulcers on the 7 and 21 days following full circumferential ESD (n = 4); E: Macroscopic observation of esophageal gross specimens (n = 4); F: Cartoon diagram measuring the length of the short axis at the narrowest part of the artificial esophageal ulcer and adjacent normal mucosa (n = 4); G: The histogram shows the esophageal stricture rate (n = 4). Data are presented as mean ± SE. aP < 0.001 vs the control group, bP < 0.01 vs the control group. ESD: Endoscopic submucosal dissection; KFX: Kangfuxin solution; PDNN: Prednisolone.
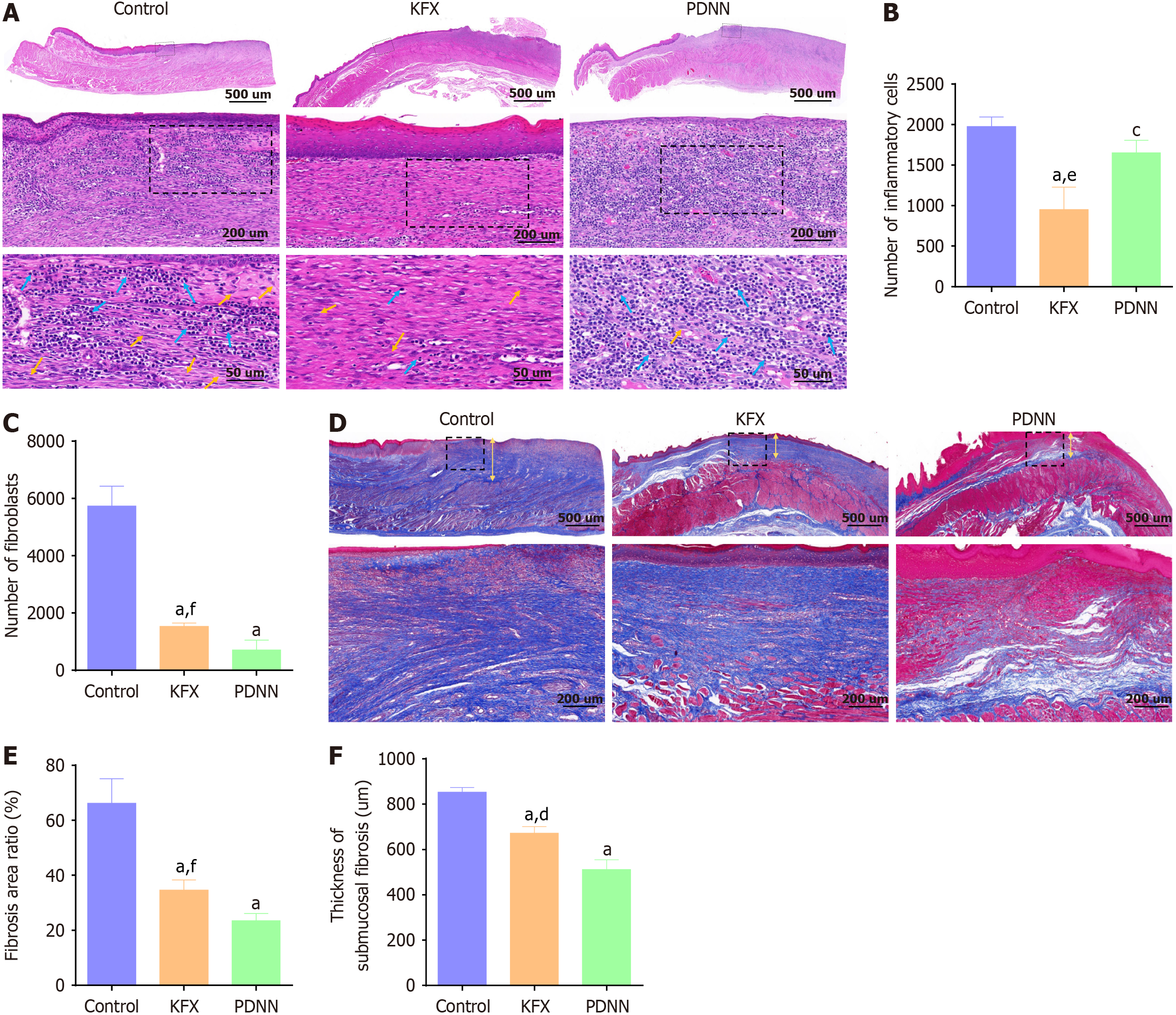
Figure 2 Kangfuxin solution administration improved pathological structure and collagen remodeling of the esophagus after full circumferential endoscopic submucosal dissection.
A: Representative images of hematoxylin-eosin staining of the esophageal tissue, magnification 20 × , 50 × , and 200 × , respectively (n = 4); the blue arrows and the yellow arrows indicate the inflammatory cells and fibroblasts, respectively; B: Quantitation of inflammatory cells in (A) (n = 4); C: Quantitation of fibroblasts in the regenerative tissue beneath the mucosa in (A) (n = 4); the number of inflammatory cells and the presence of fibroblasts in the esophageal submucosa were significantly reduced in both the Kangfuxin solution (KFX) and prednisolone (PDNN) groups; D: Representative images of Masson staining of the esophageal tissue, magnification 20 × and 50 × respectively (n = 4); in contrast to the Control group, both KFX and PDNN groups showed decreased fibrotic areas and more loosely arranged collagen structure; E: Quantitation of the total fibrotic area in (A) (n = 4); F: Quantitation of the newly formed fibrosis thickness beneath the mucosa in (A) (n = 4); the yellow arrow indicates the distance of fibrosis thickness measurement under the mucosa of the esophagus. Data are presented as mean ± SE. aP < 0.001 vs the control group, cP < 0.05 vs the control group, dP < 0.001 vs the PDNN group, eP < 0.01 vs the PDNN group, fP < 0.05 vs the PDNN group. KFX: Kangfuxin solution; PDNN: Prednisolone.
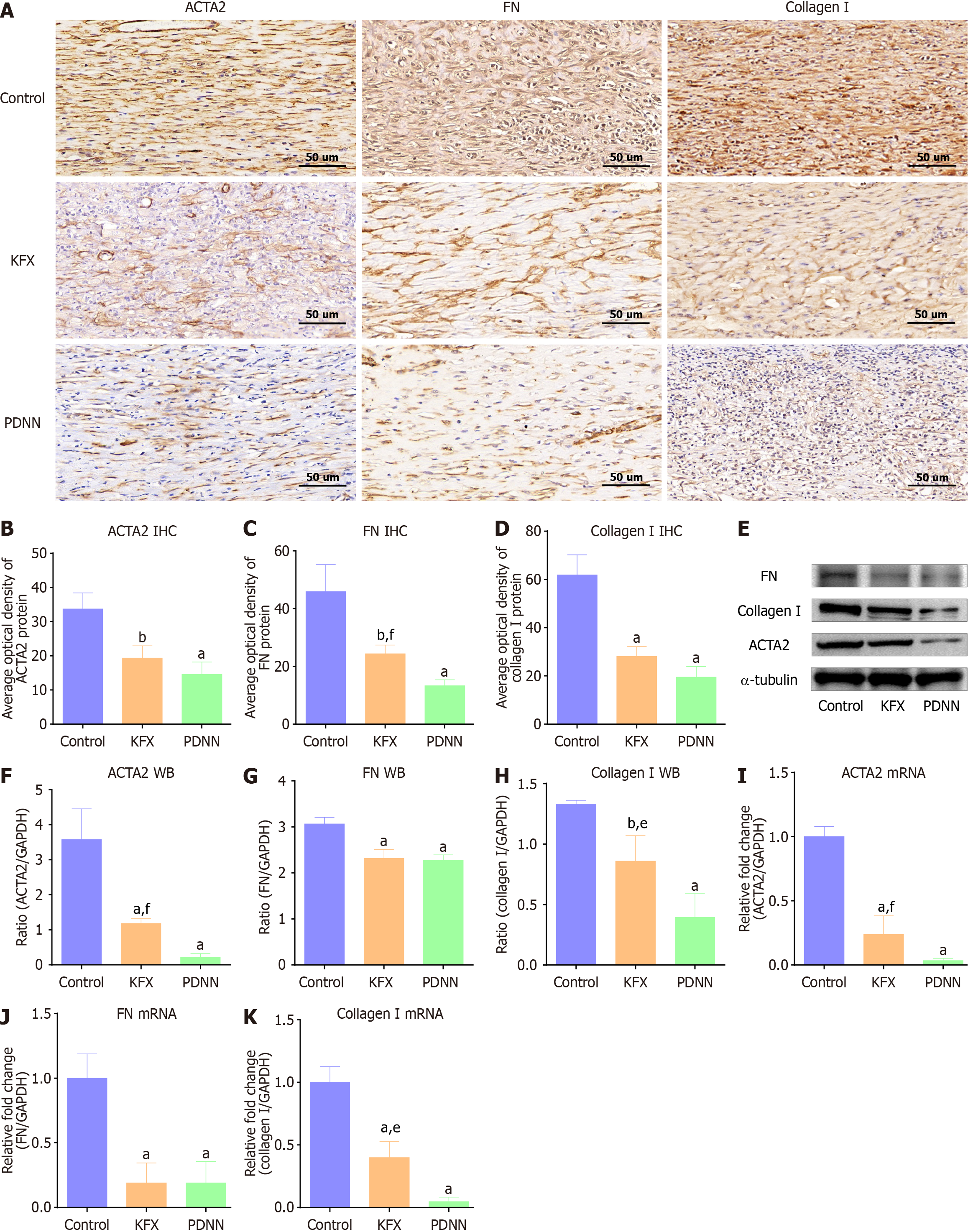
Figure 3 Kangfuxin solution inhibited the excessive deposition of fibrous components in artificial esophageal ulcers.
A: Representative images of immunohistochemical staining to detect Α-smooth muscle actin-2 (ACTA2), fibronectin (FN), and collagen I in the artificial ulcer of esophageal tissue, magnification 200 × (n = 4); B-D: Quantitation of the staining intensity of ACTA2, FN, and collagen I in (A) (n = 4); Kangfuxin solution (KFX) treatment reduced the distribution of ACTA2-positive myofibroblasts and suppressed the expression of extracellular matrix components FN and collagen I; E: The protein levels of ACTA2, FN, and collagen I were determined by western blot; α-tubulin was used as the loading control (n = 4); F-H: Quantitation of relative expression of ACTA2, FN, and collagen I in (E), respectively (n = 4); I-K: The mRNA levels of ACTA2, FN, and collagen I were quantitated by RT-PCR (n = 4); administration of KFX significantly suppressed the protein and gene expression of ACTA2, FN, and collagen I. Data are presented as mean ± SE. aP < 0.001 vs the control group, bP < 0.01 vs the control group, eP < 0.01 vs the PDNN group, fP < 0.05 vs the PDNN group. KFX: Kangfuxin solution; PDNN: Prednisolone; ACTA2: Α-smooth muscle actin-2; FN: Fibronectin; IHC: Immunohistochemistry; WB: Western blotting.
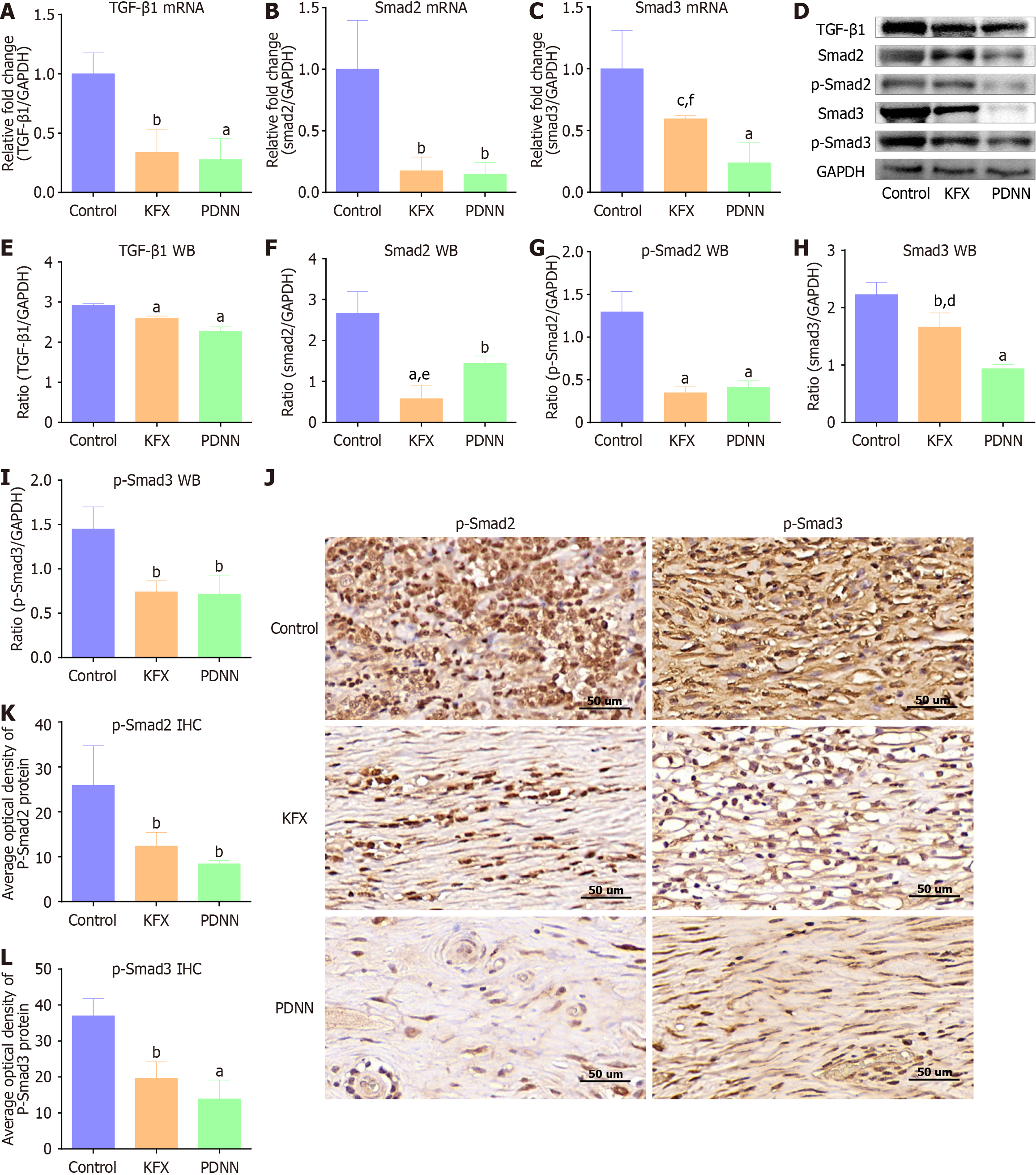
Figure 4 Kangfuxin solution suppressed upregulation of TGF-β1/Smads signaling in the artificial ulcer tissue of the esophagus.
A-C: Relative expression of transforming growth factor β1 (TGF-β1), Smad2, and Smad3 mRNA was determined by RT-PCR (n = 4); D: Western blotting to detect the protein expression of TGF-β1, Smad2, p-Smad2, Smad3, and p-Smad3 in each group (n = 4); E-I: Quantitation of proteins relative expression in D (n = 4); compared to the control group, the expression of TGF-β1, Smad2, and Smad3 was suppressed in both the Kangfuxin solution and prednisolone groups; J: Representative images of immunohistochemical staining of p-Smad2 and p-Smad3, magnification, 200 × (n = 4); K and L: The quantitation of relative expression of p-Smad2 and p-Smad3 in J (n = 4). Data are presented as mean ± SE. aP < 0.001 vs the control group, bP < 0.01 vs the control group, cP < 0.05 vs the control group, dP < 0.001 vs the PDNN group, eP < 0.01 vs the PDNN group. KFX: Kangfuxin solution; PDNN: Prednisolone; TGF-β1: Transforming growth factor β1; WB: Western blotting.
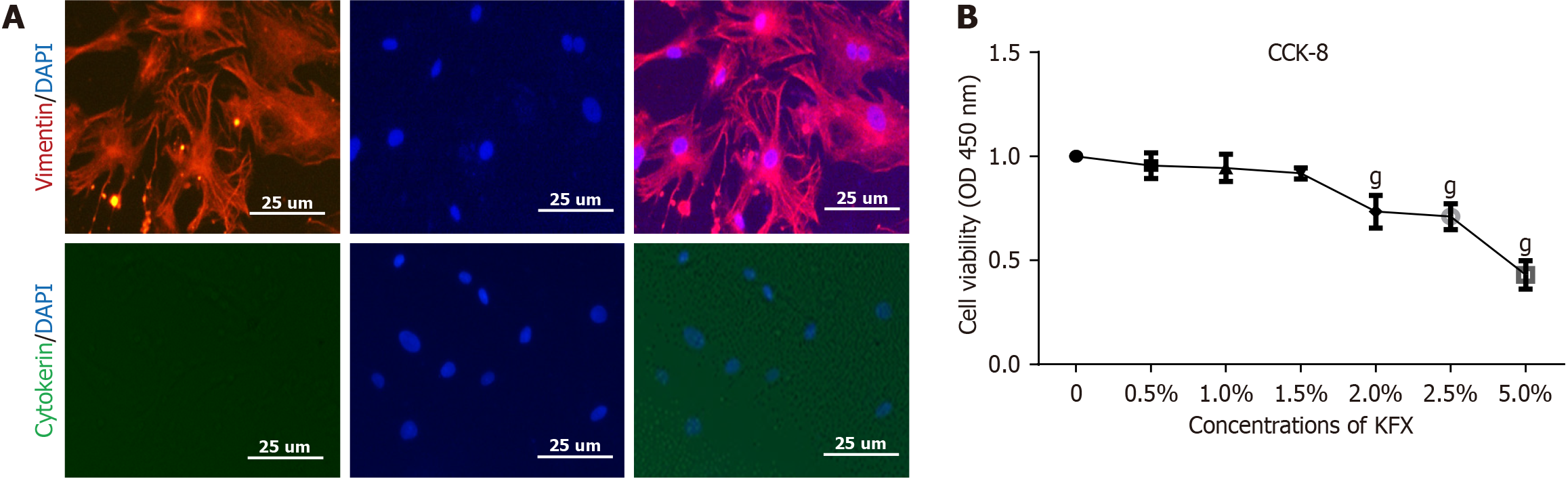
Figure 5 Phenotyping of isolated primary esophageal cells and dose determination of Kangfuxin solution.
A: Representative images of immunofluorescence staining of vimentin and cytokeratin, magnification 400 ×; primary cells exhibited specific expression of vimentin while showing minimal expression of cytokeratin protein; B: The proliferation rate of primary esophageal fibroblasts after stimulation with different concentrations of Kangfuxin solution using the CCK-8 assay. Data are presented as mean ± SE. gP < 0.001 vs the zero tube.
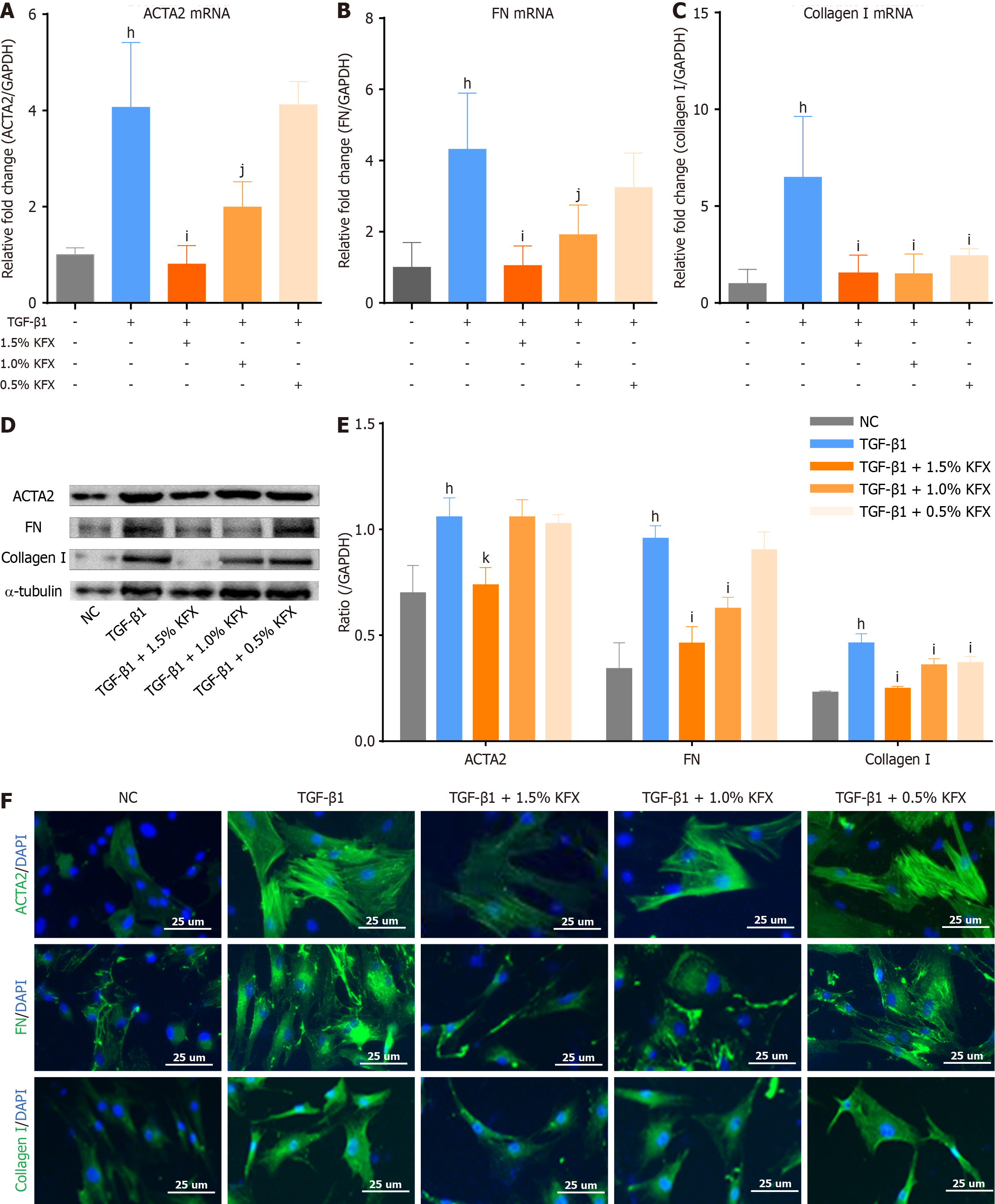
Figure 6 Kangfuxin solution inhibited the excessive fibrotic activity in primary esophageal fibroblast.
A-C: The expression levels ofΑ-smooth muscle actin-2 (ACTA2), fibronectin (FN), and Collagen Ⅰ mRNA were determined by RT-PCR; D: Western blot detected the protein expression of ACTA2, FN, and collagen Ⅰ in primary esophageal fibroblasts (pEsF); E: Quantitation of relative expression of fibrosis protein in (D); Kangfuxin solution intervention dose-dependently suppressed the expression of ACTA2, FN, and collagen Ⅰ in pEsF; F: Representative images of immunofluorescence staining of ACTA2, FN, and collagen Ⅰ in the pEsF, magnification, 400 ×. Data are presented as mean ± SE. hP < 0.001 vs the negative control group, iP < 0.001 vs the TGF-β1 group, jP < 0.01 vs the TGF-β1 group, kP < 0.05 vs the TGF-β1 group. NC: Negative control group; KFX: Kangfuxin solution; TGF-β1: Transforming growth factor β1; ACTA2: Α-smooth muscle actin-2; FN: Fibronectin; IHC: Immunohistochemistry; WB: Western blotting.
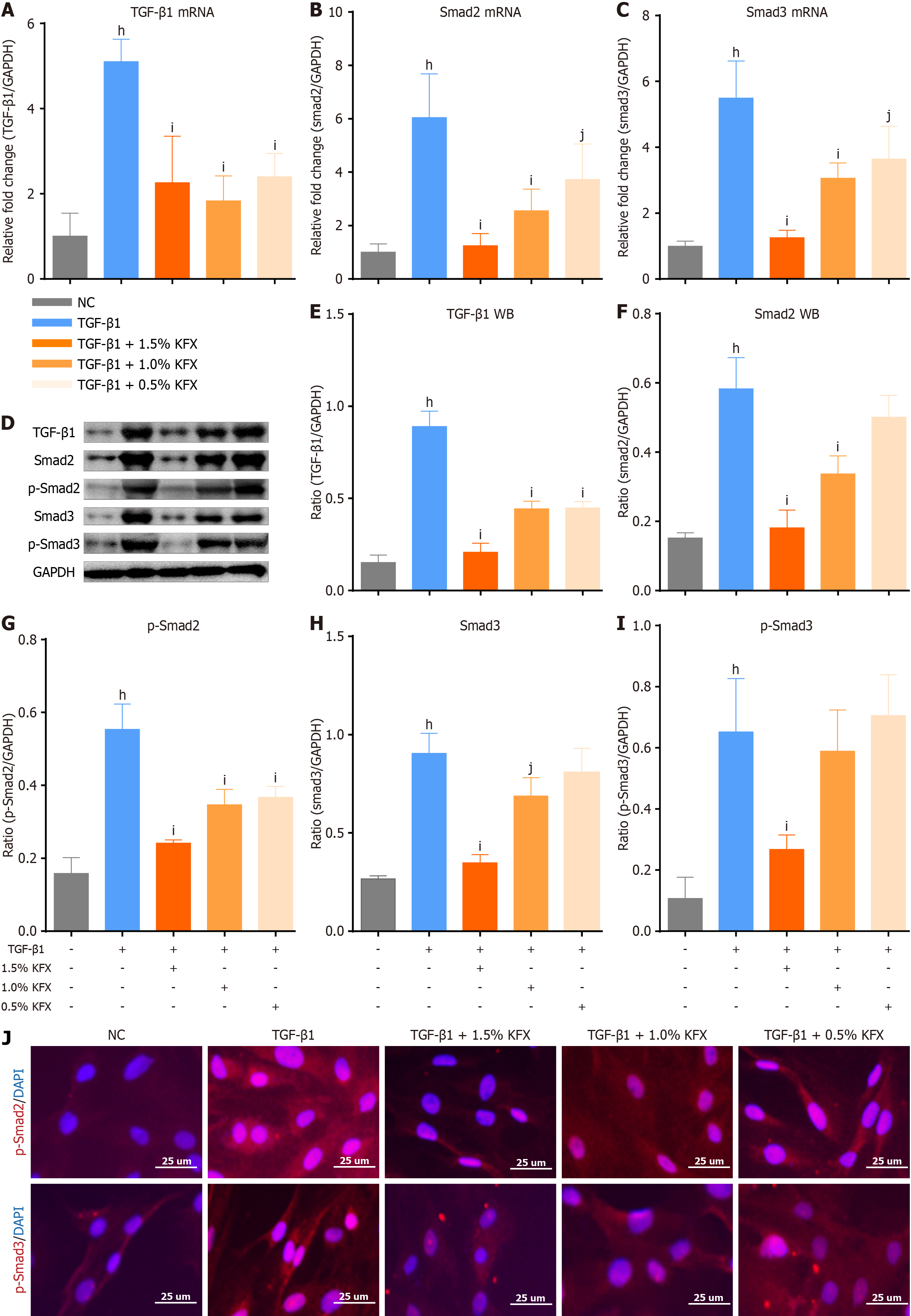
Figure 7 Kangfuxin solution inhibited upregulation of TGF-β1/Smads signaling in primary esophageal fibroblast.
A-C: RT-PCR to detect gene transcription level of Transforming growth factor β1 (TGF-β1), Smad2, and Smad3; D: The western boltting determined the protein expression of TGF-β1, Smad2/3, and p-Smad2/3; E-I: Quantitation of proteins expression in D; compared to the TGF-β1 group, KFX significantly downregulated endogenous p-Smad2/3 expression; J: Representative images of immunofluorescence staining of p-Smad2 and p-Smad3, magnification, 400 ×. Data are presented as mean ± SE. hP < 0.001 vs the negative control group, iP < 0.001 vs the TGF-β1 group, jP < 0.01 vs the TGF-β1 group. NC: Negative control group; KFX: Kangfuxin solution; TGF-β1: Transforming growth factor β1; WB: Western blotting.
- Citation: Zhou X, Ma D, He YX, Jin J, Wang HL, Wang YF, Yang F, Liu JQ, Chen J, Li Z. Kangfuxin solution alleviates esophageal stenosis after endoscopic submucosal dissection: A natural ingredient strategy. World J Gastroenterol 2025; 31(1): 98561
- URL: https://www.wjgnet.com/1007-9327/full/v31/i1/98561.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i1.98561