Copyright
©The Author(s) 2024.
World J Gastroenterol. Mar 28, 2024; 30(12): 1663-1669
Published online Mar 28, 2024. doi: 10.3748/wjg.v30.i12.1663
Published online Mar 28, 2024. doi: 10.3748/wjg.v30.i12.1663
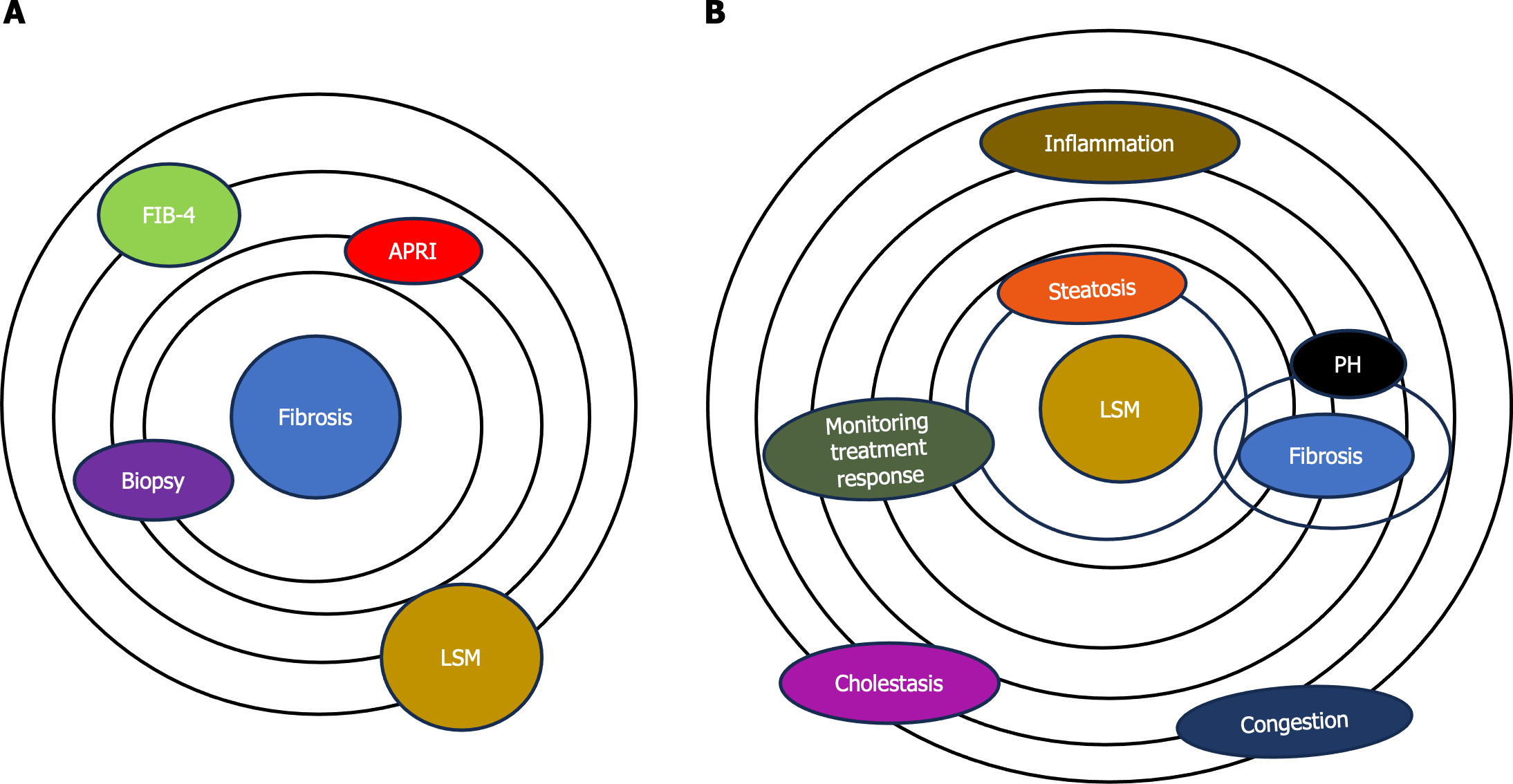
Figure 1 Role of elastography in assessing liver tissue health.
A: Model of assessment of fibrosis. Elastography, once primarily associated with fibrosis assessment (biopsy, different noninvasive scores like fibrosis index based on 4 factors, aspartate aminotransferase-to-platelet index, etc); B: Model of assessment of liver stiffness. Now, elastography has evolved into a versatile method offering assessment of the mechanical properties and dynamic nature of liver tissues such as the quantification of liver steatosis by providing a noninvasive means for evaluation of fat content and the detection of inflammatory changes within liver tissues. Elastography may provide valuable insights into portal hypertension and monitor responses to therapeutic interventions. There are some confounding factors (cholestasis and heart congestion) that can contribute to increasing the liver stiffness. LSM: Liver stiffness measurement; FIB-4: Fibrosis index based on 4 factors; APRI: Aminotransferase-to-platelet index; PH: Portal hypertension.
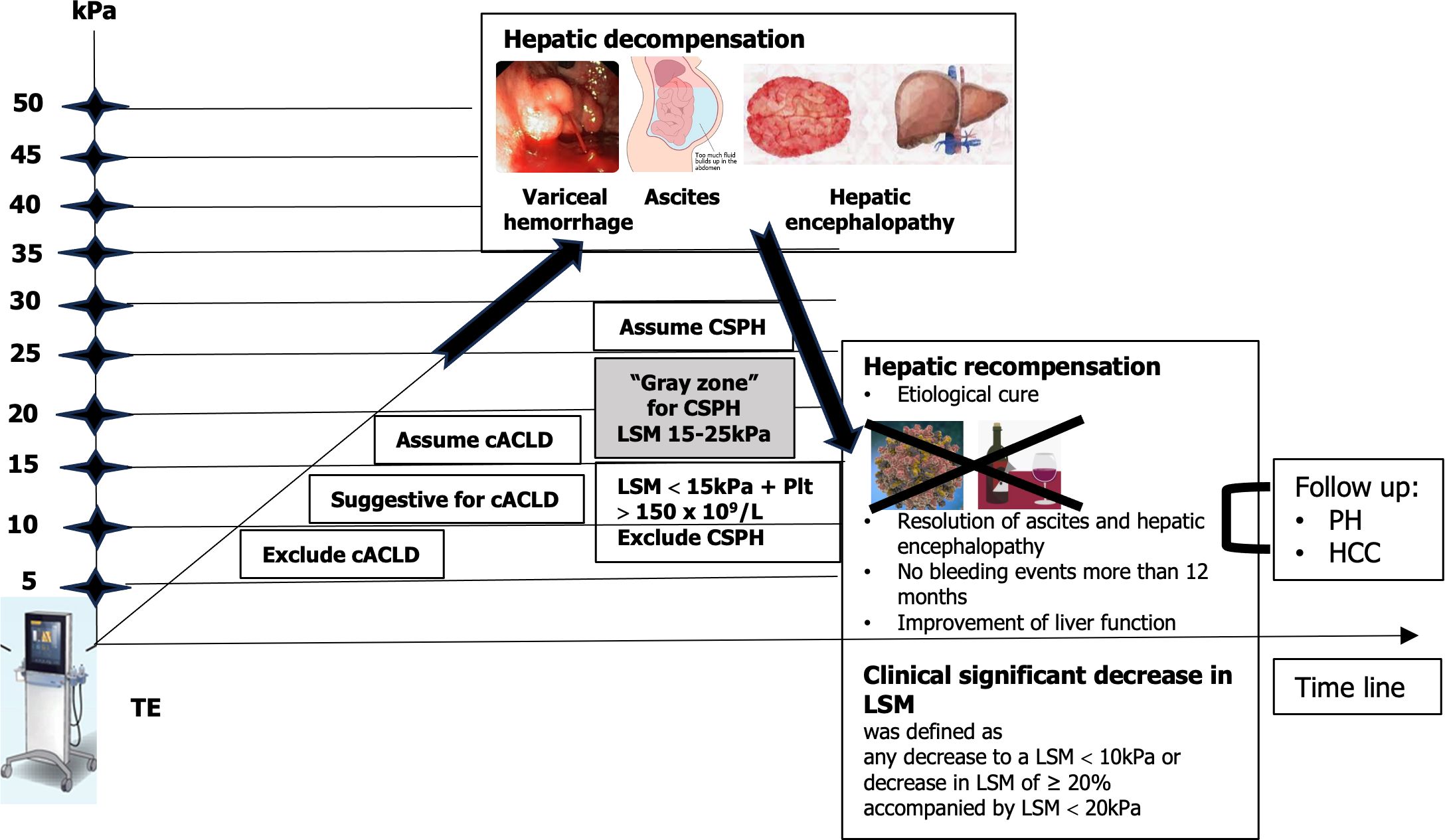
Figure 2 Use of noninvasive tests according to the rule of 5 to determine compensated advanced chronic liver disease and clinically significant portal hypertension.
Dynamic use of noninvasive tests for assessment of hepatic decompensation or recompensation. Patients having a liver stiffness measurement (LSM) < 10 kPa rules out compensated advanced chronic liver disease (cACLD) in the absence of other clinical/imaging signs. LSM values between 10 kPa and 15 kPa are suggestive of cACLD, and LSM ≤ 15 kPa plus platelets ≥ 150 × 109/L rule out clinically significant portal hypertension (CSPH) in the majority of etiologies. LSM measured by transient elastography (TE) > 15 kPa are considered as a high likelihood of cACLD in all etiologies. Patients with intermediate values of LSM between 15 kPa and 25 kPa are in a “gray zone” of CSPH. The best cutoff to determine the presence of CSPH was an LSM ≥ 25 kPa (specificity and positive predictive value > 90%) in alcoholic liver disease, chronic hepatitis B, chronic hepatitis C, and non-obese patients with nonalcoholic steatohepatitis. Hepatic recompensation includes all of the following criteria: Suppression or removal of the underlying etiology of cirrhosis; Resolution of ascites and hepatic encephalopathy after discontinuation of diuretics and prophylactic therapies; Absence of variceal bleeding for 12 months; Sustained improvement of biochemical liver function, assessed by serum albumin, bilirubin, and international normalized ratio[13]. LSM: Liver stiffness measurement; HCC: Hepatocellular carcinoma; PH: Portal hypertension; TE: Transient elastography.
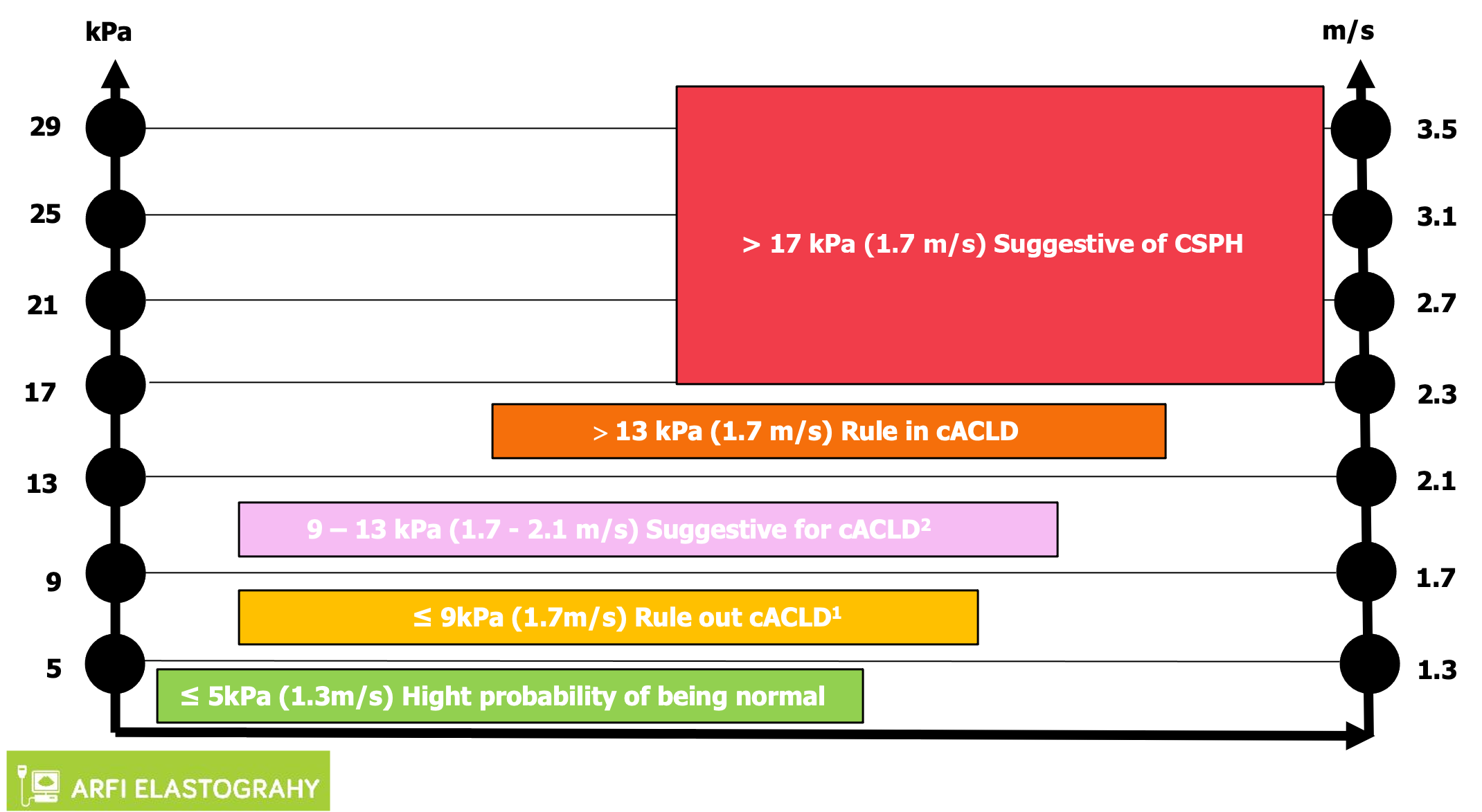
Figure 3 Interpretation of liver stiffness value with acoustic radiation force impulse techniques.
Based on some published studies, the consensus panel Baveno VII proposed a vendor-neutral “rule of 4” (5, 9, 13, and 17 kPa) for the acoustic radiation force impulse techniques for viral etiologies and nonalcoholic fatty liver disease, liver stiffness of 5 kPa (1.3 m/sec) or less has a high probability of being normal. Values greater than 13 kPa (2.1 m/sec) are highly suggestive of compensated advanced chronic liver disease (cACLD). There is a probability of clinically significant portal hypertension with liver stiffness values greater than 17 kPa (2.4 m/sec), but additional patient testing may be required. In some patients with nonalcoholic fatty liver disease, the cutoff values for cACLD may be lower and follow-up or additional testing in those with values between 7 kPa and 9 kPa is recommended[10]. For other causes such as alcoholic hepatitis, primary biliary cirrhosis, Wilson’s disease, autoimmune hepatitis, sclerosing cholangitis, and drug-induced liver disease, there is insufficient data to make a conclusion. 1Liver stiffness less than 9 kPa (1.7 m/sec), in the absence of other known clinical signs, rules out compensated advanced chronic liver disease (cACLD). 2Values between 9 kPa (1.7 m/sec) and 13 kPa (2.1 m/sec) are suggestive of compensated advanced chronic liver disease but may need further testing for confirmation. cACLD: Compensated advanced chronic liver disease; CSPH: Clinically significant portal hypertension.
- Citation: Peltec A, Sporea I. Multiparametric ultrasound as a new concept of assessment of liver tissue damage. World J Gastroenterol 2024; 30(12): 1663-1669
- URL: https://www.wjgnet.com/1007-9327/full/v30/i12/1663.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i12.1663