Copyright
©The Author(s) 2023.
World J Gastroenterol. Feb 7, 2023; 29(5): 825-833
Published online Feb 7, 2023. doi: 10.3748/wjg.v29.i5.825
Published online Feb 7, 2023. doi: 10.3748/wjg.v29.i5.825
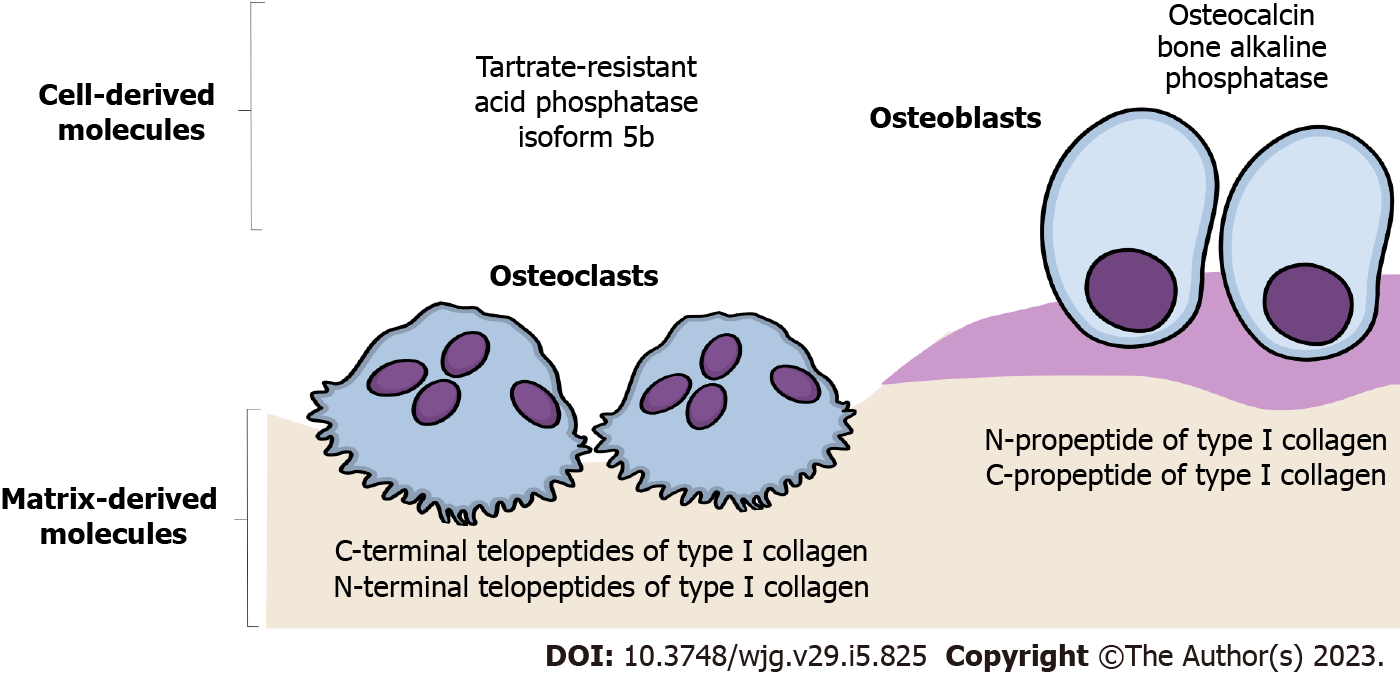
Figure 1 Schematic representation of the most frequently analyzed bone turnover markers.
The emphasis is placed on the difference between bone turnover markers released by catabolic osteoclast activity (bone resorption markers) and anabolic osteoblast activity (bone formation markers).
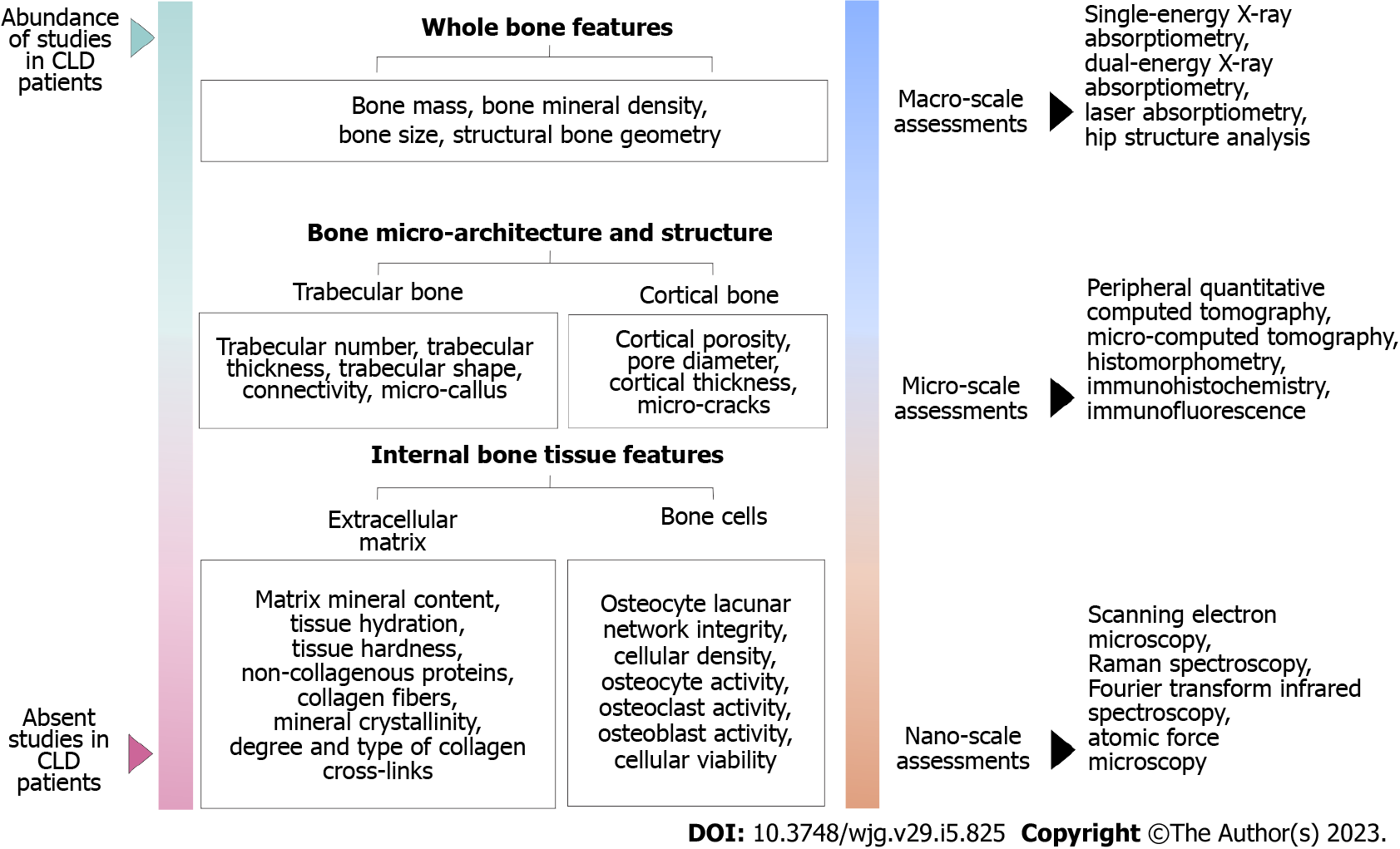
Figure 2 Multiscale approach in the assessment of bone strength determinants.
The importance of the various bone properties that contributes to increased bone fragility, and up-to-date methodologies are used to assess these bone strength determinants. The emphasis is placed on the difference between factors that were previously assessed and those factors that require further investigation in patients with chronic liver disease. CLD: Chronic liver disease.
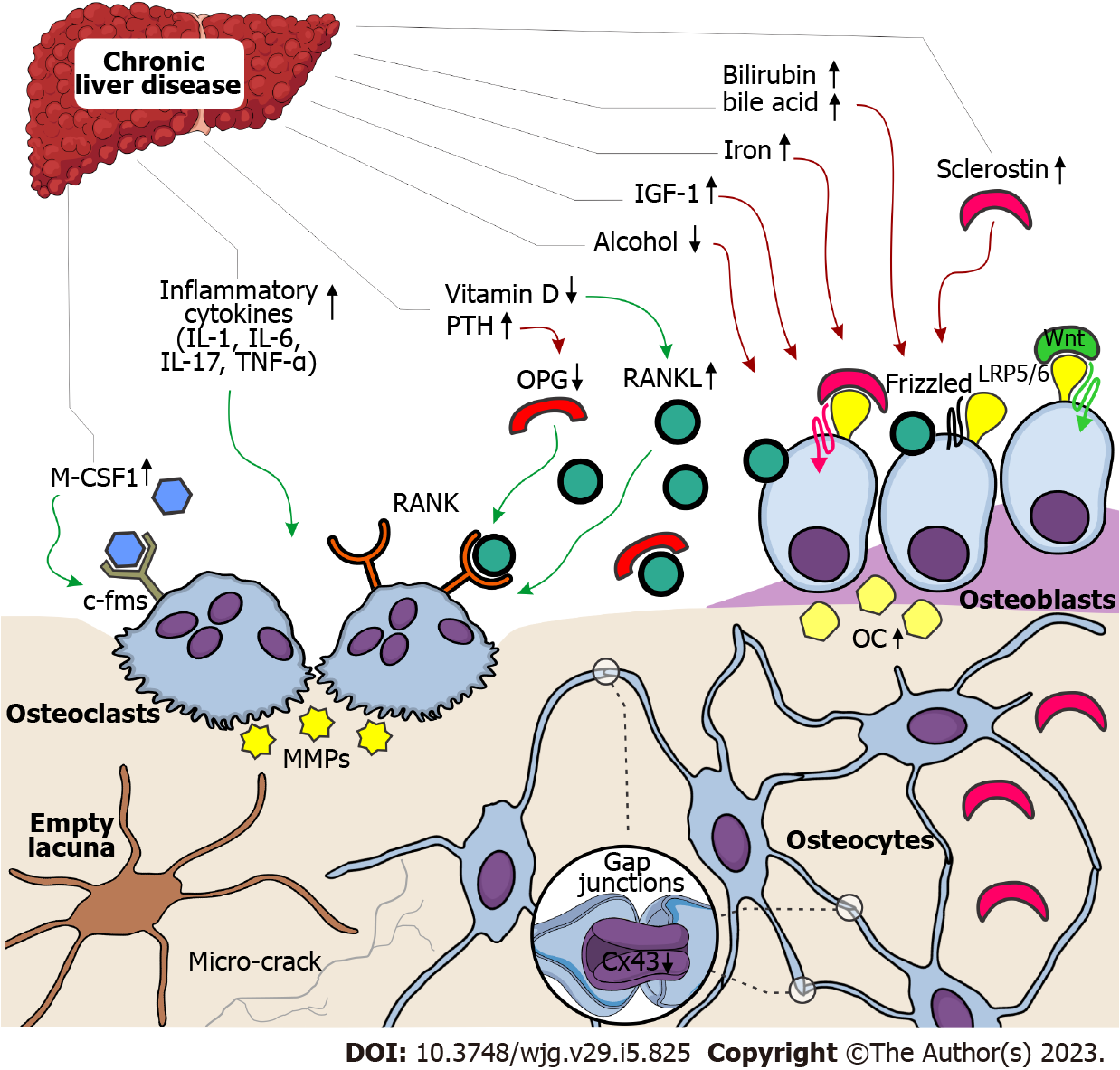
Figure 3 Schematic representation of possible pathophysiological mechanisms leading to bone loss in chronic liver disease patients.
The role of multiple factors leading to bone loss and osteoporosis in individuals with chronic liver disease places an emphasis on the difference between factors that cause osteoblast dysfunction (reduced bone formation) and factors that stimulate osteoclast activity (increased bone resorption). Green arrows indicate an activating effect, while red arrows indicate a deactivating effect. c-fms: Colony-stimulating factor-1 receptor; Cx43: Connexin 43; IGF-1: Insulin-like growth factor 1; IL: Interleukin; LRP5/6: Low-density lipoprotein receptor-related protein 5/6; M-CSF1: Macrophage colony-stimulating factor 1; MMPs: Matrix metalloproteinases; OC: Osteocalcin; OPG: Osteoprotegerin; PTH: Parathyroid hormone; RANK: Receptor activator for nuclear factor kappa B; RANKL: Receptor activator for nuclear factor kappa B ligand; TNF: Tumor necrosis factor.
- Citation: Jadzic J, Djonic D. Bone loss in chronic liver diseases: Could healthy liver be a requirement for good bone health? World J Gastroenterol 2023; 29(5): 825-833
- URL: https://www.wjgnet.com/1007-9327/full/v29/i5/825.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i5.825