Copyright
©The Author(s) 2023.
World J Gastroenterol. Jun 7, 2023; 29(21): 3257-3268
Published online Jun 7, 2023. doi: 10.3748/wjg.v29.i21.3257
Published online Jun 7, 2023. doi: 10.3748/wjg.v29.i21.3257
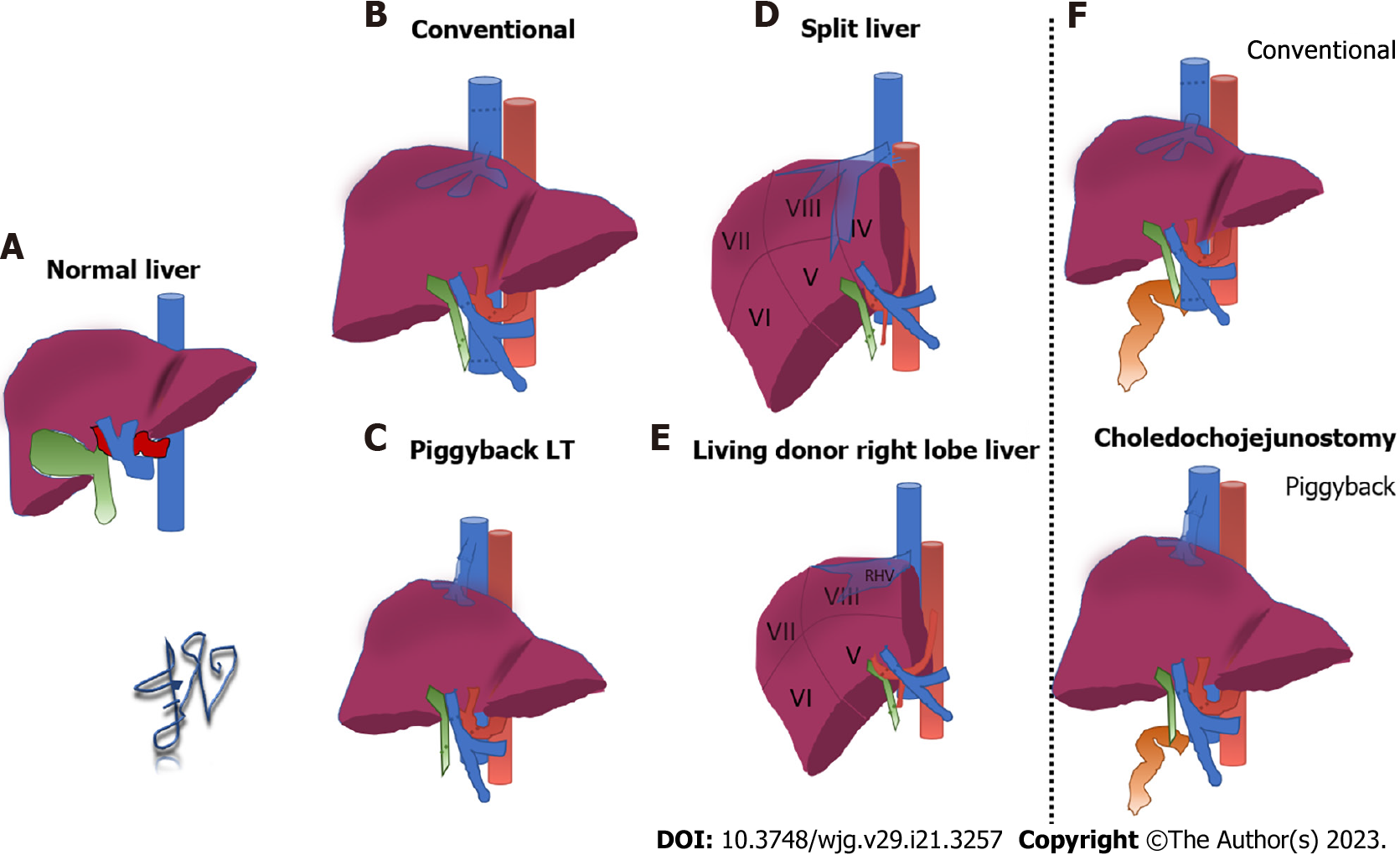
Figure 1 Schematic representation of surgical techniques for liver transplantation.
A: Normal anatomy of the liver; B: Conventional technique for liver transplantation; C: Piggyback technique; D: Split liver technique in adults; E: Living donor right lobe liver transplantation; F: Conventional (top row) and piggyback (bottom row) techniques with choledochojejunostomy.
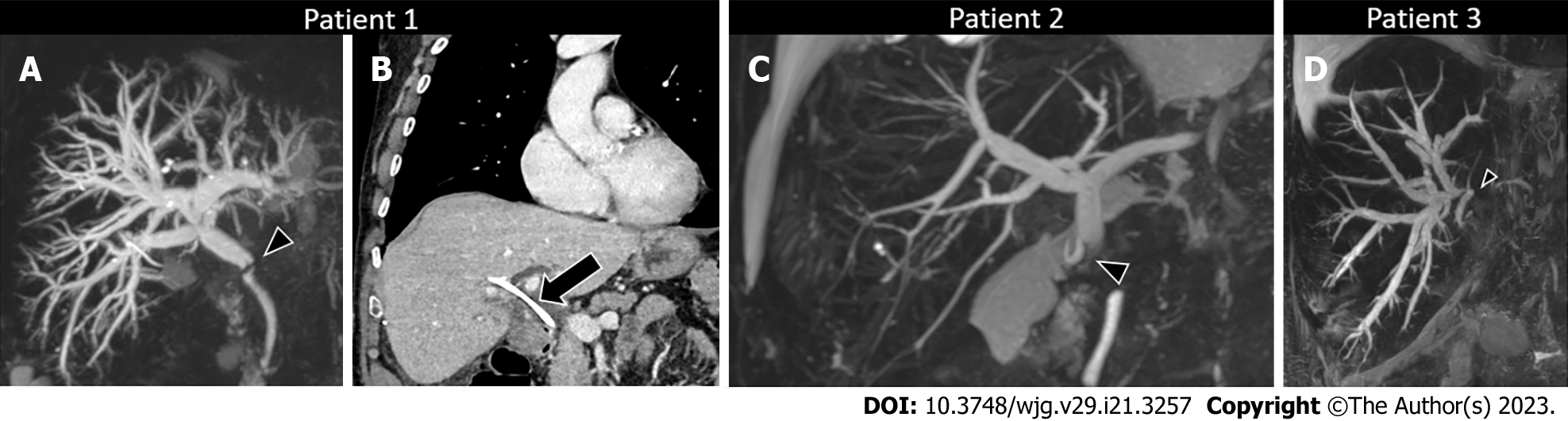
Figure 2 Anastomotic biliary strictures.
A: Anastomotic stricture of choledochocholedochostomy 3 mo after liver transplantation. Endoscopic retrograde cholangiopancreatography was performed with balloon dilatation of the stricture and stent positioning. Magnetic resonance cholangiopancreatography (MRCP) maximum intensity projection (MIP) demonstrates anastomotic biliary stricture (arrowhead) with marked upstream biliary dilatation; B: Contrast enhanced computed tomography in the coronal plane shows in the same patient the stent in the biliary tree (arrow) and normal biliary tree caliber; C: Anastomotic stricture of choledochojejunostomy 6 mo after liver transplantation. MRCP MIP demonstrates anastomotic biliary stricture (arrowhead) with marked upstream biliary dilatation; D: Anastomotic stricture of end-to-end biliary anastomosis after split liver transplantation with right split lobe. MRCP MIP demonstrates anastomotic biliary stricture (arrowhead) with marked upstream biliary dilatation of the right split transplanted lobe.
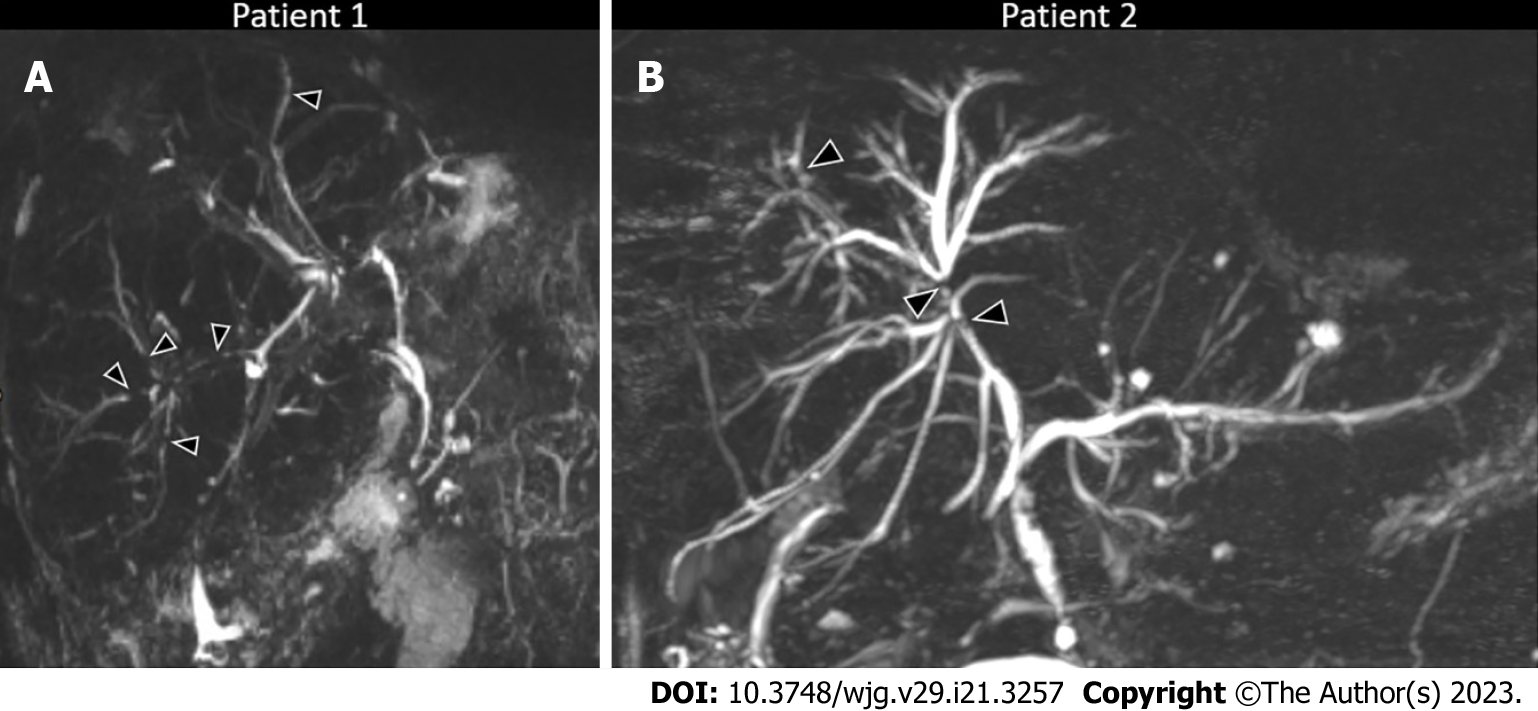
Figure 3 Non-anastomotic biliary strictures.
A: Non-anastomotic strictures in a patient with chronic rejection demonstrated at biopsy 11 y after transplant and then re-transplanted. Magnetic resonance cholangiopancreatography (MRCP) maximum intensity projection (MIP) demonstrates multiple non-anastomotic biliary strictures (arrowheads); B: Non-anastomotic strictures in a patient with recurrent secondary cholangitis 4 y after liver transplantation. MRCP MIP demonstrates multiple non-anastomotic biliary strictures (arrowheads) with upstream biliary dilatation.
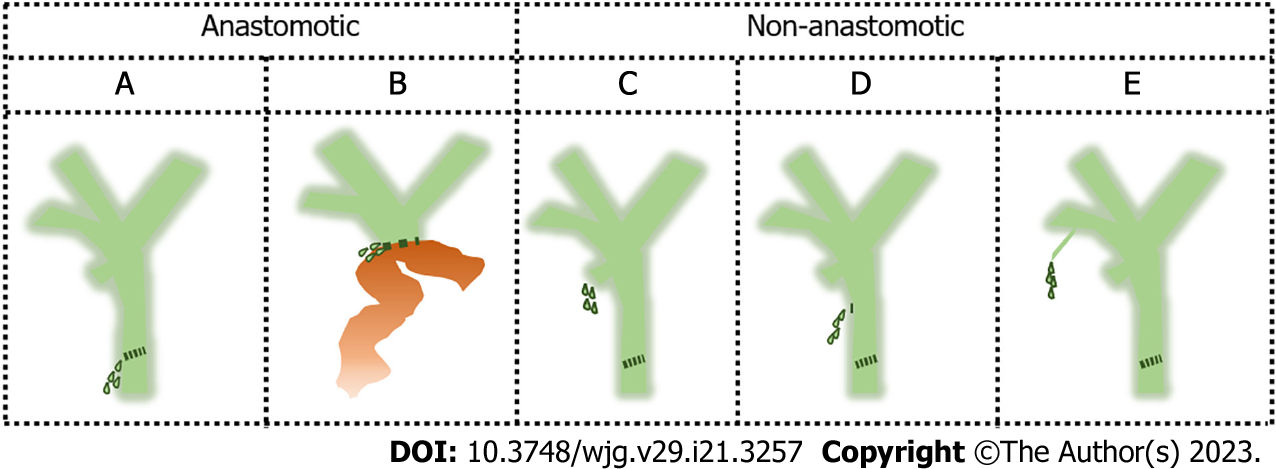
Figure 4 Schematic representation of biliary leaks.
A: Anastomotic leak at the level of choledochocholedochostomy; B: Anastomotic leak at the level of choledochojejunostomy; C: Non-anastomotic leak at the level of the cystic duct stump; D: Non-anastomotic leak at the level of T-tube removal; E: Non-anastomotic leak from small bile ducts that are transected perioperatively during hepatic resection.
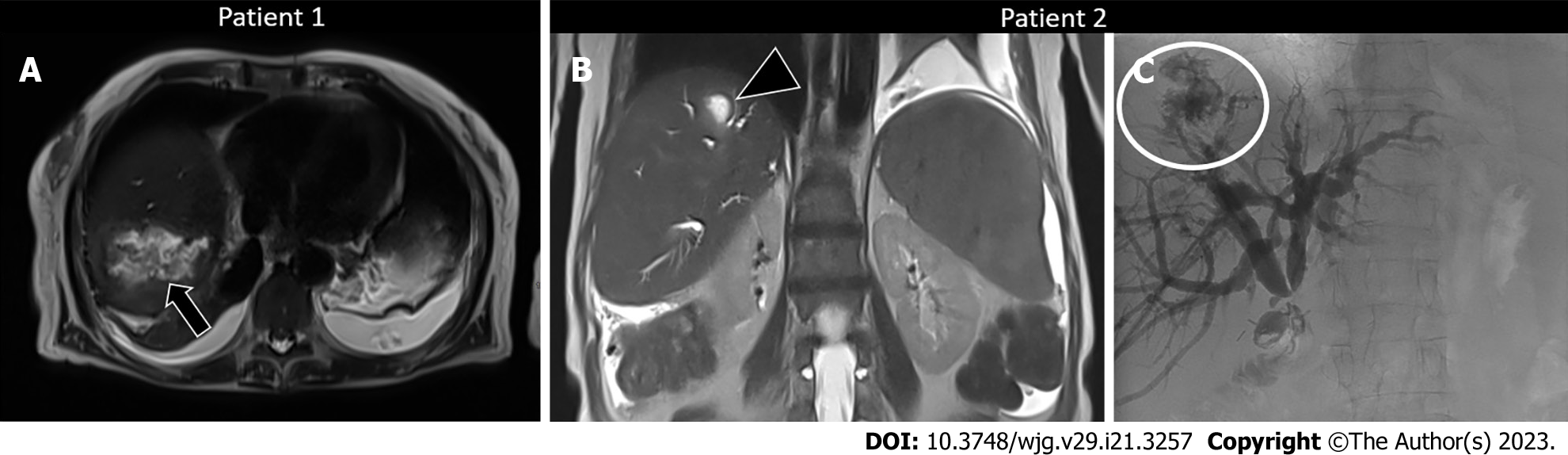
Figure 5 Biloma and biliary leak after liver transplantation.
A: Patient with biloma occurring 9 mo after liver transplantation. T2-weighted axial image shows a collection (arrow) in the right hepatic lobe with internal heterogenous signal intensities. Percutaneous drainage of the collection was performed demonstrating superinfected biloma; B: Patient with biliary leak occurring after liver transplantation. T2-weighted coronal magnetic resonance imaging shows an intrahepatic fluid collection (arrowhead) consistent with biloma; C: Cholangiographic image in the same patient demonstrated the biliary leak (circle) causing an intrahepatic biloma.
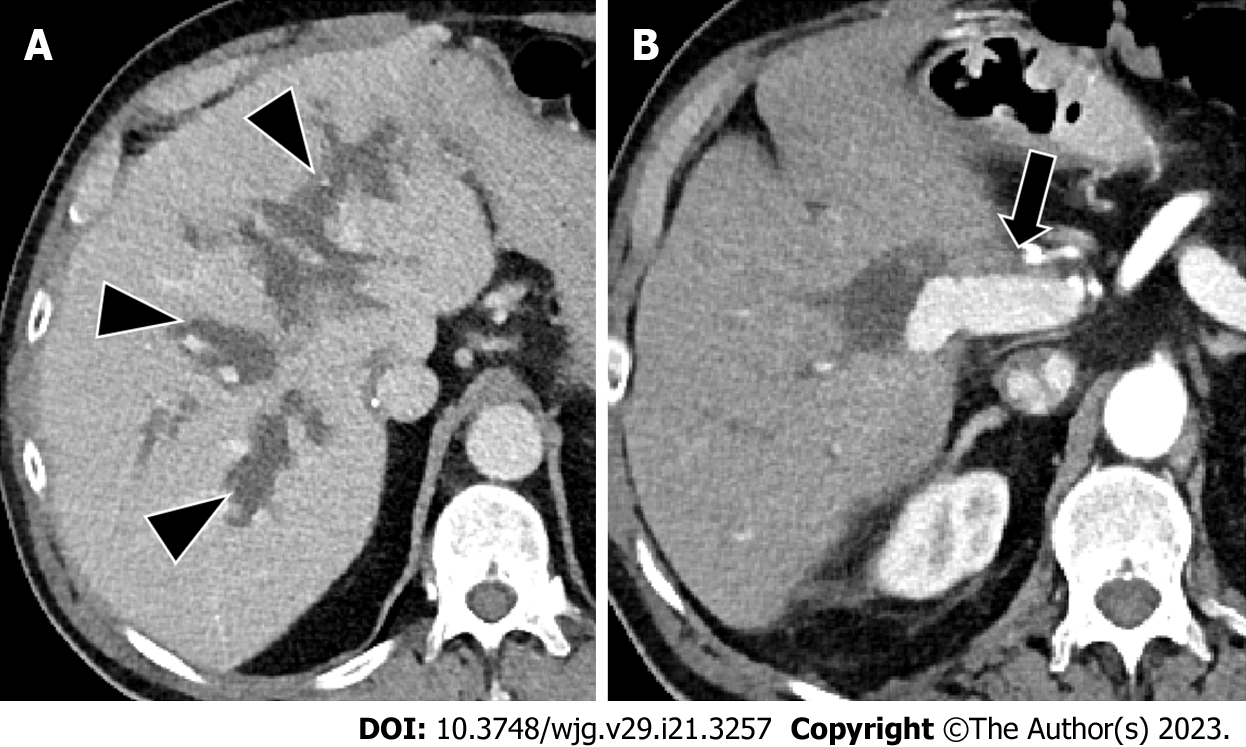
Figure 6 Biliary lakes occurring after liver transplantation.
A: Contrast-enhanced computed tomography (CT) in the axial plane in the portal venous phase demonstrates biliary lakes (arrowheads) adjacent to the portal vein branches; B: Contrast-enhanced CT in the arterial phase demonstrates lack of enhancement of the hepatic artery (arrow) caused by the adjacent surgical clip.
Figure 7 Lack of excretion of hepatobiliary contrast after liver transplantation in a patient with increased serum bilirubin of 2.
2 mg/dL. Gadoxetate disodium-enhanced magnetic resonance imaging in the hepatobiliary phase acquired at 20 min is inadequate as demonstrated by hypointensity of the liver parenchyma compared to that of hepatic vessels and lack of contrast in the biliary tree.
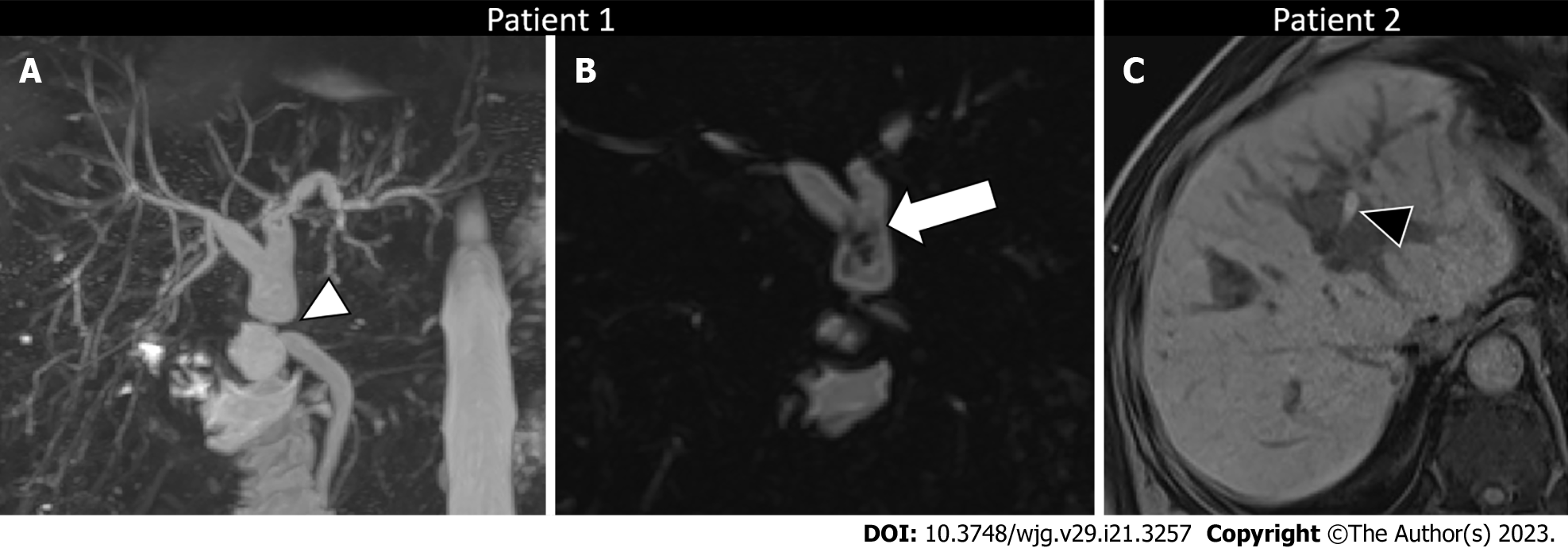
Figure 8 Biliary sludge and biliary cast.
A: Patient with biliary sludge and anastomotic stricture 3 mo after liver re-transplantation. Magnetic resonance cholangiopancreatography (MRCP) maximum intensity projection image demonstrates anastomotic biliary stricture (arrowhead) with marked upstream biliary dilatation; B: Three-dimensional MRCP in the coronal plane in the same patient demonstrates biliary sludge (arrow) in the dilated hepatic duct extending into the left and right ducts. C: Patient with biliary cast 2 y after liver transplantation. Unenhanced T1-weighted gradient-recalled image shows hyperintense content (arrowhead) in the left biliary duct, consistent with biliary cast.
Figure 9 Enlarged ampullary papilla occurring years after liver transplantation and causing minimal cholestasis.
T2-weighted imaging in the coronal plane demonstrates an enlarged ampullary papilla (arrowhead) protruding in the duodenal lumen (arrow). Ultrasonography-endoscopy confirmed the enlarged ampullary papilla and biopsy was performed, which excluded malignancy and confirmed the diagnosis of papillary stenosis (i.e. sphincter of Oddi dysfunction); sphincterotomy was then performed.
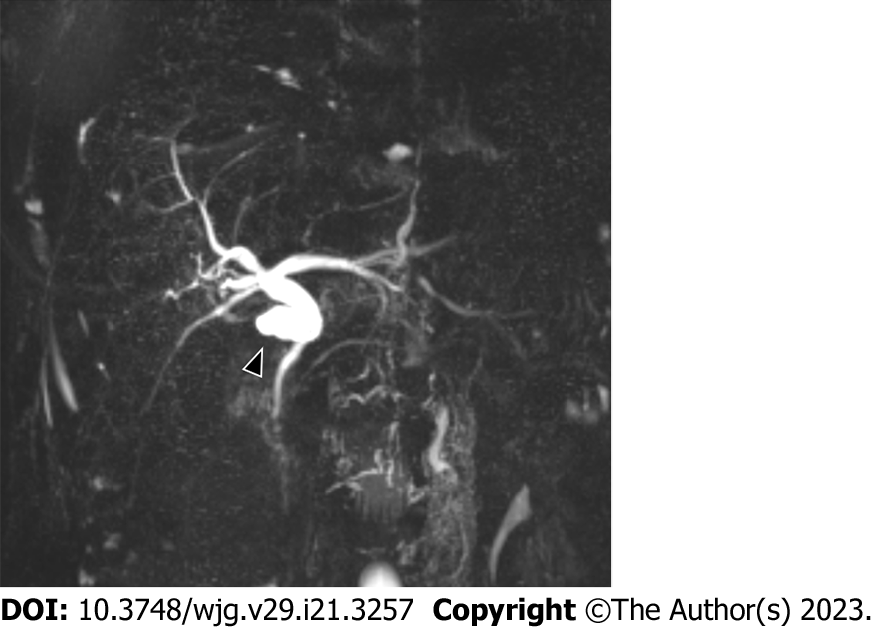
Figure 10 Mucocele occurring years after liver transplantation.
Magnetic resonance cholangiopancreatography maximum intensity projection shows a fluid collection in communication with biliary tree. Biliary content was confirmed with percutaneous drainage.
- Citation: Vernuccio F, Mercante I, Tong XX, Crimì F, Cillo U, Quaia E. Biliary complications after liver transplantation: A computed tomography and magnetic resonance imaging pictorial review. World J Gastroenterol 2023; 29(21): 3257-3268
- URL: https://www.wjgnet.com/1007-9327/full/v29/i21/3257.htm
- DOI: https://dx.doi.org/10.3748/wjg.v29.i21.3257