Copyright
©The Author(s) 2022.
World J Gastroenterol. Dec 28, 2022; 28(48): 6846-6866
Published online Dec 28, 2022. doi: 10.3748/wjg.v28.i48.6846
Published online Dec 28, 2022. doi: 10.3748/wjg.v28.i48.6846
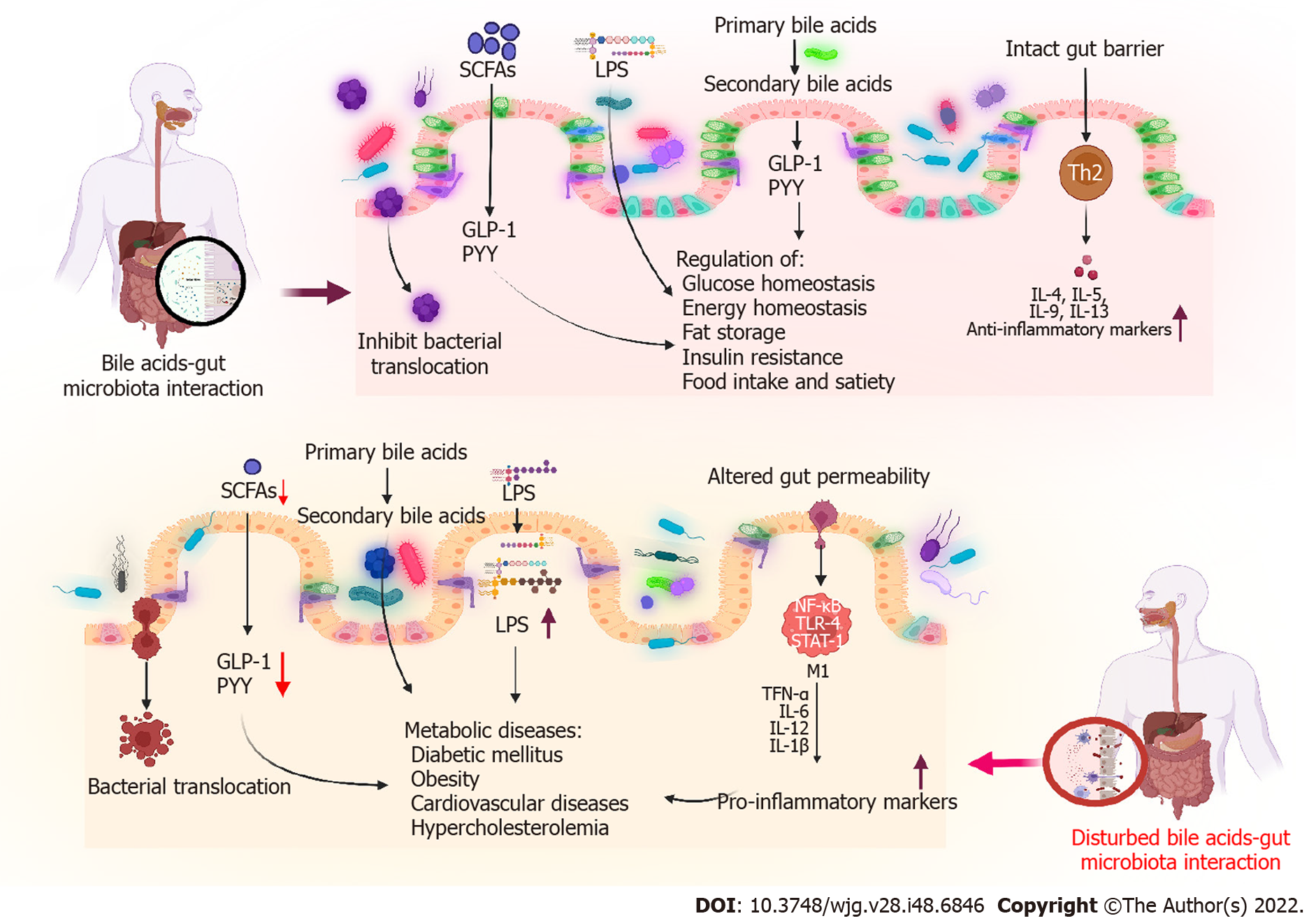
Figure 1 Graphical abstract.
GLP-1: Glucagon-like peptide-1; LPS: Lipopolysaccharide; PYY: Peptide YY; SCFAs: Short-chain fatty acids.
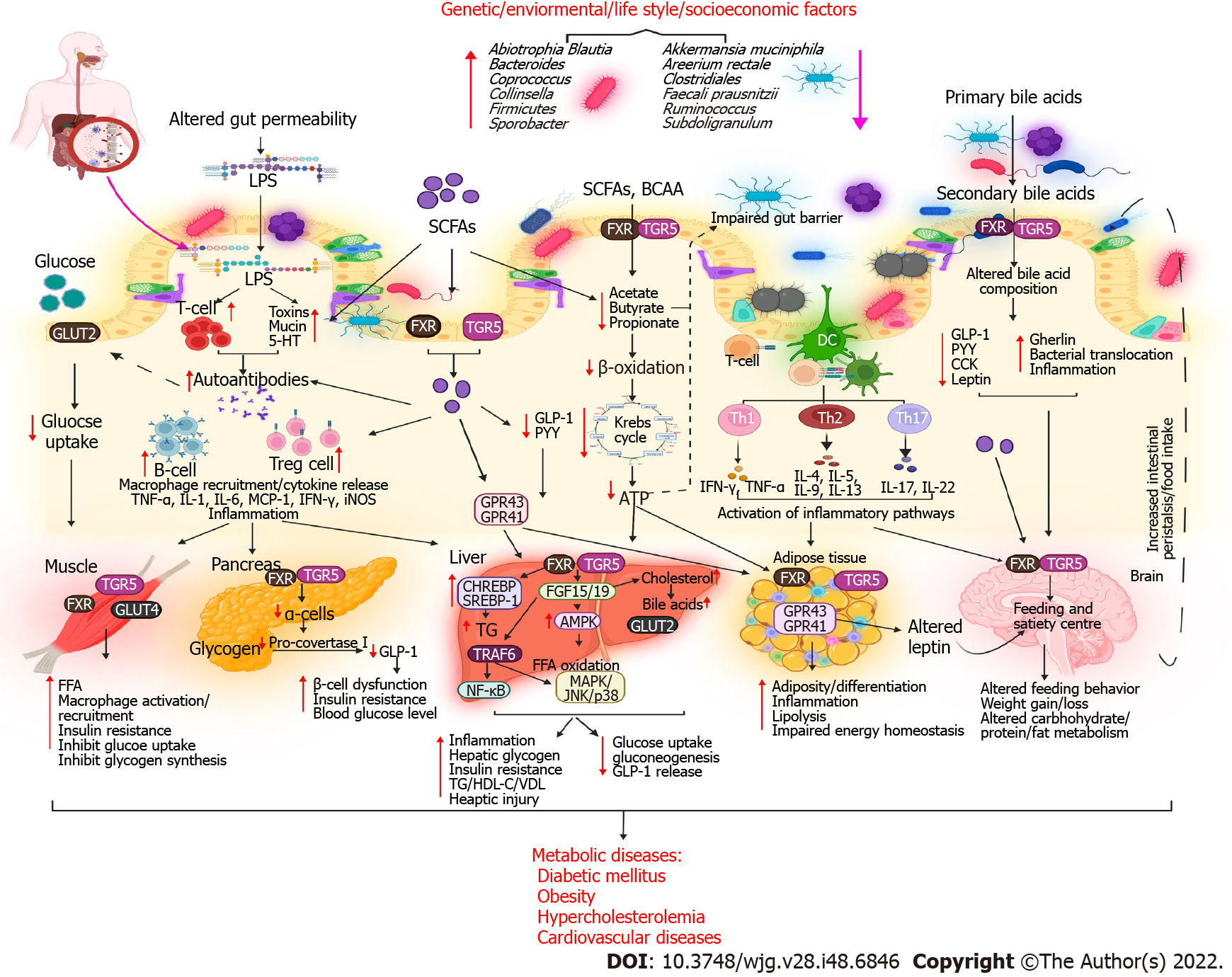
Figure 2 Metabolic diseases resulting from altered bile acid–gut microbiome interactions.
The health and gut microbiota of individuals are affected by genetic, environmental, lifestyle, and socioeconomic factors. Due to altered gut microbial composition, the permeability of the gut barrier is impaired, facilitating pathogen invasion in the intestinal lumen via receptor-mediated pathways. Increased levels of lipopolysaccharide and short-chain fatty acids trigger the immune system, result in the production of autoantibodies (B cells and Treg cells), and cause the infiltration of macrophages, which release toxins and lead to inflammation and metabolic endotoxemia. Conversely, the release of glucagon-like peptide-1 (GLP-1), peptide YY (PYY), and ghrelin is decreased, altering carbohydrate, protein, and fat metabolism. When glucose uptake is decreased in the intestine, free fatty acid synthesis is increased, macrophages are activated, and muscles become insulin resistant. When circulating autoantibodies enter the pancreas, they destroy α and β cells, thereby reducing insulin secretion and enhancing insulin sensitivity. A decrease in FGF15/19, CHREBP, SREBP-1, and TRAF6 expression levels in the liver activates NF-κB/MAPK inflammatory pathways, resulting in liver dysfunction and altered fat metabolism in the liver. Proinflammatory markers and reduced GLP-1, PYY, and ghrelin levels affect adipose tissue function, leading to increased adiposity and impaired energy metabolism. In the brain, altered levels of GLP-1, PYY, ghrelin, and leptin affect feeding and satiety centers. These changes lead to the development of metabolic diseases. FFA: Free fatty acid; GLP-1: Glucagon-like peptide-1; SCFAs: Short-chain fatty acids; LPS: Lipopolysaccharide; PYY: Peptide YY; CCK: Cholecystokinin; FXR: Farnesoid X receptor; CCK: Cholecystokinin; TG: Triglycerides; HDL-C: High-density lipoprotein cholesterol; VLDL: Very-low-density lipoprotein.
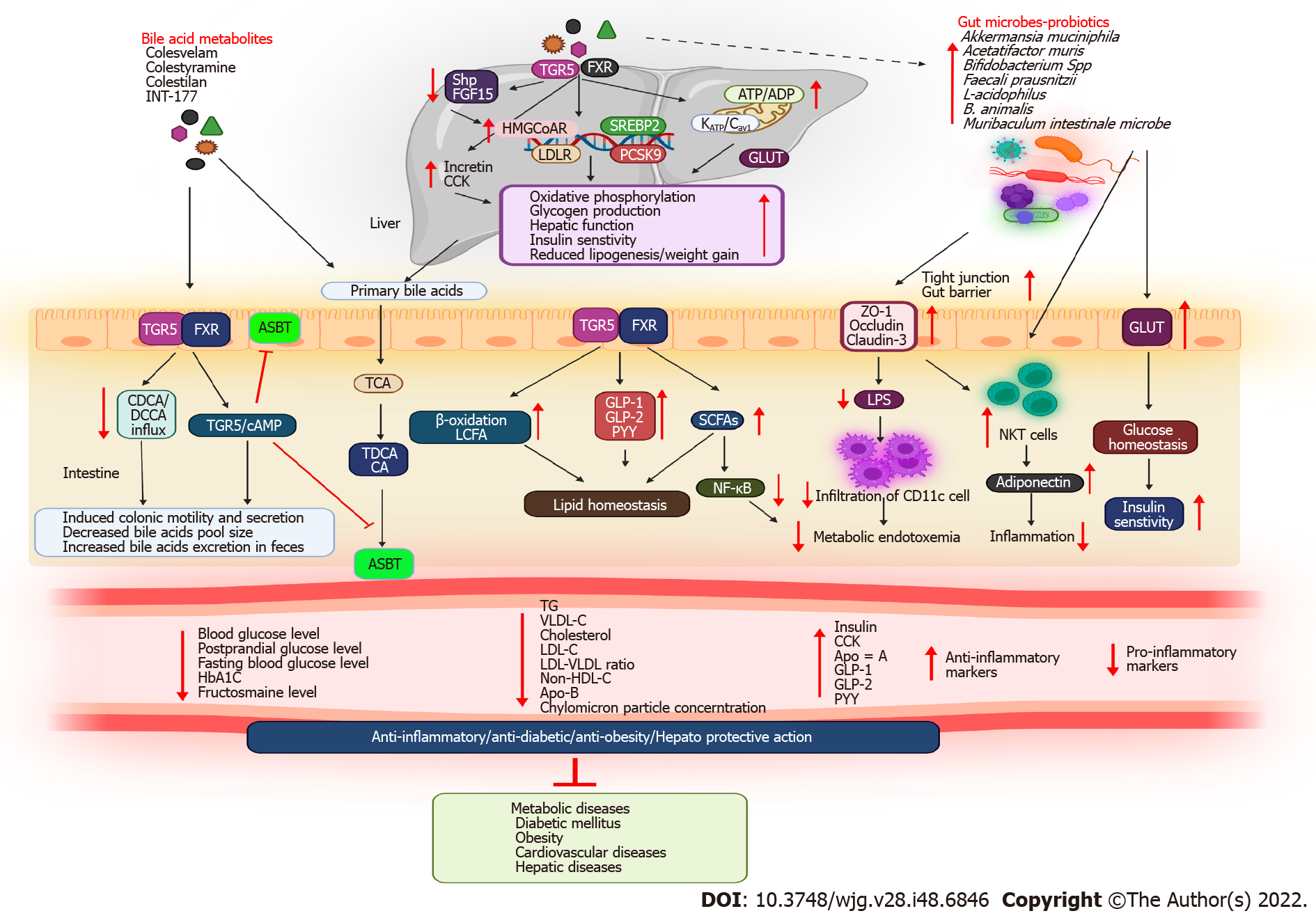
Figure 3 Mechanism by which bile acid metabolites and gut microbes alleviate metabolic diseases.
Bile acid metabolites, e.g., bile acid sequestrants (BASs), enter the liver via receptor-mediated pathways. As a result of their effects, mitochondrial oxidative phosphorylation is stimulated; HMGCoAR, LDLR, and SREBP2 gene expression is induced; incretin and cholecystokinin levels are increased; and the abundance of intestinal bacteria is increased, reducing the levels of triglyceride (TG), very-low-density lipoprotein (VLDL), and cholesterol in the blood. By increasing the expression of ZO-1, occludin, and claudin-3 in the gut lumen, probiotics facilitate tight junction proteins, preventing macrophage infiltration and metabolic endotoxemia. In contrast, BAS improves colonic motility; increases glucagon-like peptide-1 (GLP-1), peptide YY (PYY), and ghrelin secretion; and regulates carbohydrate, fat, and energy metabolism, thereby reducing blood glucose, TG, cholesterol, and VLDL levels and improving insulin sensitivity and liver function. Because of their anti-inflammatory, antidiabetic, and antiobesity properties, BASs and gut microbes alleviate metabolic diseases. CDCA: Chenodeoxycholic acid; TDCA: Taurodeoxycholic acid; GLP-1: Glucagon-like peptide-1; SCFAs: Short-chain fatty acids; LPS: Lipopolysaccharide; PYY: Peptide YY; FXR: Farnesoid X receptor; CCK: Cholecystokinin; TG: Triglycerides; LDLR: Low-density lipoprotein; NKT: natural killer T.
- Citation: Sah DK, Arjunan A, Park SY, Jung YD. Bile acids and microbes in metabolic disease. World J Gastroenterol 2022; 28(48): 6846-6866
- URL: https://www.wjgnet.com/1007-9327/full/v28/i48/6846.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i48.6846