Copyright
©The Author(s) 2022.
World J Gastroenterol. Dec 21, 2022; 28(47): 6662-6688
Published online Dec 21, 2022. doi: 10.3748/wjg.v28.i47.6662
Published online Dec 21, 2022. doi: 10.3748/wjg.v28.i47.6662
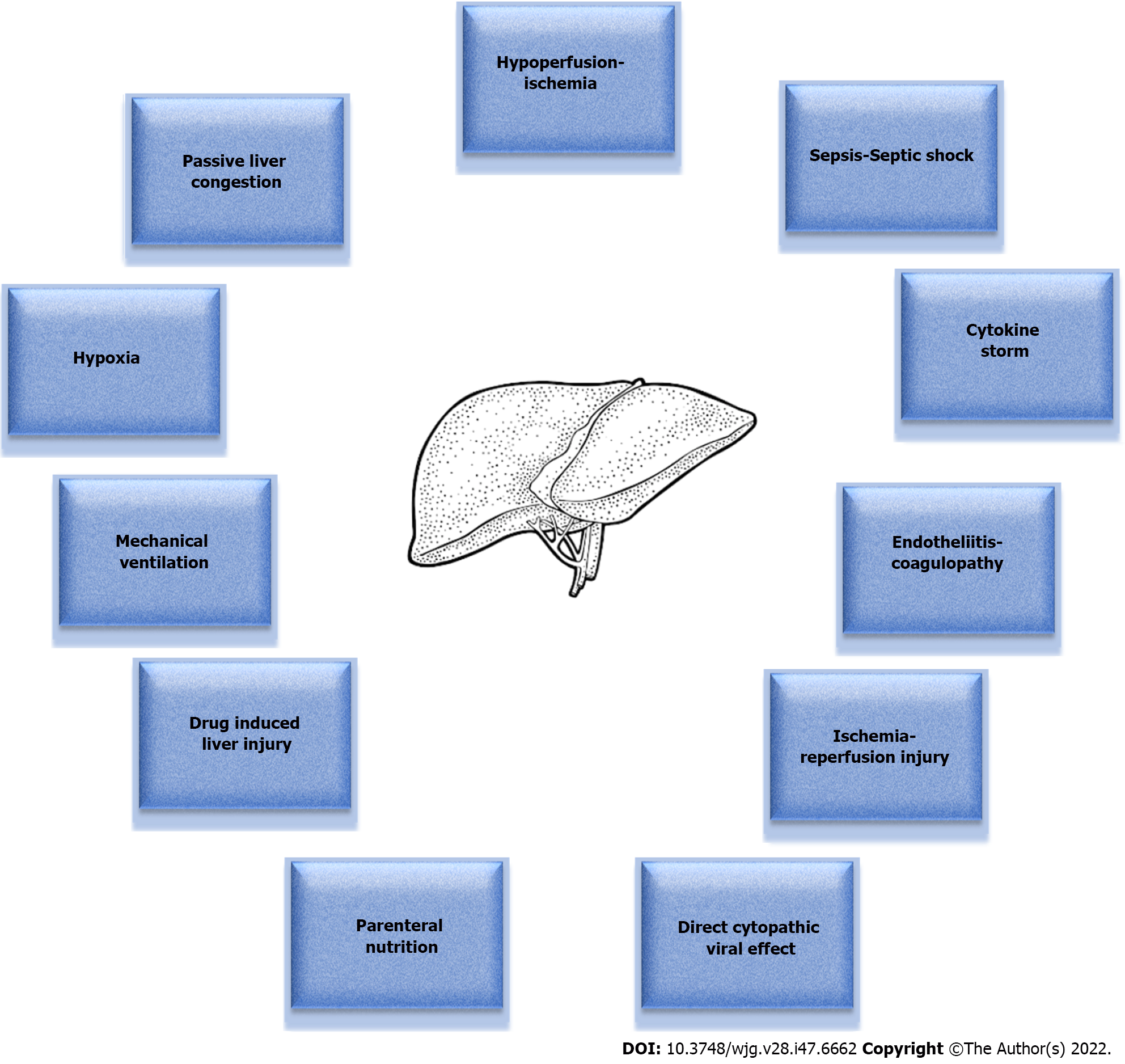
Figure 1 Pathophysiological mechanisms implicated in the development of coronavirus disease 2019 acute liver injury in the intensive care unit setting.
Figure 1 depicts the various pathophysiological mechanisms that come into play in the setting of coronavirus disease 2019 (COVID-19) infection, which eventually culminate in the development of acute liver injury (ALI) in intensive care unit (ICU) patients. Hypoperfusion and ischemia due to the frequently observed hemodynamic instability in the ICU patients play a major role in the process. Passive liver congestion as a result of congestive heart failure of various etiologies is another key determinant. The situation can be further aggravated by ischemia-reperfusion injury. Sepsis can also cause hepatic dysfunction, which is usually cholestatic in nature and reversible, but, when it progresses to septic shock, it results in multiple organ dysfunction syndrome and liver hypoperfusion, manifesting as shock liver. Besides, hypoxia due to respiratory failure and acute respiratory distress syndrome may also lead to ALI. Paradocixally, mechanical ventilation per se can exert deleterious effects on the liver through positive pressure ventilation, especially when accompanied by the application of high positive end-expiratory pressure and large tidal volumes. Furthermore, ALI can stem from the inflammatory cascade generated by the cytokine storm, while it can be further complicated by impaired microcirculation and thrombosis as a result of endotheliitis with concomitant coagulopathy. Drug-induced liver injury, as well as parenteral nutrition, must also not be overlooked as potential causative factors. Finally, liver injury could also be attributed to a direct cytopathic viral effect. There seems to be a complex interplay among these numerous underlying mechanisms, which may act either independently and cause COVID-19 induced ALI in the ICU setting, or more frequently synergistically and generate a relentless ALI vicious cycle.
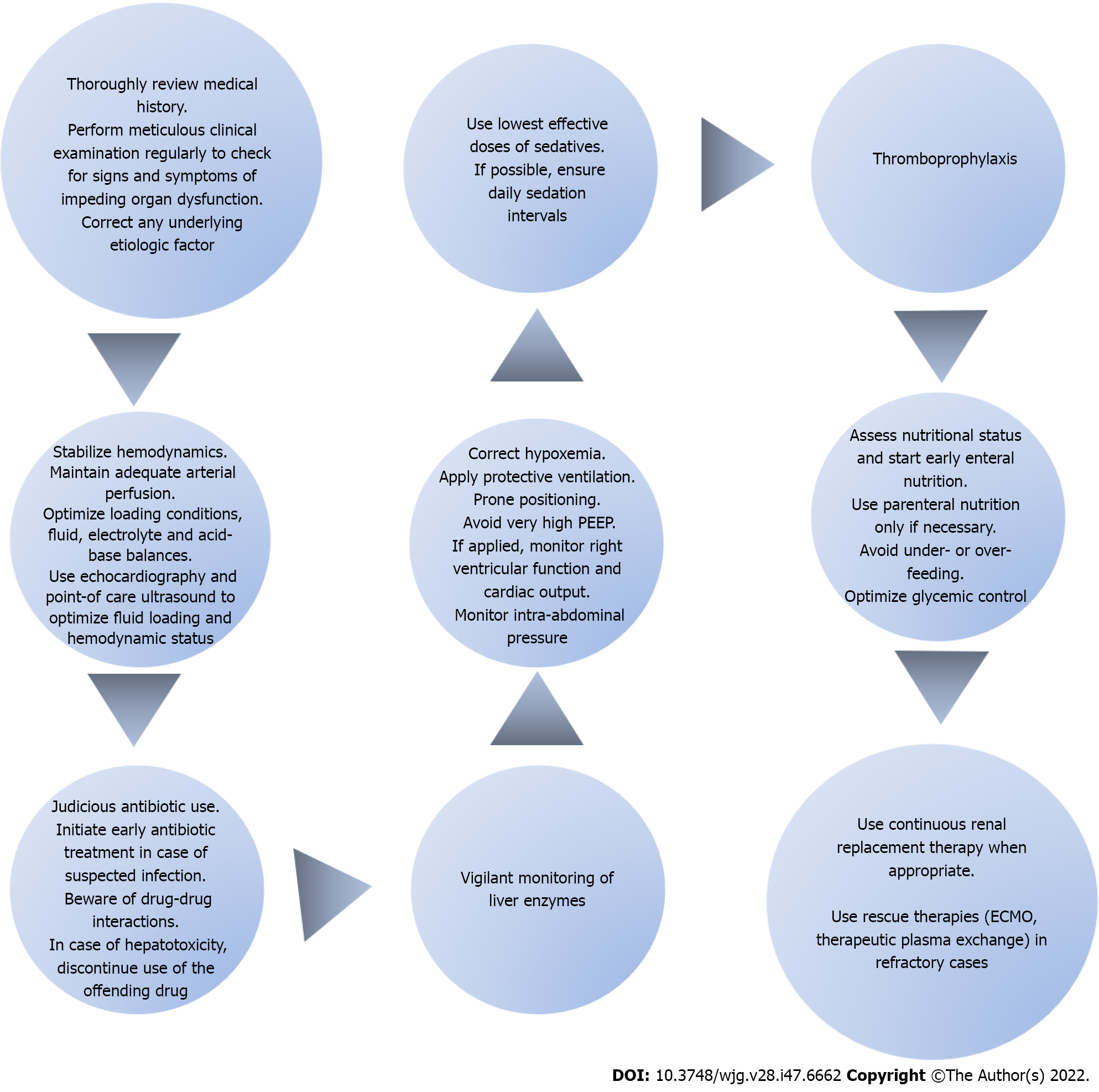
Figure 2 Steps of the intensive care unit therapeutic approach in patients with coronavirus disease 2019 induced acute liver injury.
The intensive care unit (ICU) therapeutic approach for coronavirus disease 2019 patients with acute liver injury (ALI) lies in preventive measures and is exclusively supportive once ALI ensues. After obtaining a detailed medical history, a thorough physical examination should be performed on a regular basis. Upon recognition of any signs of impeding liver dysfunction, the possible etiologic factor should be systematically sought and appropriately addressed. Hemodynamic stabilization of the patient is of paramount importance. The goal is to maintain adequate arterial perfusion in order to prevent liver ischemia. The use of echocardiography and point-of-care ultrasonography will help determine the hemodynamic status and optimize loading conditions. It is important to constantly maintain fluid, electrolyte and acid-base balances. Furthermore, early identification and management of sepsis cannot be overemphasized. Prompt initiation of appropriate antibiotic therapy is the mainstay of sepsis management. Antibiotics should be used judiciously with an increased level of awareness for possible drug-drug interactions. In case of hepatotoxicity, the administration of the responsible pharmacologic agent should be discontinued. Close monitoring of liver enzymes is advised at all times. Furthermore, hypoxia should be consistently addressed and corrected. In mechanically ventilated patients, a lung-protective ventilation strategy should be implemented with the use of low tidal volumes coupled with a target of plateau pressure < 30 cm H2O. The application of very high positive end-expiratory pressure should be avoided because it could compromise right ventricular performance and precipitate passive liver congestion. Moreover, prone positioning is recommended in order to improve hypoxia. Intra-abdominal pressure should also be monitored so as to prevent any potential increases related to mechanical ventilation which could jeopardize liver function. Additionally, optimal sedation strategies should be applied with the lowest effective doses and daily sedation intervals. Thromboprophylaxis is strongly recommended as a preventive measure in all ICU patients. Besides that, nutritional status should be regularly assessed and efforts should focus on initiating early enteral feeding while avoiding parenteral nutrition. Under- or over- feeding should be avoided and glycemic control should be optimized. Finally, renal replacement therapy can be used whenever indicated. In refractory cases, rescue therapies may be employed with the use of extracorporeal membrane oxygenation and therapeutic plasma exchange in an attempt to provide circulatory and respiratory support and reverse end-organ failure. PEEP: Positive end-expiratory pressure; ECMO: Extracorporeal membrane oxygenation.
- Citation: Polyzogopoulou E, Amoiridou P, Abraham TP, Ventoulis I. Acute liver injury in COVID-19 patients hospitalized in the intensive care unit: Narrative review. World J Gastroenterol 2022; 28(47): 6662-6688
- URL: https://www.wjgnet.com/1007-9327/full/v28/i47/6662.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i47.6662