Copyright
©The Author(s) 2022.
World J Gastroenterol. Oct 21, 2022; 28(39): 5707-5722
Published online Oct 21, 2022. doi: 10.3748/wjg.v28.i39.5707
Published online Oct 21, 2022. doi: 10.3748/wjg.v28.i39.5707
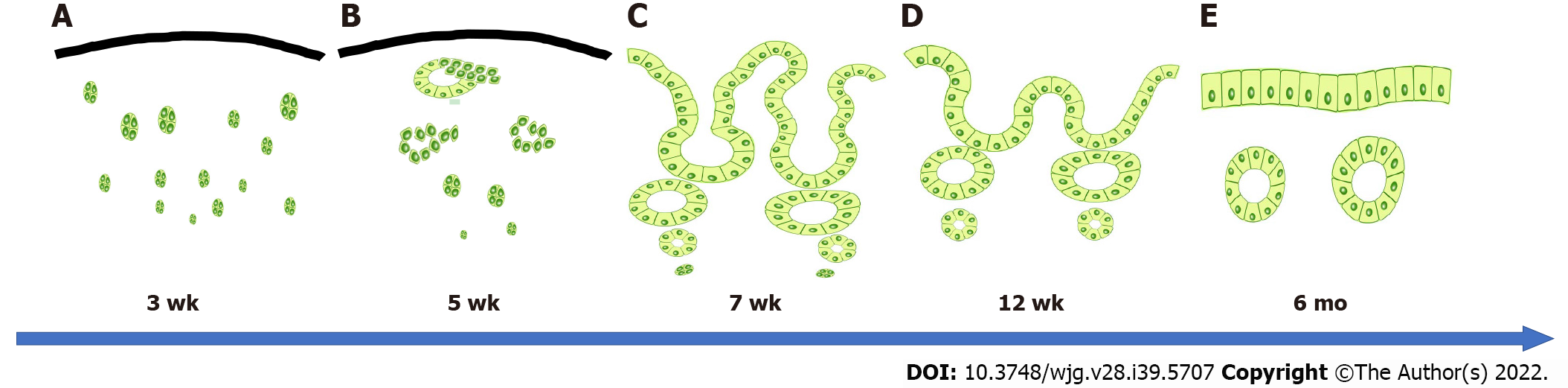
Figure 1 Ideal bile duct regeneration process.
A: Bile duct regeneration at approximately 3 wk. Numerous cell masses appear in the stroma that are thought to form peribiliary glands; B: Bile duct regeneration at approximately 5 wk. A ring-shaped peribiliary gland-like structure is observed, in which cell masses that are thought to form peribiliary glands are fused; C: Bile duct regeneration at approximately 7 wk. Numerous bile duct-attached glandular structures are observed on the bile passage surface, and the epithelial surface exhibits a high papillary morphology; D: Bile duct regeneration at approximately 12 wk. The number of peribiliary glands on the bile passage surface is decreased, the peribiliary glands become fused, and the epithelial surface becomes more even; E: Approximately 6 mo after bile duct regeneration. Similar to the native bile duct, the epithelial surface becomes a single layer of cubic columnar epithelium.
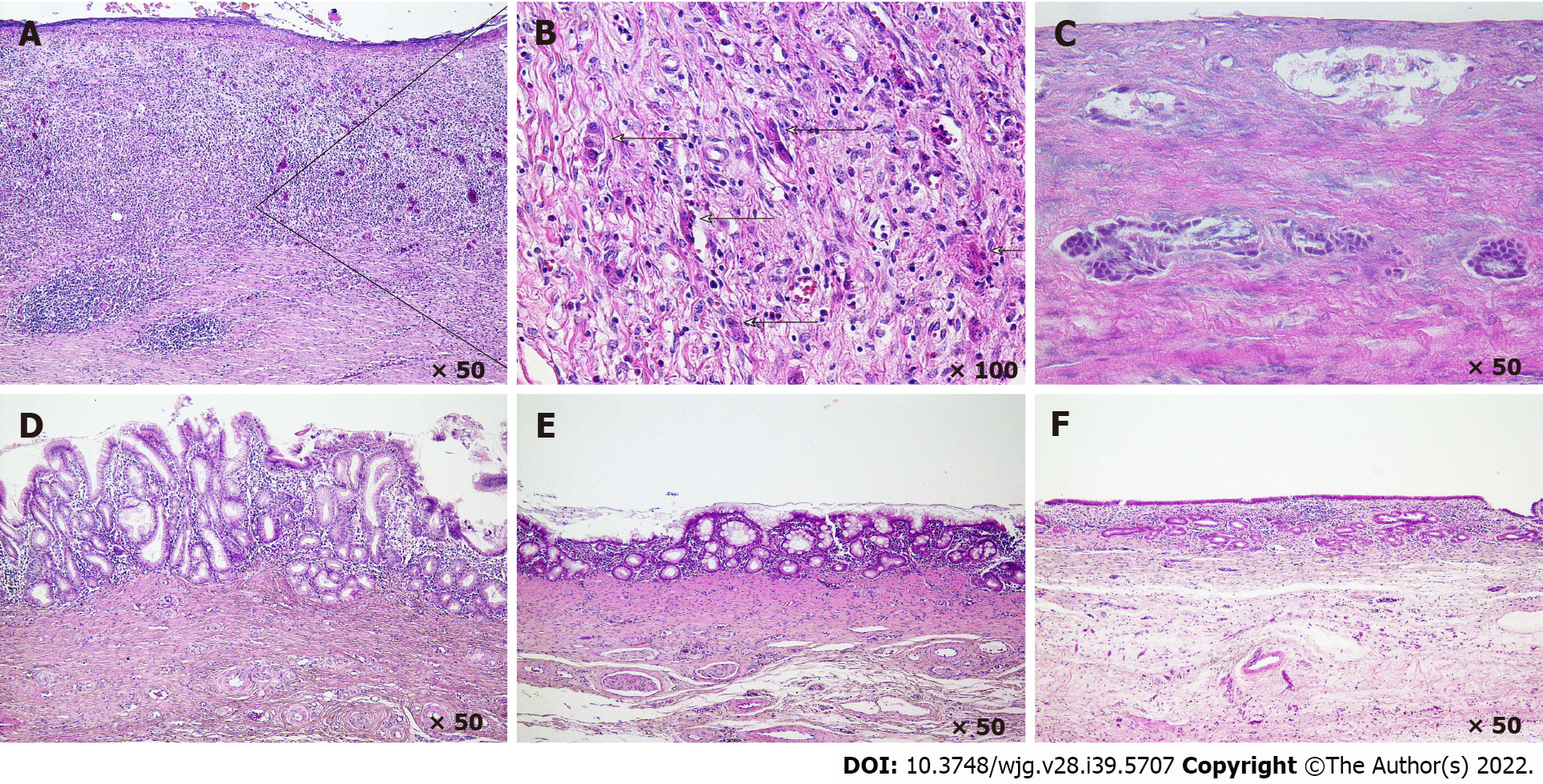
Figure 2 Histology of bile duct regeneration on the outside of the short-term absorption type bile duct substitute.
A and B: At 3 wk after bile duct substitute (BDS) implantation, a cell population in the stroma that may comprise the origin of the peribiliary gland is observed; C: At 5 wk after BDS implantation, a ring-shaped biliary gland-like structure is observed in which cell masses that are thought to form peribiliary glands are fused; D: At 7 wk after BDS implantation, many bile duct appendages are observed on the bile passage surface, and the epithelial surface exhibits a high papillary morphology; E: At 12 wk after BDS implantation, the number of peribiliary gland on the bile passage surface is decreased, the appendages begin to fuse, and the epithelial surface becomes more even; F: At 6 mo after BDS implantation, the epithelial surface becomes a single layer of cubic columnar epithelium, similar to the native bile duct.
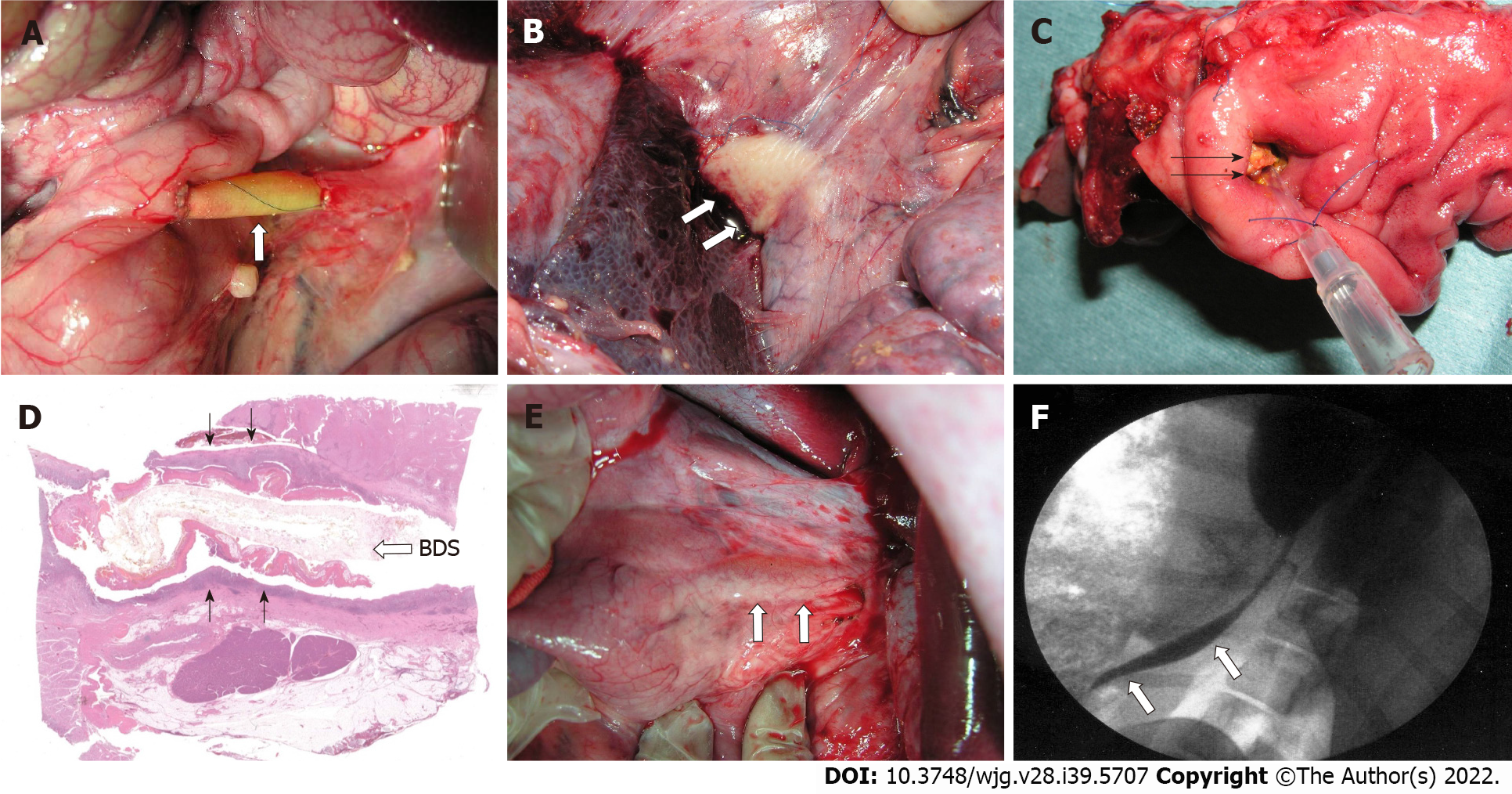
Figure 3 Bile duct substitutes using bioabsorbable material (synthetic polymer with short absorption period).
A: A bile duct substitute (BDS) using bioabsorbable material is implanted to bypass the extrahepatic bile duct (3 cm in size). Three weeks post-BDS implantation; B: White cell clusters are observed on the outside of the BDS; C: A vulnerable BDS is observed from the duodenal side; D: Dark purple connective tissue is noted on the outside of the BDS; E: At 6 mo after BDS implantation, the neo-bile duct is macroscopically similar to the natural common bile duct have been regenerated (arrow); F: Cholangiography (6 mo after BDS implantation). The BDS implant and anastomotic site become unknown, and the contrast medium flows smoothly into the duodenum (white arrows).
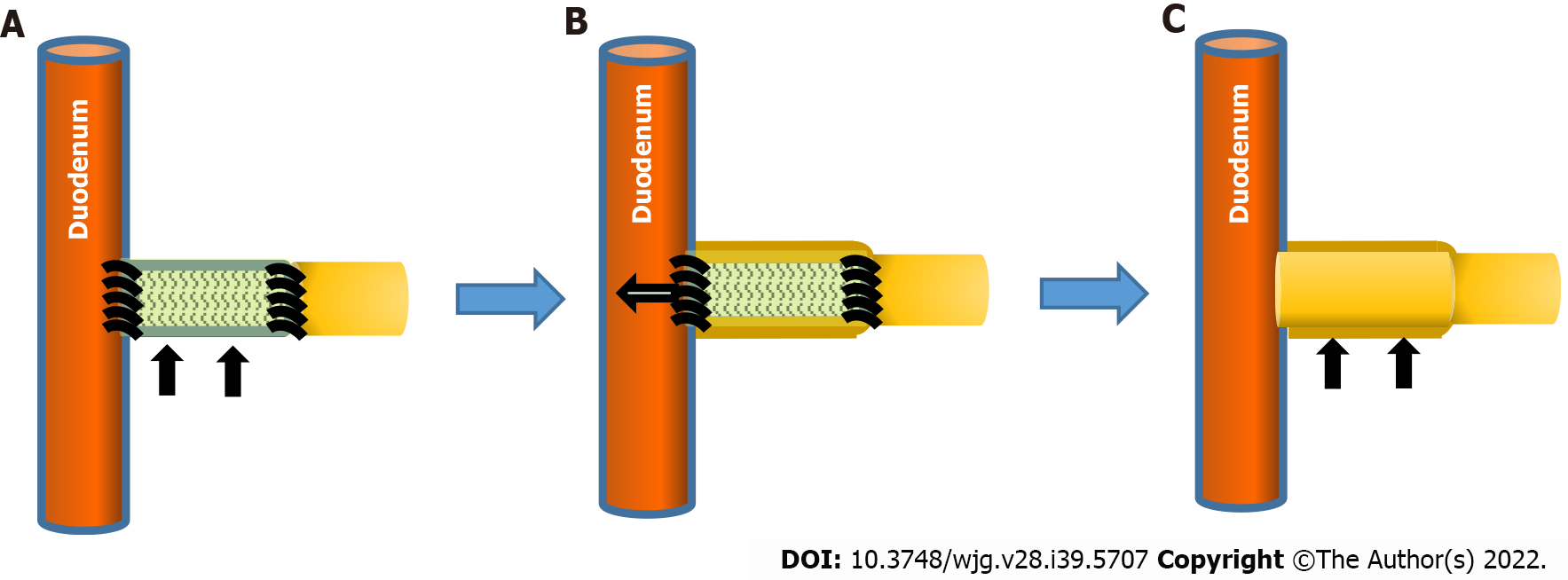
Figure 4 Regeneration of the neo-bile duct outside the short-term absorption type bile duct substitute.
A: Bile duct substitute (BDS) (black arrows) is anastomosed to the native extrahepatic bile duct; B: Immature cells attach around the BDS, forming a cylindrical cell mass outside the BDS. The bioabsorbable polymer that comprise BDS becomes fragile in the living body from approximately 3 wk and sheds to the duodenal side; C: After BDS is no longer present at the transplant site, immature cell clusters mature as bile duct cells and the bile ducts are regenerated as tissue (black arrows).
- Citation: Miyazawa M, Aikawa M, Takashima J, Kobayashi H, Ohnishi S, Ikada Y. Pitfalls and promises of bile duct alternatives: A narrative review. World J Gastroenterol 2022; 28(39): 5707-5722
- URL: https://www.wjgnet.com/1007-9327/full/v28/i39/5707.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i39.5707