Copyright
©The Author(s) 2022.
World J Gastroenterol. Oct 7, 2022; 28(37): 5469-5482
Published online Oct 7, 2022. doi: 10.3748/wjg.v28.i37.5469
Published online Oct 7, 2022. doi: 10.3748/wjg.v28.i37.5469
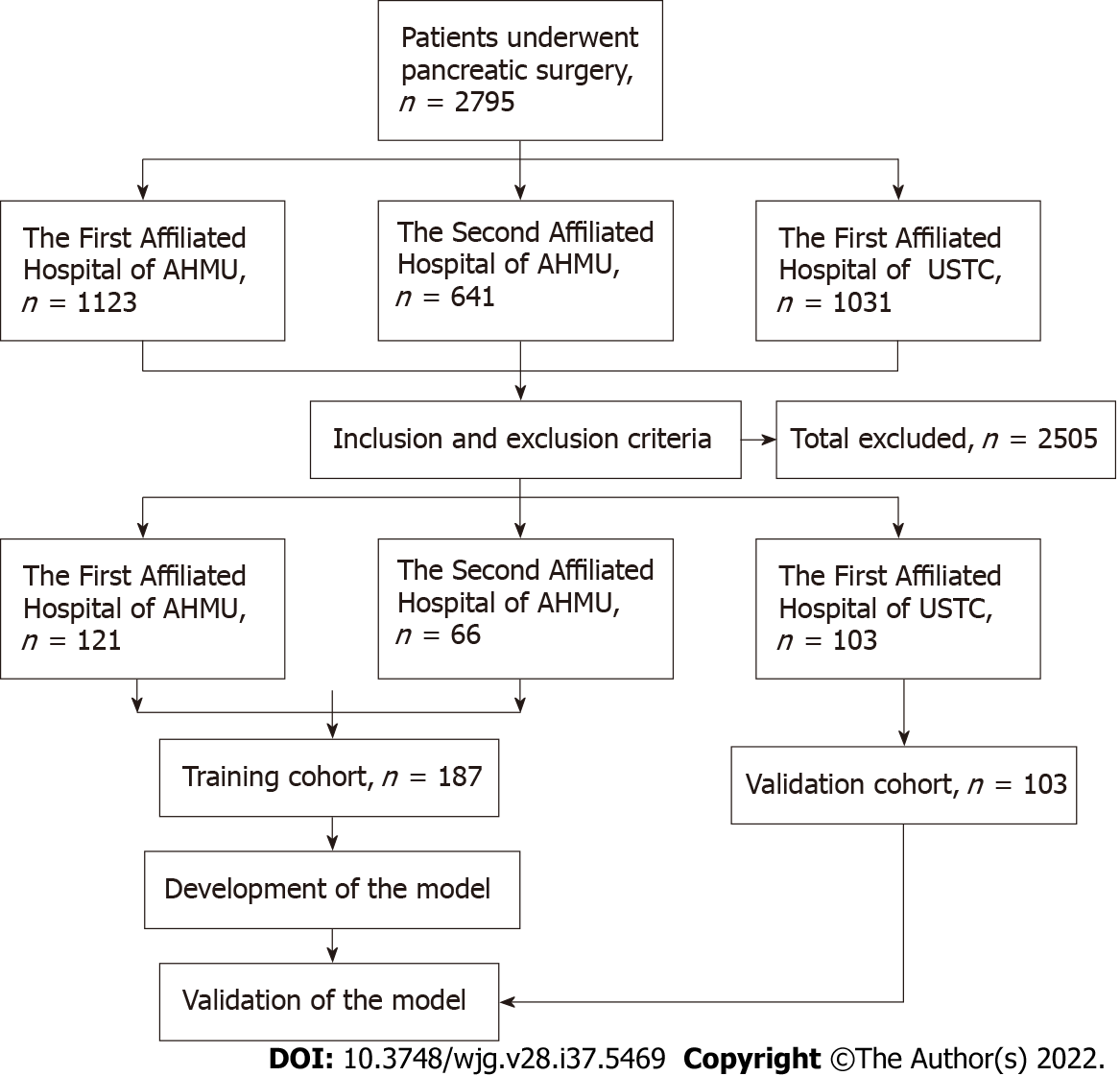
Figure 1 Flowchart of patient recruitment and diagnosis.
AHMU: Anhui Medical University; USTC: University of Science and Technology of China.
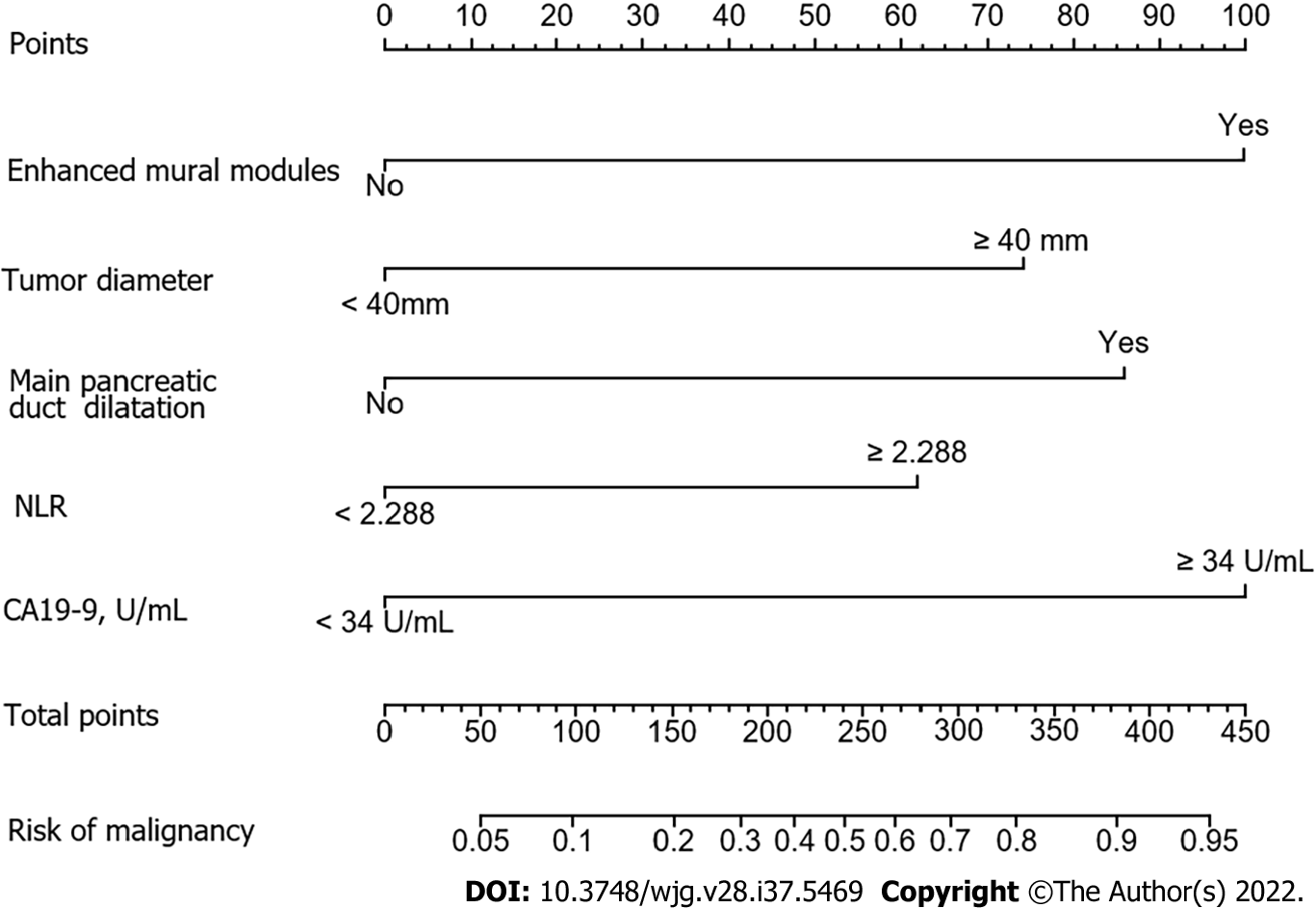
Figure 2 Nomogram for predicting risk of malignancy in the training cohort.
NLR: Neutrophil-to-lymphocyte ratio.
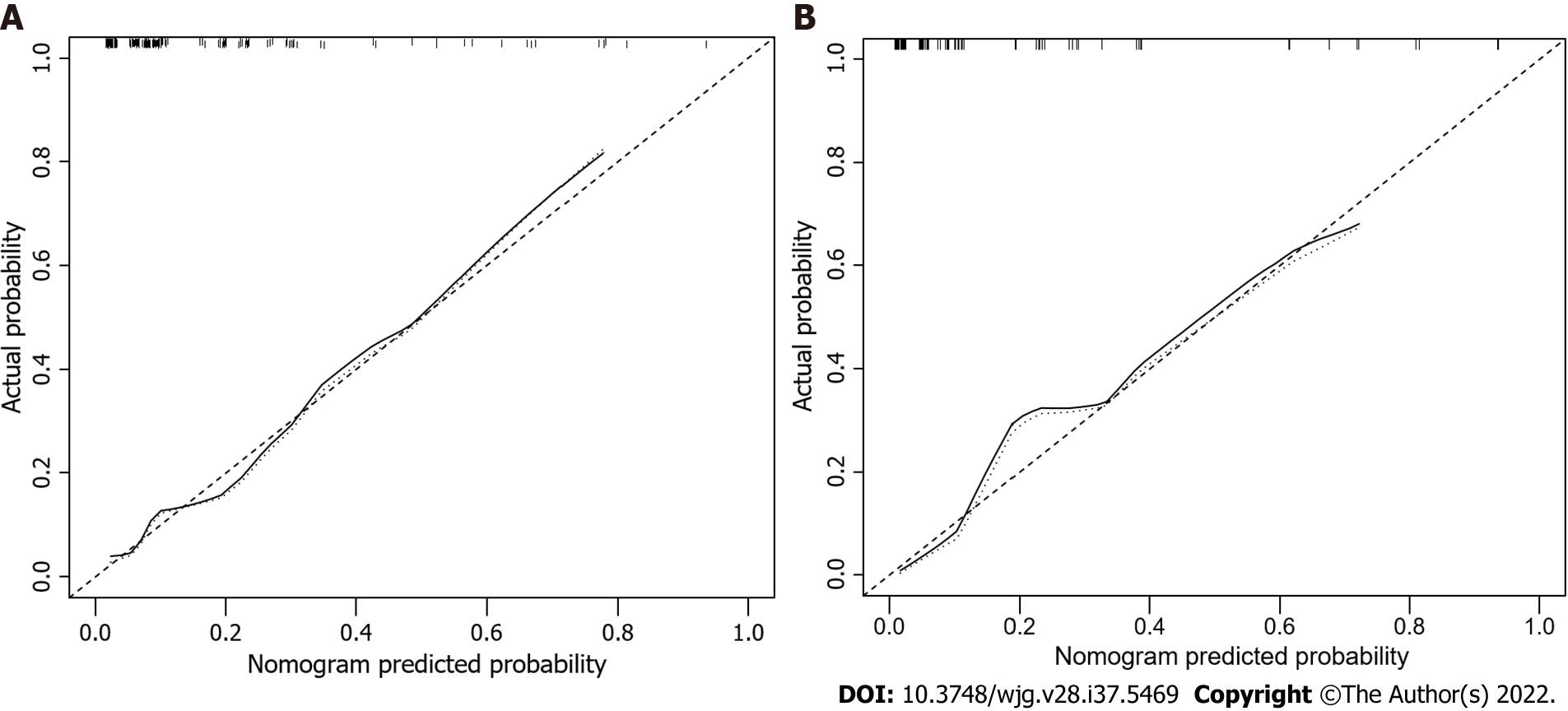
Figure 3 Calibration curves for predicting the risk of malignancy.
The nomogram had concordance index values of 0.824 and 0.893 in the training and validation cohort, respectively. A: Training cohort; B: Validation cohort.
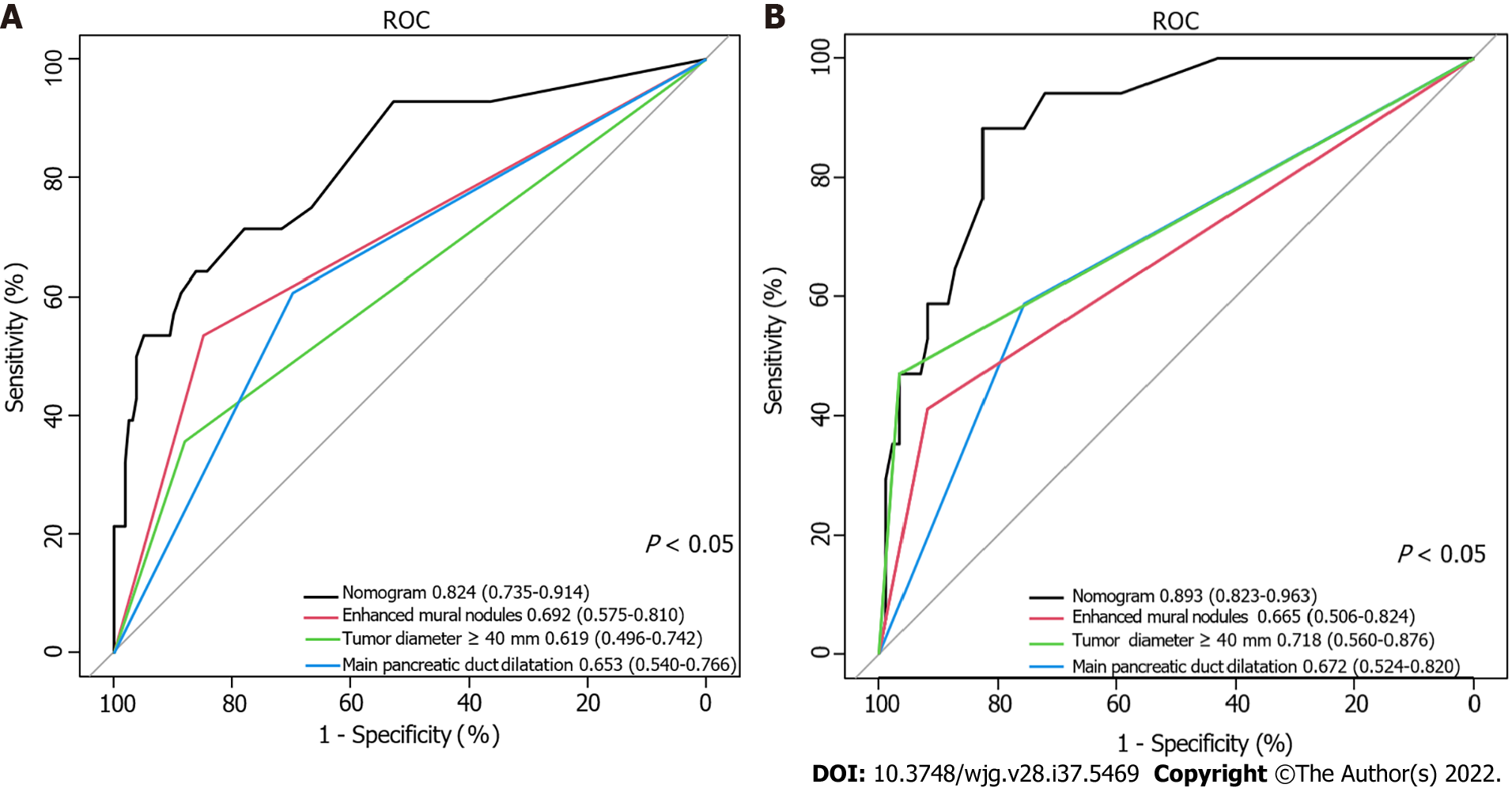
Figure 4 Receiver operating characteristic curve of the nomogram and other three risk factors identified in guidelines.
A: Training cohort; B: Validation cohort. AUC: Area under the curve.
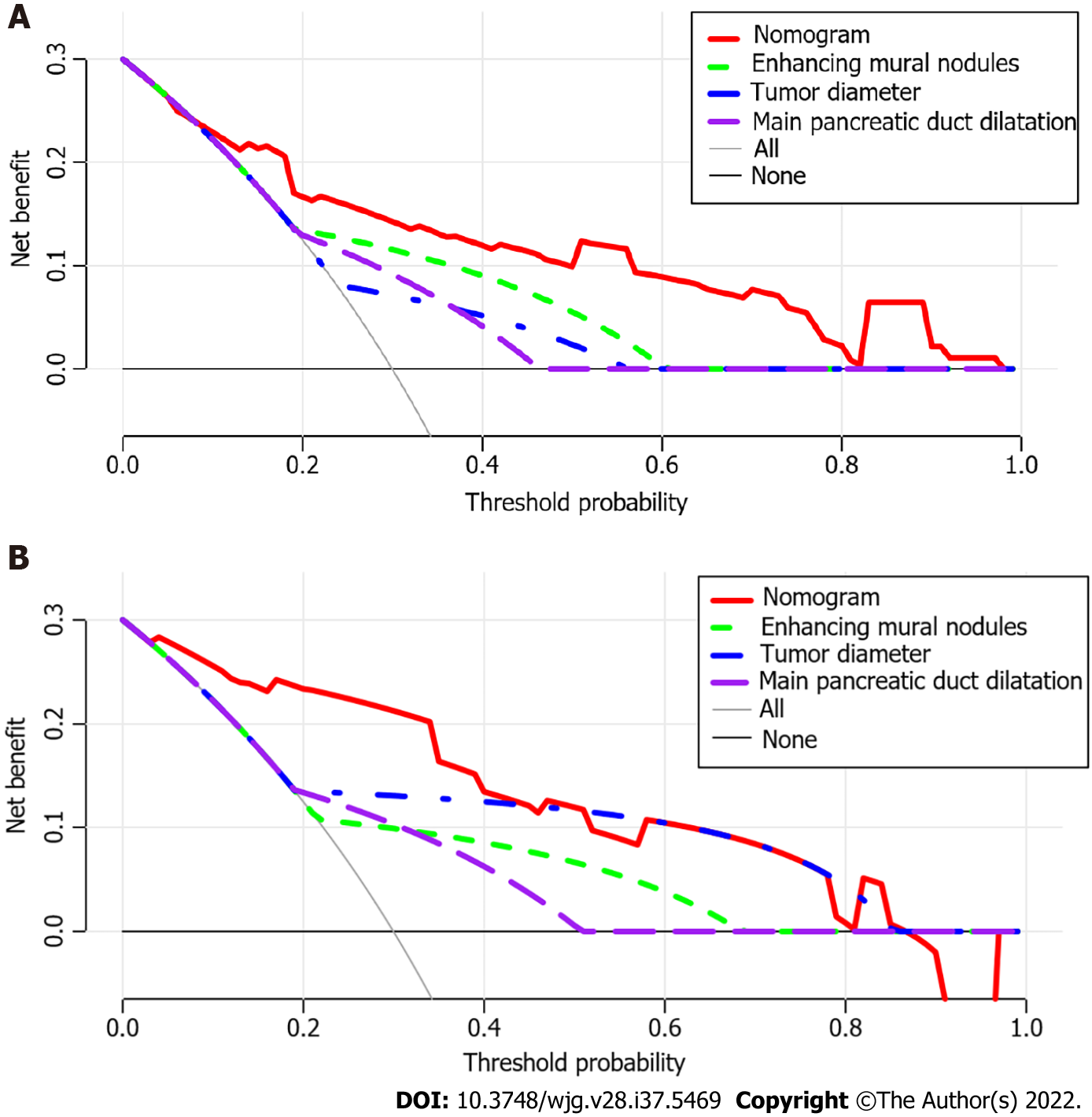
Figure 5 Decision curve analysis of the nomogram and other three risk factors identified in guidelines.
The x-axis represents the threshold probability and the y-axis represents the net benefit. In the training cohort, the nomogram adds more net benefit than the other three factors when the threshold probability ranged from 0.2 to 1.0. In the validation cohort, the nomogram adds more net benefit than the other three factors when the threshold probability ranged from 0.0 to 0.4. A: In the training cohort; B: In the validation cohort.
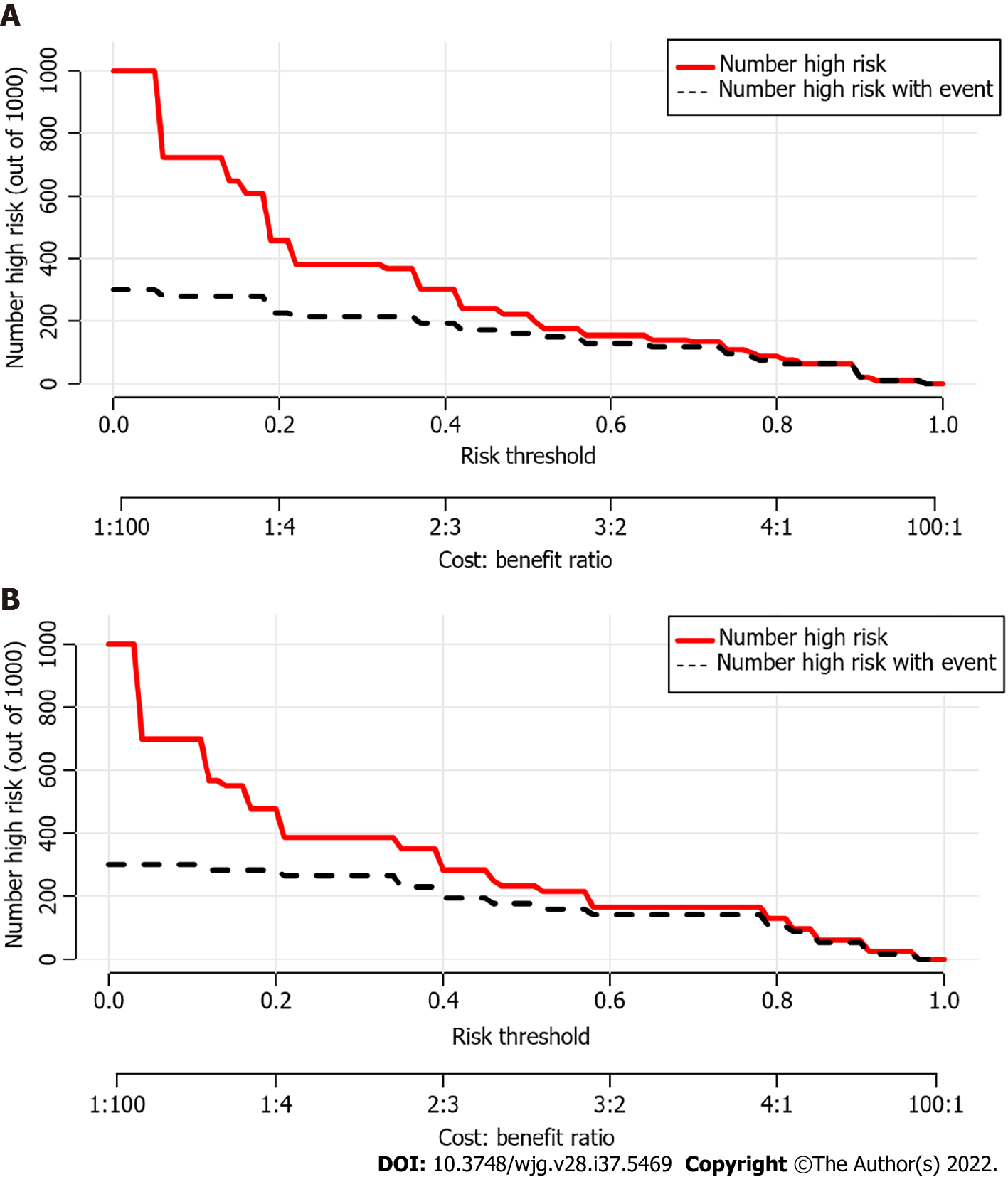
Figure 6 Clinical impact curves of the nomogram.
At different threshold probabilities within a given population, the number of high-risk patients (solid red line) and the number of high-risk patients with the outcome (black dotted line) are shown. In both training and validation cohort, the solid red line and black dotted line show a great fit. A: In the training cohort; B: In the validation cohort.
- Citation: Jiang D, Chen ZX, Ma FX, Gong YY, Pu T, Chen JM, Liu XQ, Zhao YJ, Xie K, Hou H, Wang C, Geng XP, Liu FB. Online calculator for predicting the risk of malignancy in patients with pancreatic cystic neoplasms: A multicenter, retrospective study. World J Gastroenterol 2022; 28(37): 5469-5482
- URL: https://www.wjgnet.com/1007-9327/full/v28/i37/5469.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i37.5469