Copyright
©The Author(s) 2022.
World J Gastroenterol. Aug 28, 2022; 28(32): 4540-4556
Published online Aug 28, 2022. doi: 10.3748/wjg.v28.i32.4540
Published online Aug 28, 2022. doi: 10.3748/wjg.v28.i32.4540
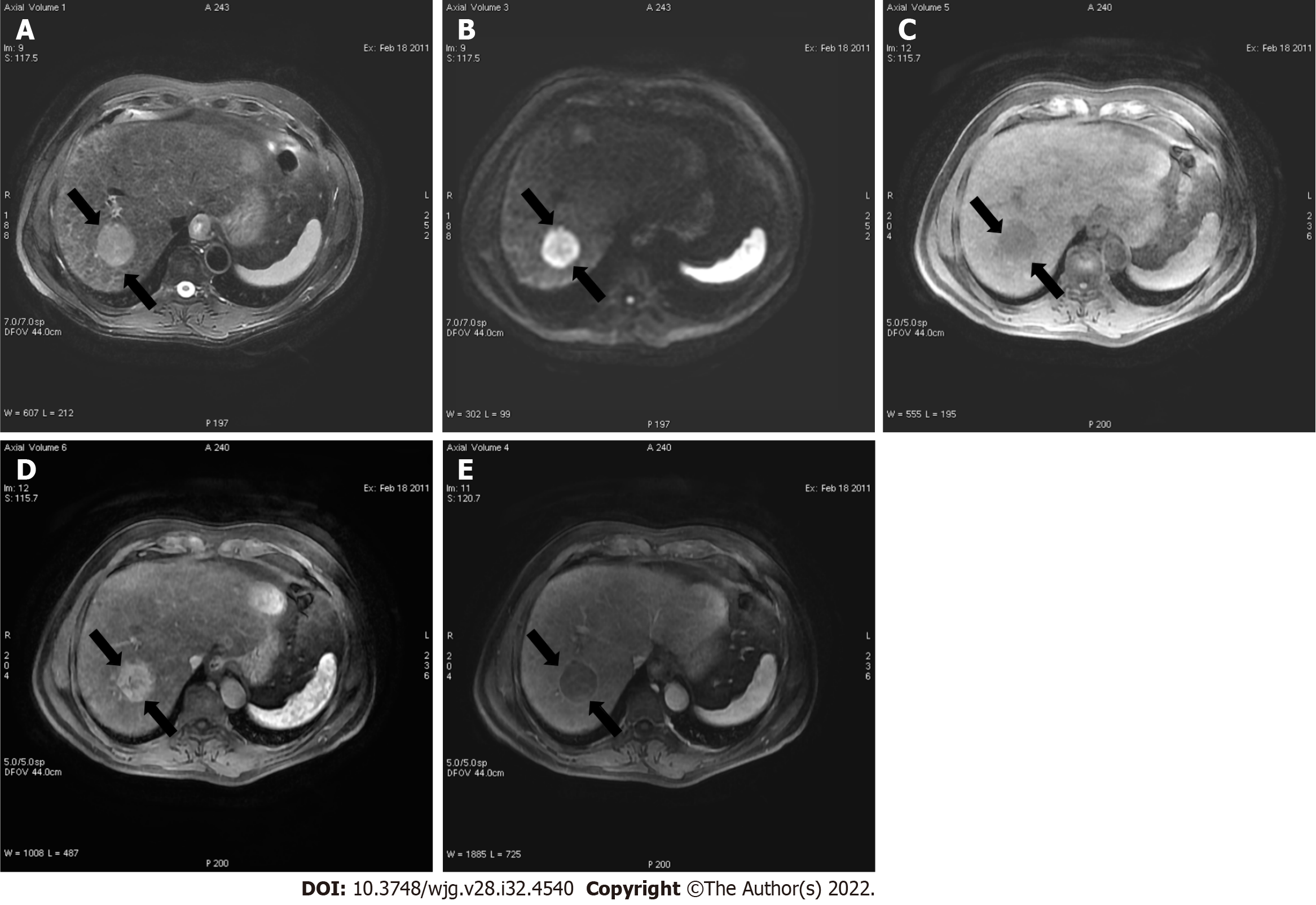
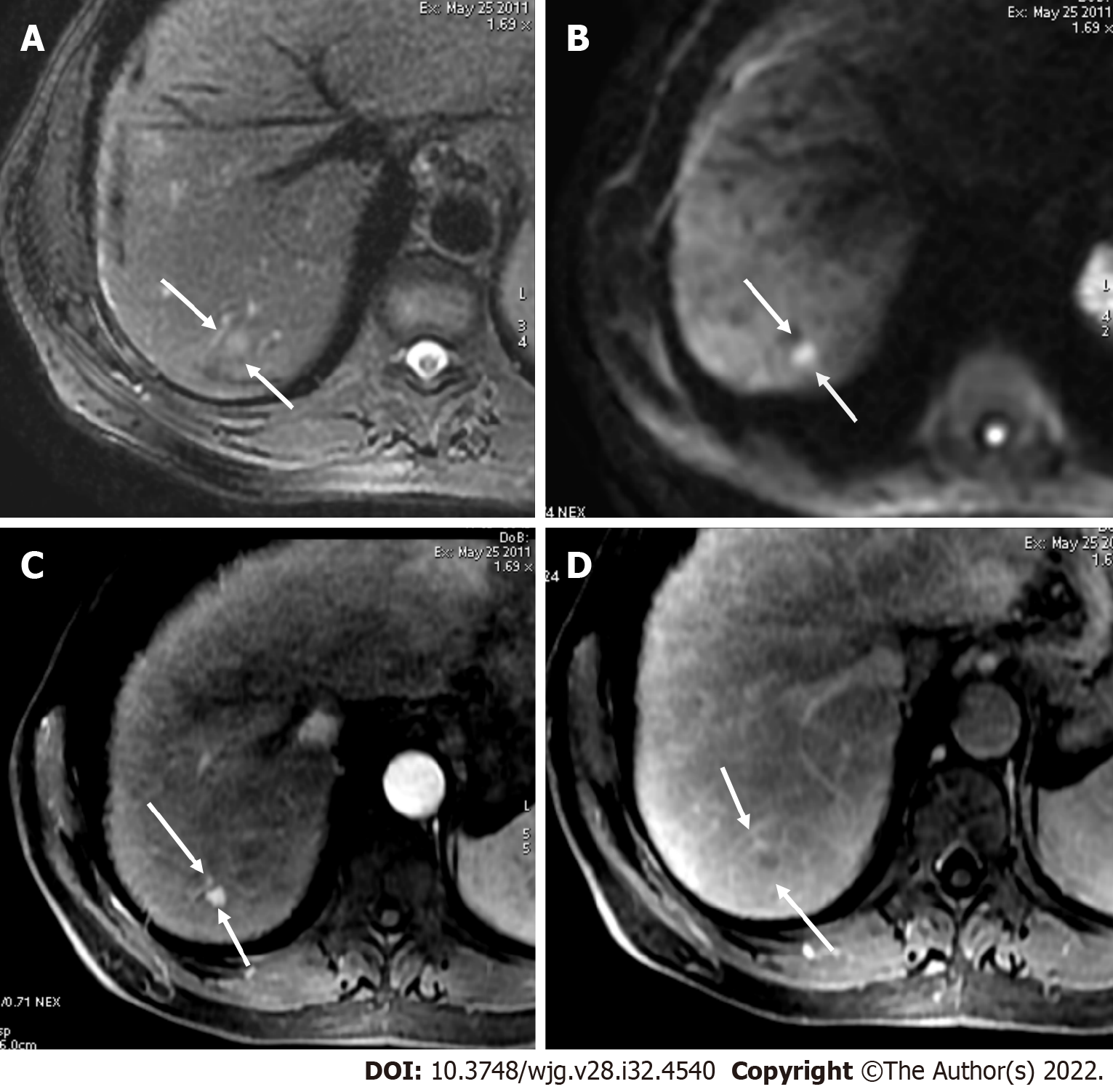
Figure 1 A 52-year-old male with hepatocellular carcinoma and chronic hepatitis B.
A: A segment VII mass showed a high signal on the short tau inversion recovery image; B: High on diffusion-weighted imaging; C: Low on unenhanced volumetric interpolated breath-hold examination image; D: Non-rim arterial phase hyperenhancement on arterial phase; E: Washout and enhancing capsule on portal phase. Lesion showed typical imaging findings of hepatocellular carcinoma categorized as LR-5 according to Liver Imaging Reporting and Data System criteria.
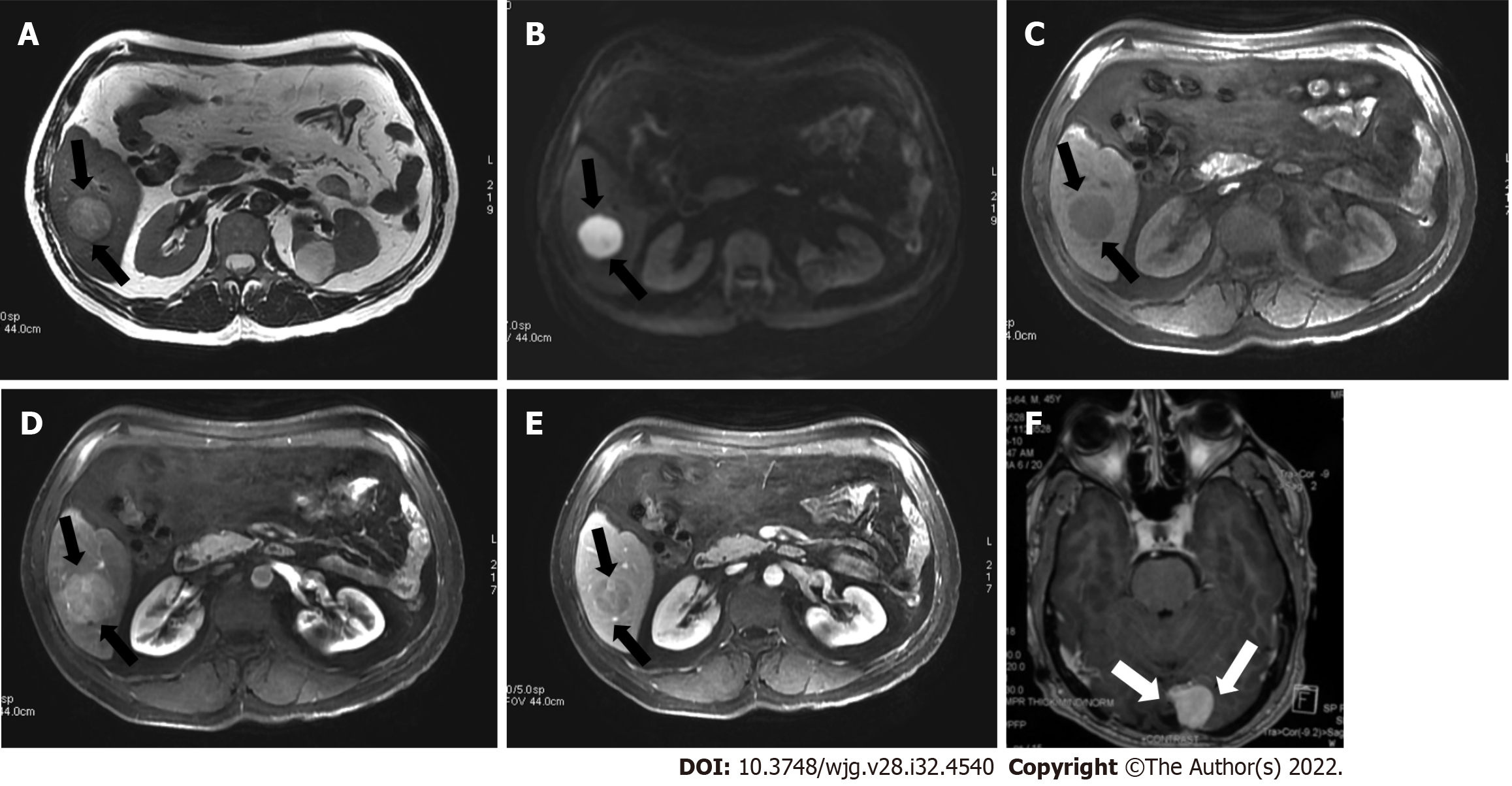
Figure 2 A 45-year-old man with a segment VI lesion.
A: The lesion demonstrated a high signal on T2 weighted image; B: High on diffusion-weighted imaging; C: Low on volumetric interpolated breath-hold examination; D: Non-rim arterial-phase hyper-enhancement on arterial-phase image; E: Washout on portal phase. If we applied Liver Imaging Reporting and Data System (LI-RADS) criteria, the erroneous diagnosis of hepatocellular carcinoma could be made. However, the patient did not meet the at-risk criteria to apply LI-RADS. Histologic examination of the lesion demonstrated metastatic hemangiopericytoma; F: Magnetic resonance imaging of the brain, axial post-contrast T1-weighted image showed an extra-axial lobulated, occipital enhancing mass corresponding to recurrence of hemangiopericytoma 12 mo after total surgical excision.
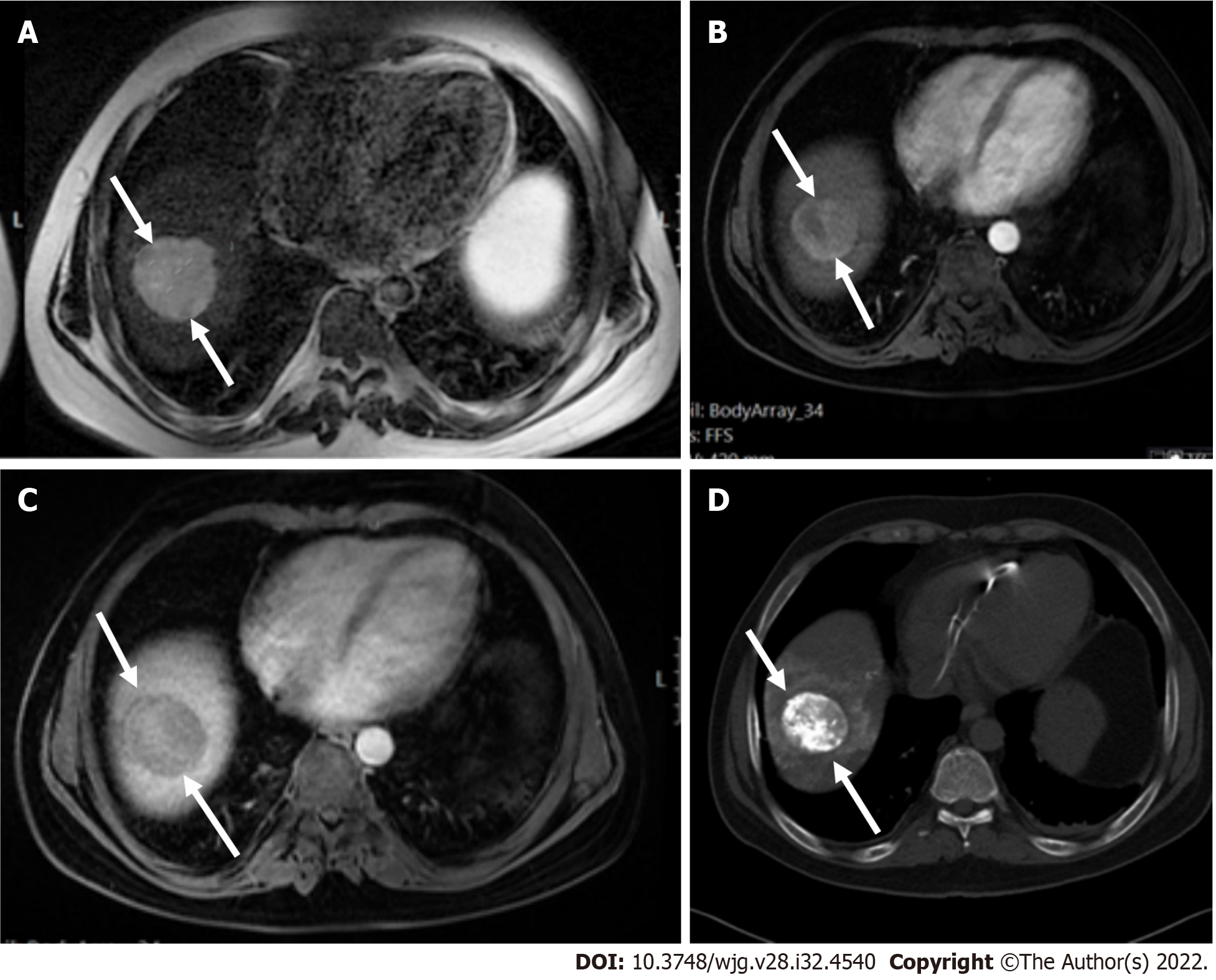
Figure 3 A 47 mm liver mass was incidentally found, in a 40-year-old man with beta thalassemia, during cardiac magnetic resonance investigation for myocardial iron overload.
A-C: On abdominal magnetic resonance imaging, the lesion demonstrated high signal intensity on T2 weighted image (A), arterial phase hyperenhancement on post-contrast arterial phase (B), and washout on portal phase (C). Although there are no current evidence-based guidelines for patients with beta thalassemia without cirrhosis, the hepatologist confirmed the patient’s risk status and proposed that Liver Imaging Reporting and Data System (LI-RADS) should be applied. According to the LI-RADS criteria, the lesion was categorized as LR-5 (definite hepatocellular carcinoma); D: Unenhanced computed tomography scan after transarterial chemoembolization showed accumulation of iodized oil (arrow) within the tumor.
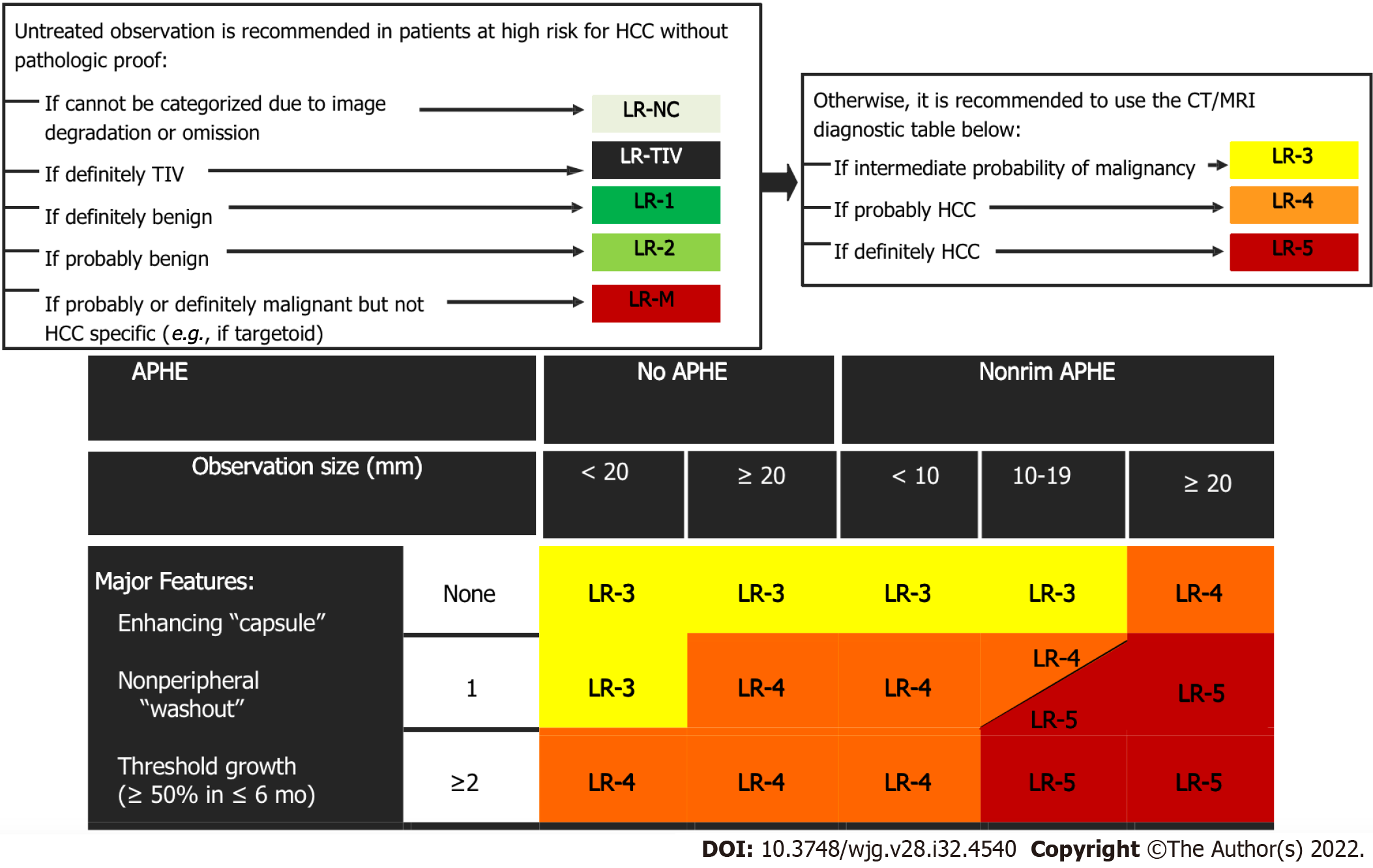
Figure 4 Diagnostic algorithm of liver lesions in computed tomography/magnetic resonance imaging (Liver Imaging Reporting and Data System v2018 CORE).
Observations in the cell LR-4 and LR-5 are categorized based on one additional major feature: LR-4 if enhancing “capsule” and LR-5 if nonperipheral “washout” or threshold growth. APHE: Arterial phase hyperenhancement; CT: Computed tomography; HCC: Hepatocellular carcinoma; MRI: Magnetic resonance imaging; TIV: Tumor in vein.
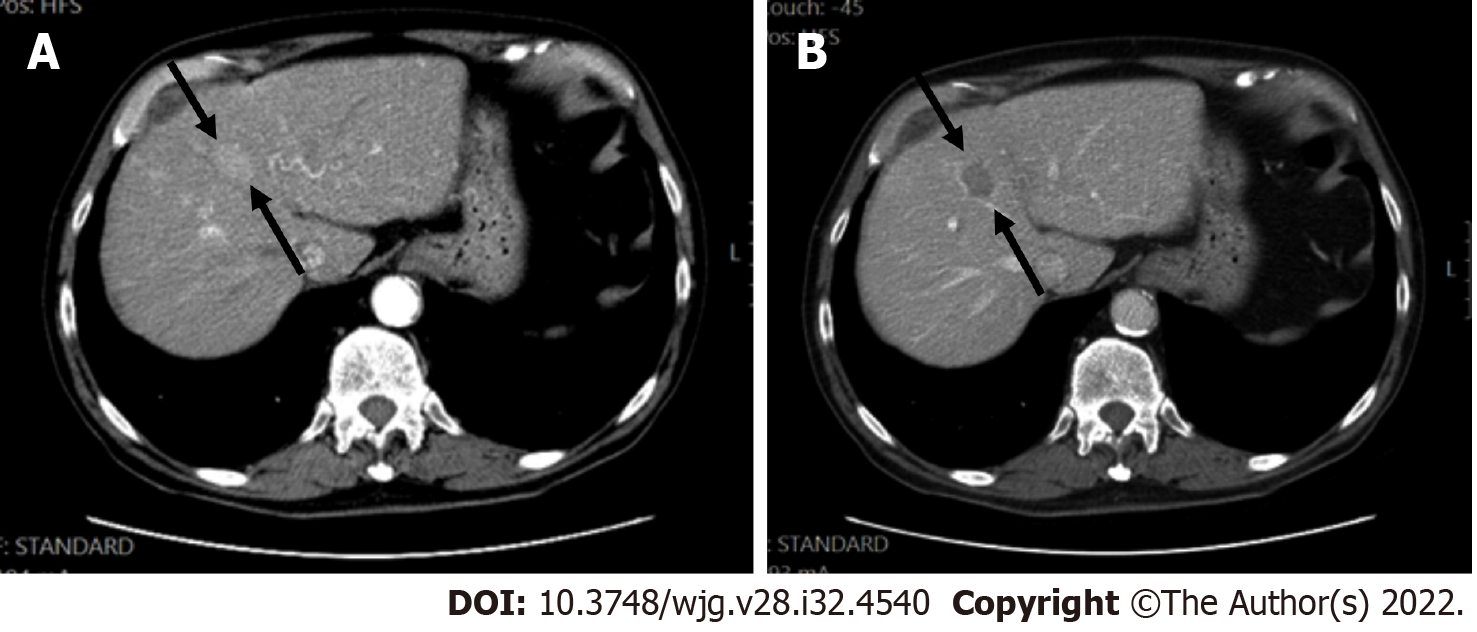
Figure 5 Hepatocellular carcinoma in a 60-year-old man with hepatitis C.
A: Computed tomography scan, late arterial phase were the hepatic artery and portal vein are both enhanced, showed a segment VIII lesion measuring 27 mm with non-rim arterial phase hyper-enhancement; B: In the portal phase, washout was seen.
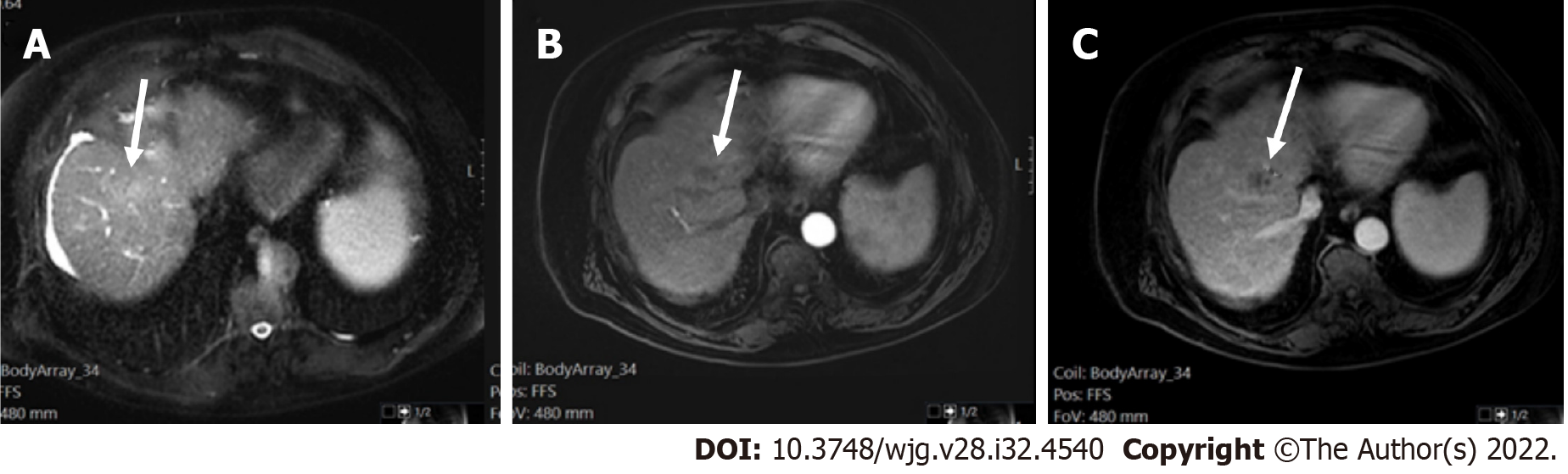
Figure 6 LR-non-categorizable category.
Magnetic resonance imaging in a 74-year-old man with hepatitis C. A: Axial short tau inversion recovery shows an observation in segment VIII with high signal intensity (arrow) within a nodular liver consistent with cirrhosis; On arterial post-contrast image (Β) and on portal phase (C) (arrows) the observation shows low signal intensity. However the arterial phase is early to characterize a possible arterialized lesion (LR-NC category).
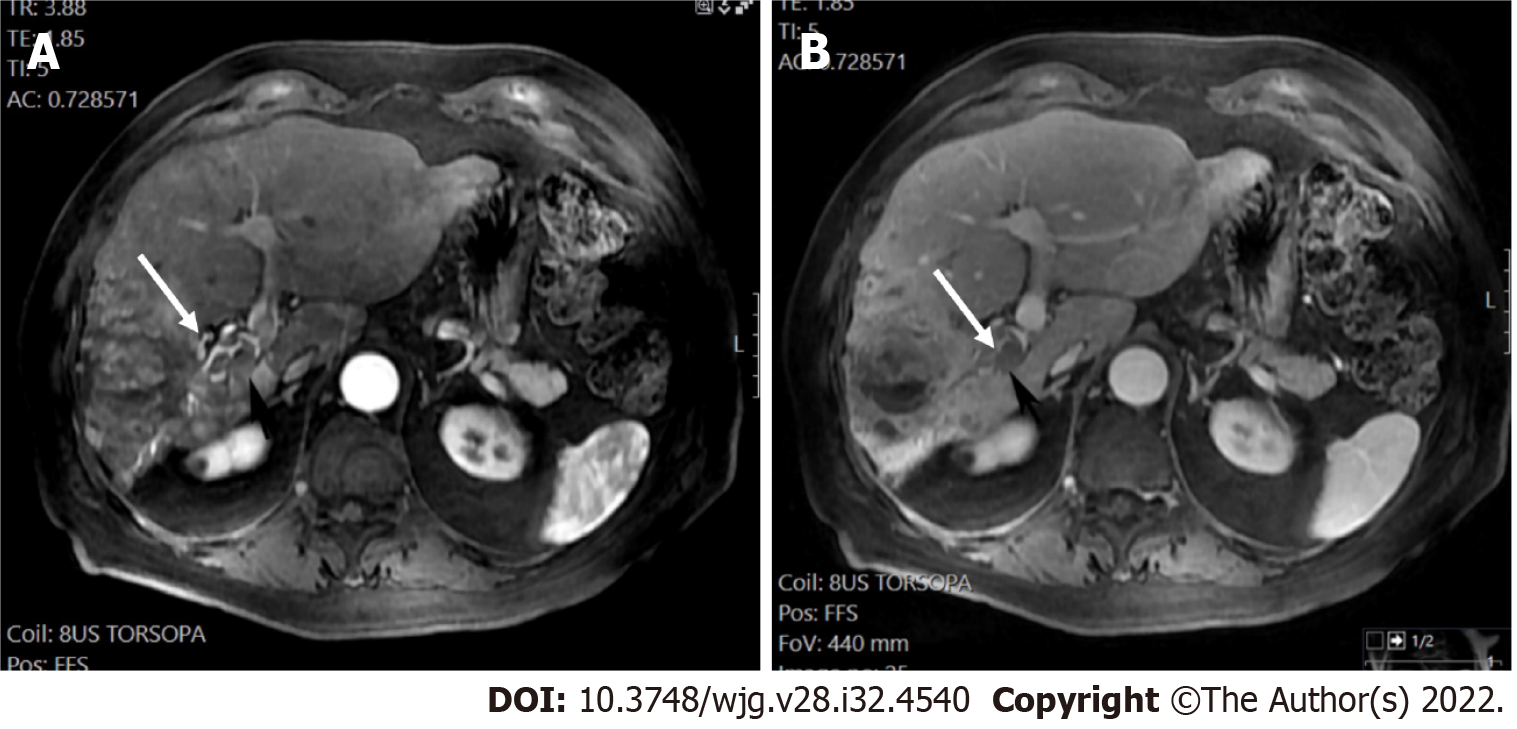
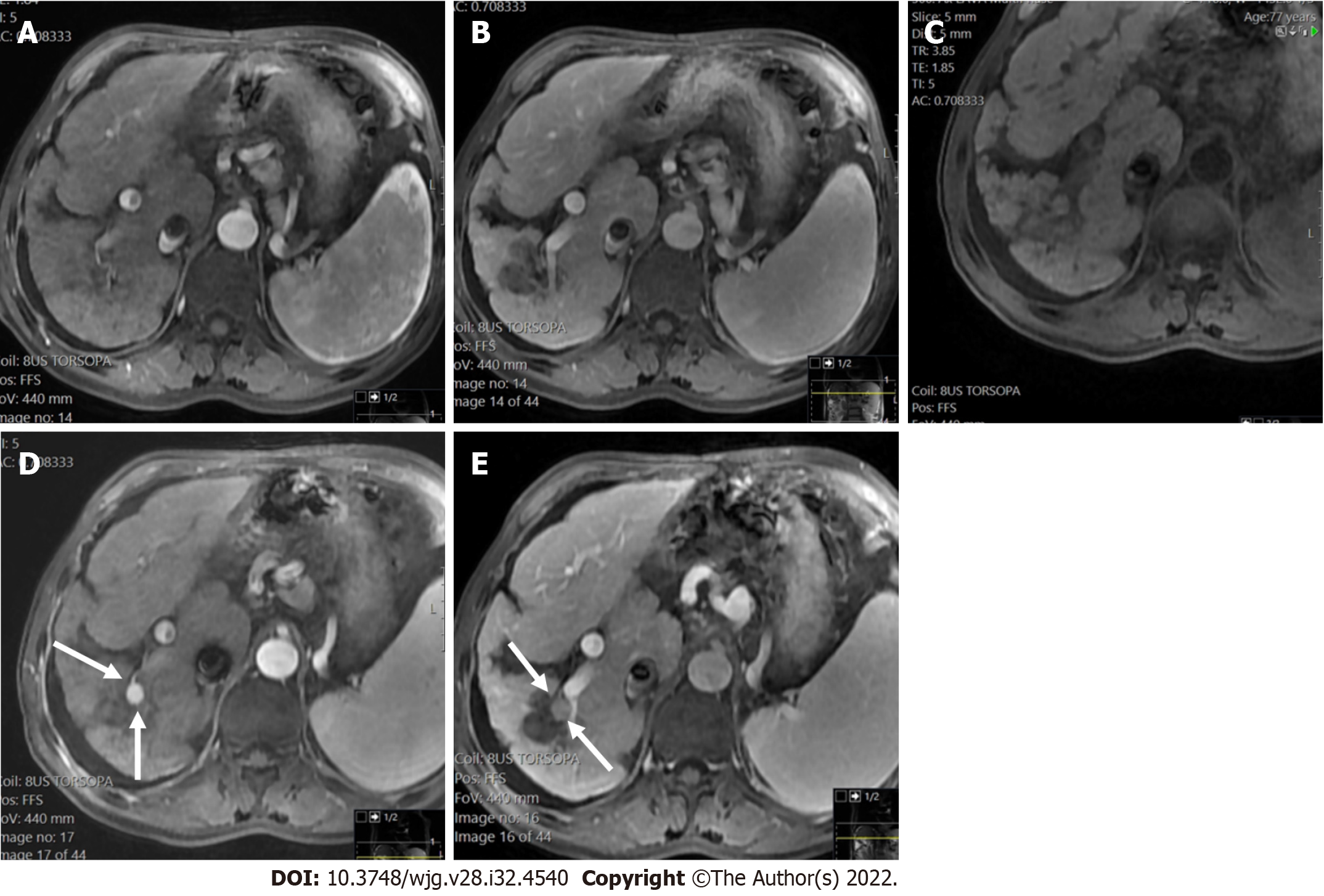
Figure 7 LR-tumor in vein (definite tumor in vein) in a 70-year-old man with alcoholic liver cirrhosis.
Magnetic resonance imaging arterial phase and portal venous phase demonstrated a large inhomogeneous enhancing mass with definite enhancing soft tissue extending to the right portal vein (arrows). A: Magnetic resonance imaging arterial phase; B: Portal venous phase.
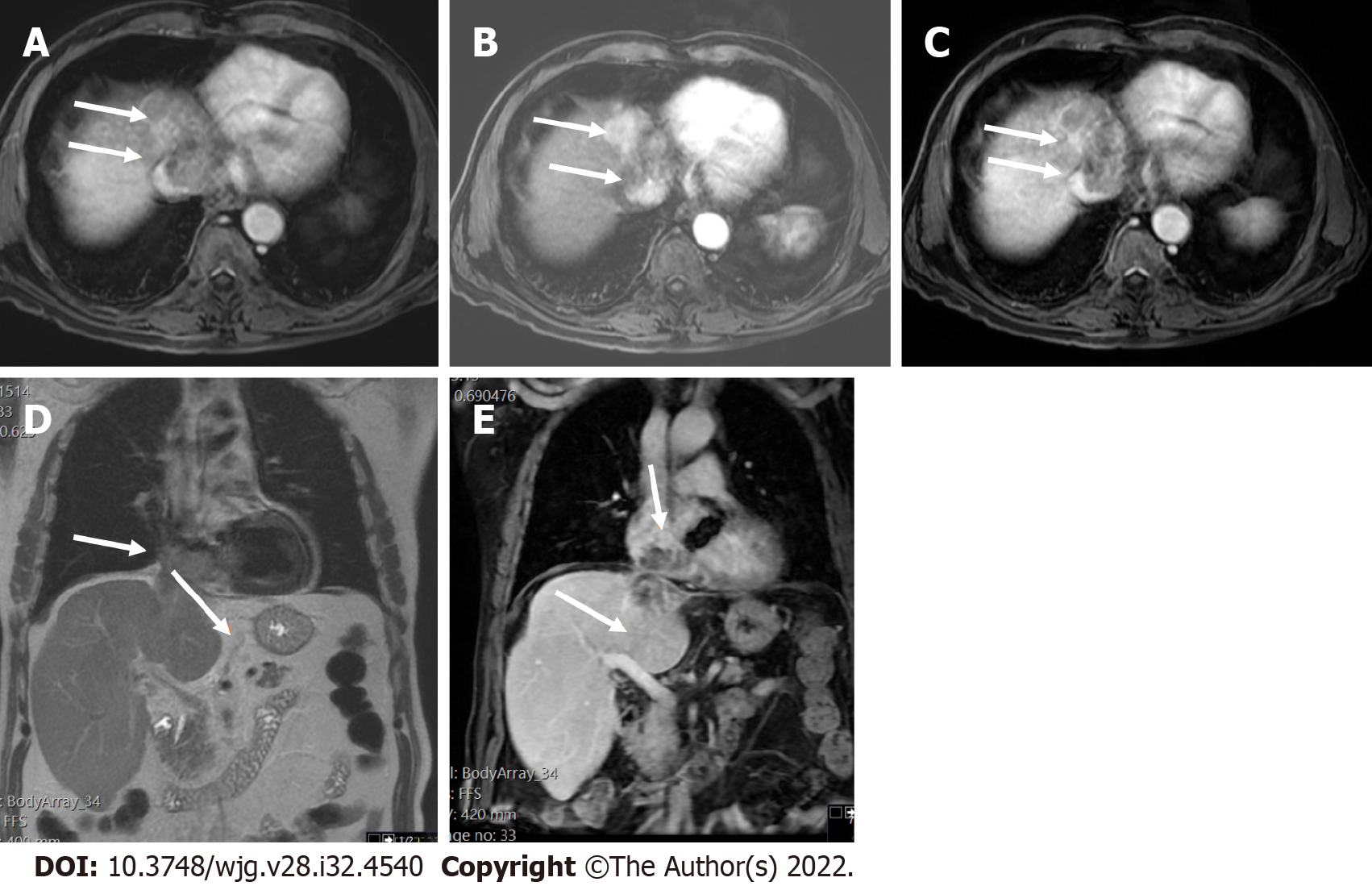
Figure 8 Two-dimensional transthoracic echocardiogram revealed a mobile right atrial mass protruding from the inferior vena cava, in a patient with chronic hepatitis B and cirrhosis.
A-C: Axial T1 weighted image (T1WI) (A), arterial post-contrast (B) and portal phase (C) showed direct right atrial extension of hepatic segment VIII-IVA tumor through the inferior vena cava, categorized as LR-tumor in vein (arrows); D and E: Coronal T2 weighted image (D) and coronal post-contrast T1WI (E) showed better craniocaudal tumor extension (arrows).
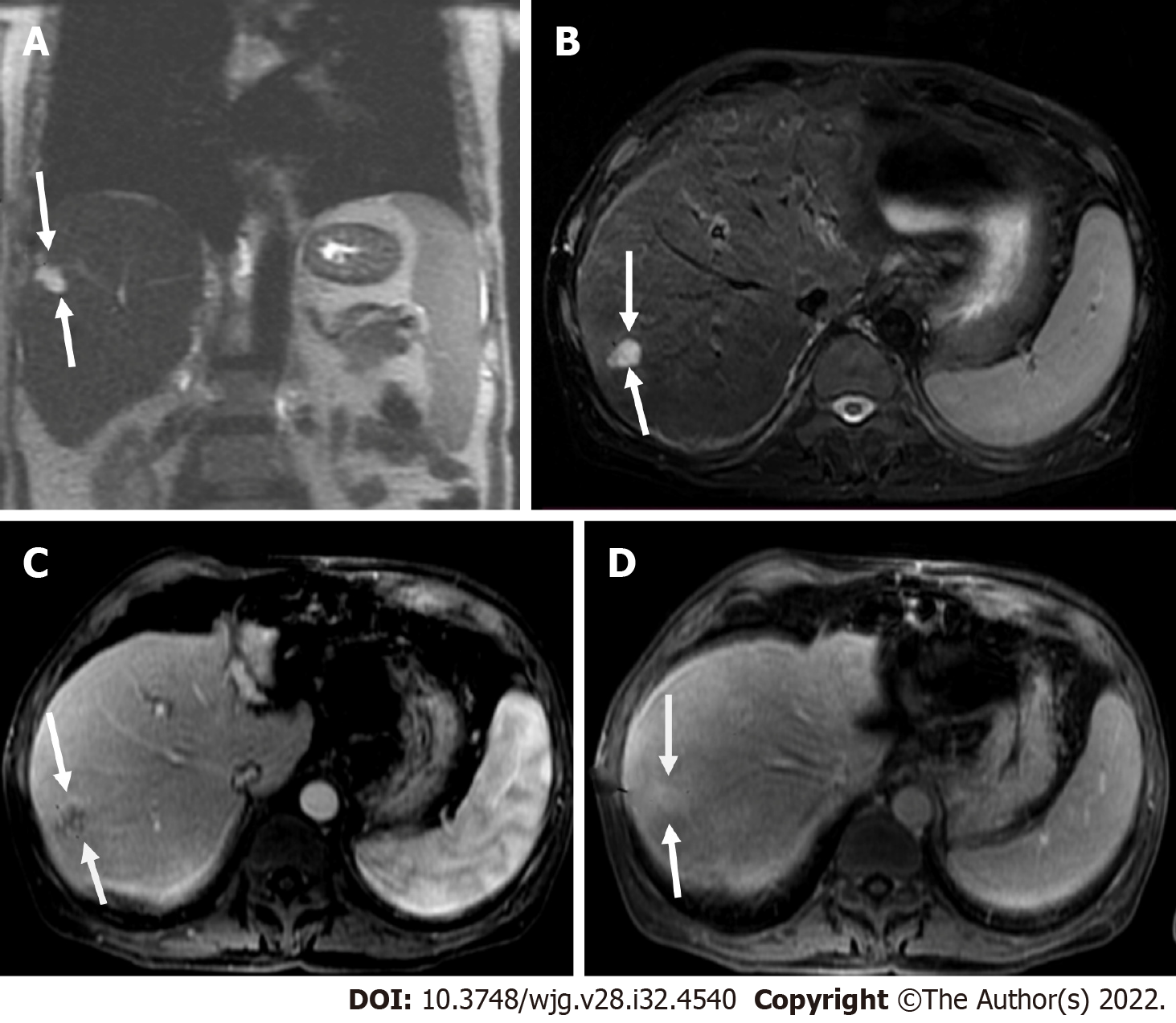
Figure 9 Coronal T2 weighted image and axial short tau inversion recovery image.
A and B: Coronal T2 weighted image (T2WI) (A) and axial short tau inversion recovery image (B) showed a 2 cm lesion in segment VII with high signal intensity (bright) within a nodular liver consistent with cirrhosis; C: Post-contrast image showed nodular peripheral enhancement; D: On delay image, the lesion showed progressive filling. In progressive cirrhosis, hemangiomas are likely to decrease in size, become more fibrotic, and are difficult to diagnose radiologically. However, the bright signal on T2WI and the enhancement pattern was pathognomonic for hemangioma of the liver consistent with LR-2.
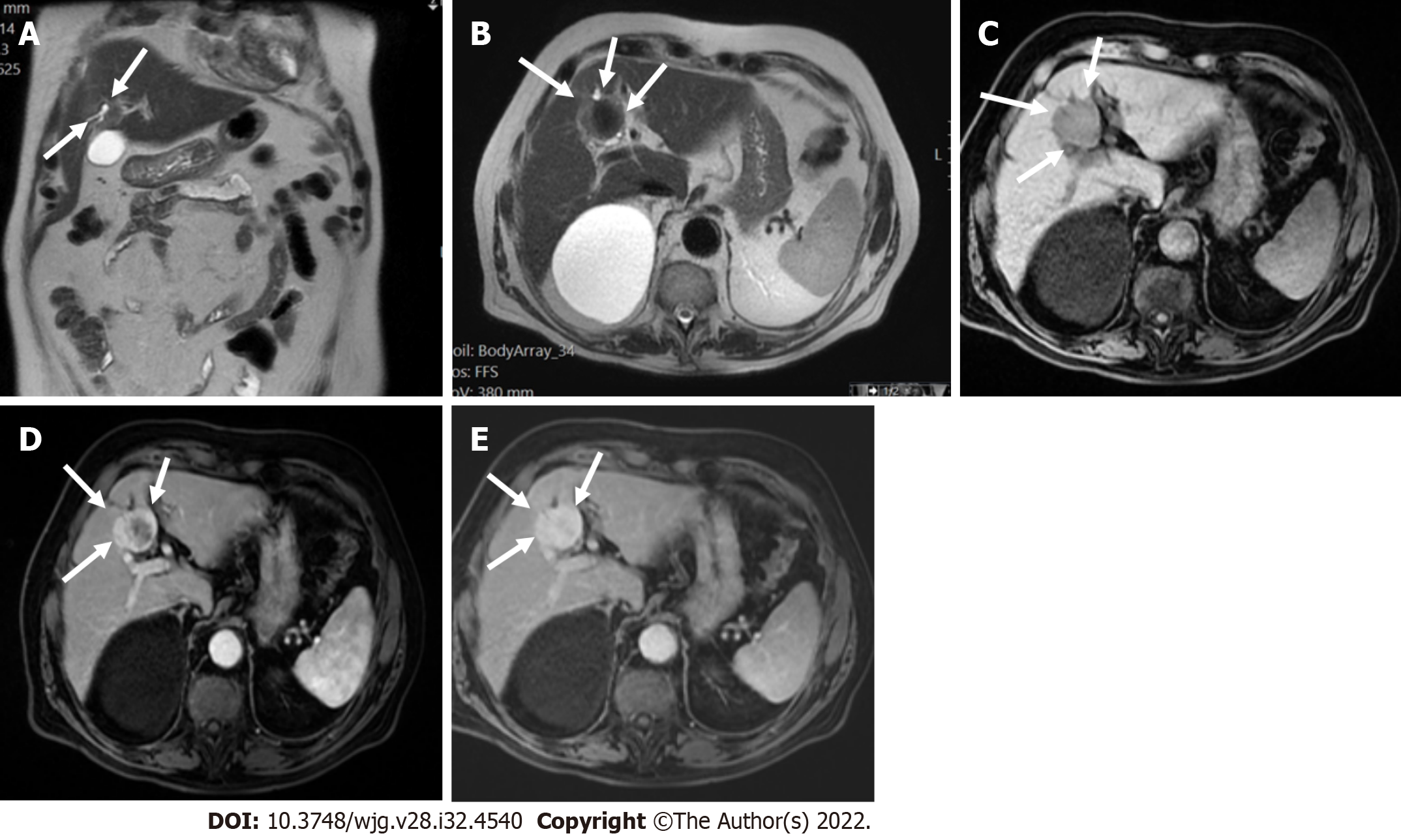
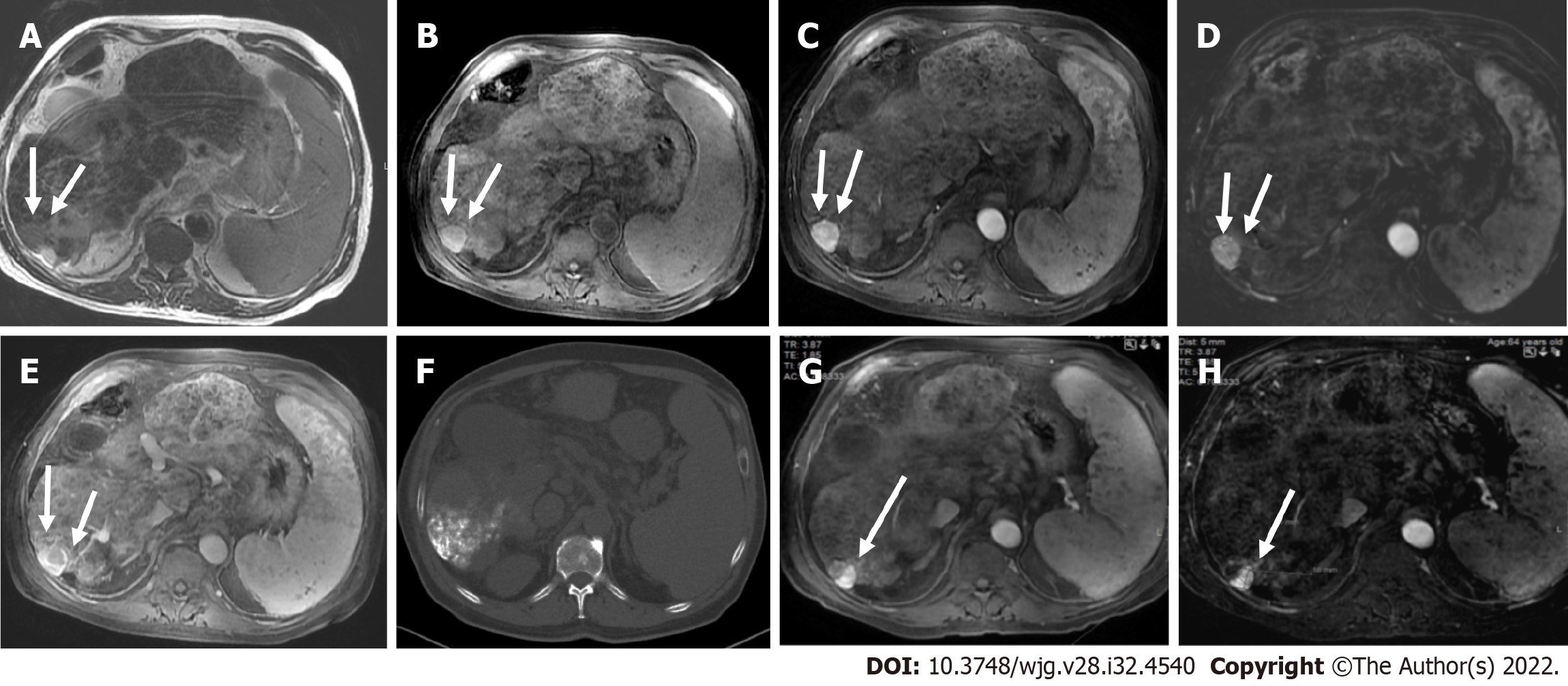
Figure 10 T1 weighted image and T2 weighted image.
A and B: Coronal (A) and axial (B) T2 weighted images showed a low signal segment V mass in a patient with chronic hepatitis B (arrows); C: The mass showed low signal intensity (arrows) on T1 weighted image; D and E: In the arterial phase (D), there was peripheral enhancement (arrows) and progressive filling (arrows) in the portal phase (E) categorized as LR-M. Histologic examination confirmed the diagnosis of cholangiocarcinoma and not hepatocellular carcinoma.
Figure 11 T2 weighted image and volumetric interpolated breath-hold examination.
A and B: Axial T2 weighted image (A) and volumetric interpolated breath-hold examination (VIBE) (B) showed a shrunken and nodular liver that was consistent with cirrhosis; C and D: On post-contrast VIBE arterial-phase image (C), a 1.6 cm lesion in segment IVb demonstrated hyperenhancement (arrows) without washout on portal venous phase image (D). According to Liver Imaging Reporting and Data System criteria, the lesion was categorized as LR-3.
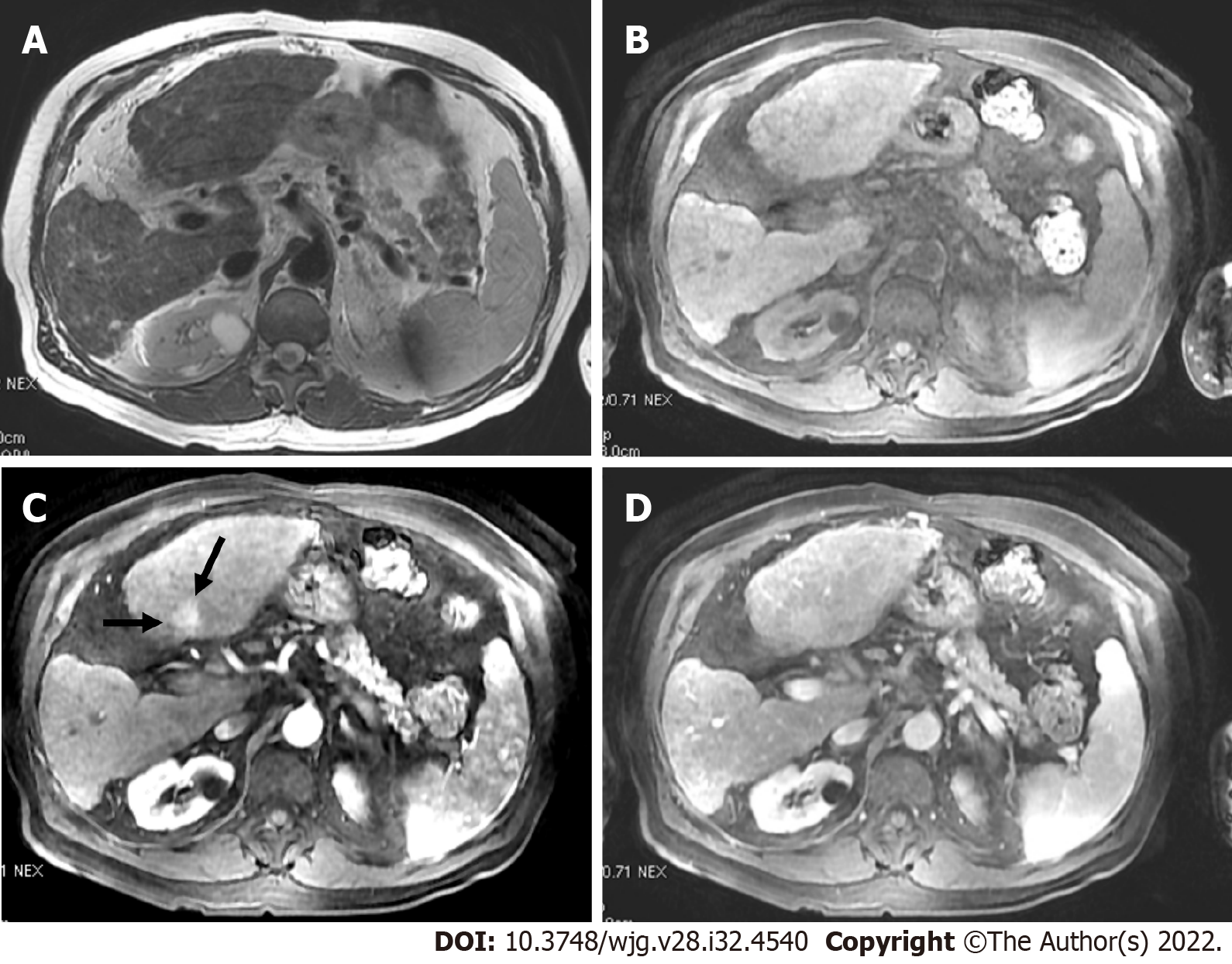
Figure 12 Axial short tau inversion recovery image.
A and B: A IVa segment observation with low signal intensity (arrows) measuring > 20 mm (A) and high signal intensity on pre-contrast image (arrows on B); C and D: On arterial (C) and portal (D) phase there was no arterial phase hyperenhancement or washout and the lesion was categorized as LR-3.
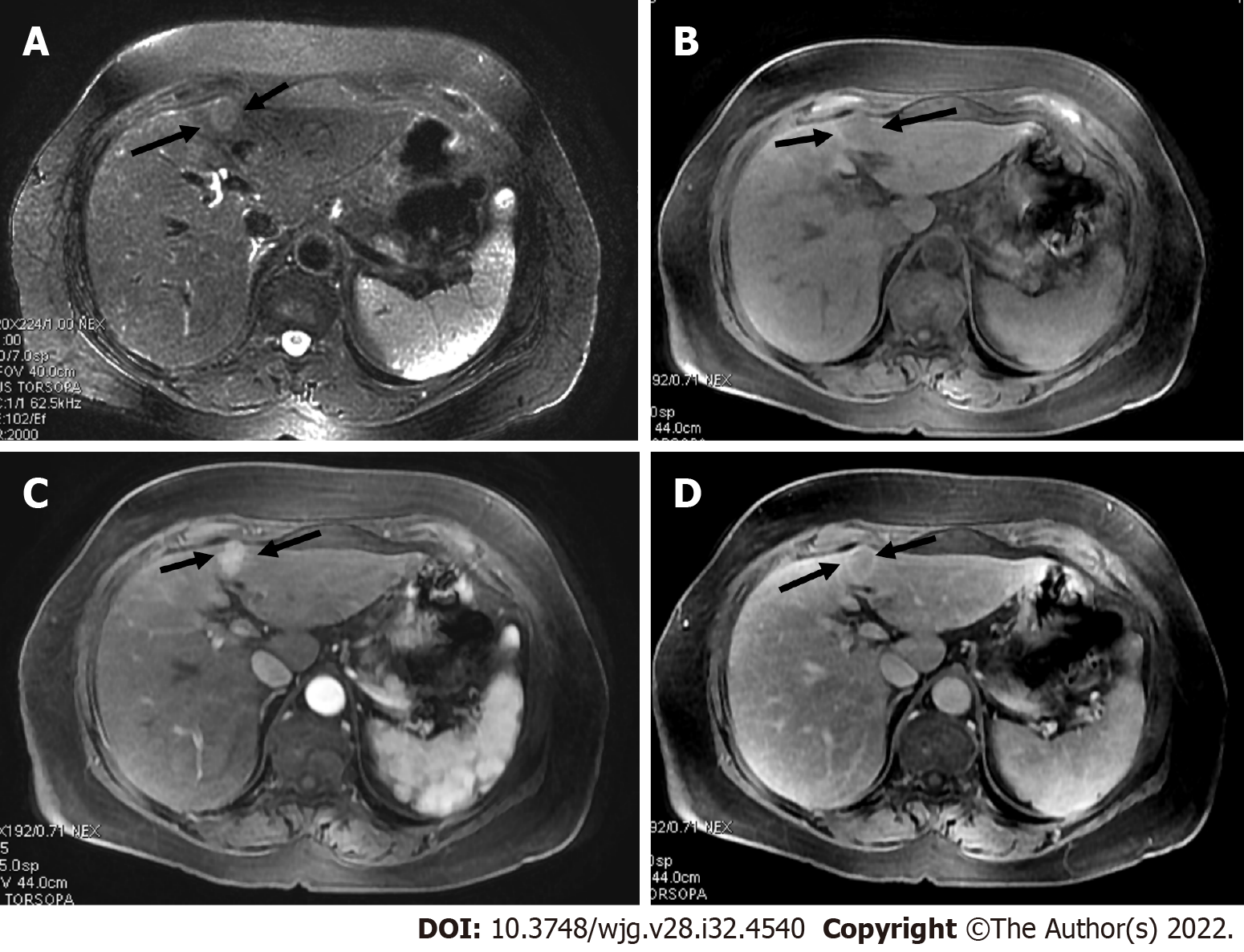
Figure 13 Axial short tau inversion recovery and diffusion-weighted imaging.
A and B: Axial short tau inversion recovery (A) and diffusion-weighted imaging (DWI) (B) images showed a < 10 mm segment VII observation with high signal intensity; C and D: In the arterial phase (C), arterial phase hyperenhancement was seen with washout in the portal phase (D) categorized as LR-4. Restriction on DWI does not allow to upgrade from LR-4 to LR-5, because ancillary features lack sufficient specificity for hepatocellular carcinoma to allow for an LR-5 upgrade.
Figure 14 A 62-year-old female with chronic hepatitis C.
A: On axial short tau inversion recovery image, a 21 mm IVb segment observation with relative high signal intensity is seen (arrows); B: On axial volumetric interpolated breath-hold examination image the observation shows low signal intensity (arrows); C and D: On post-contrast images, major features of hepatocellular carcinoma (HCC), arterial phase hyperenhancement (arrows) on arterial phase (C), washout and enhancing capsule (arrows) on portal (D) were seen, indicating LR-5 (definitely HCC).
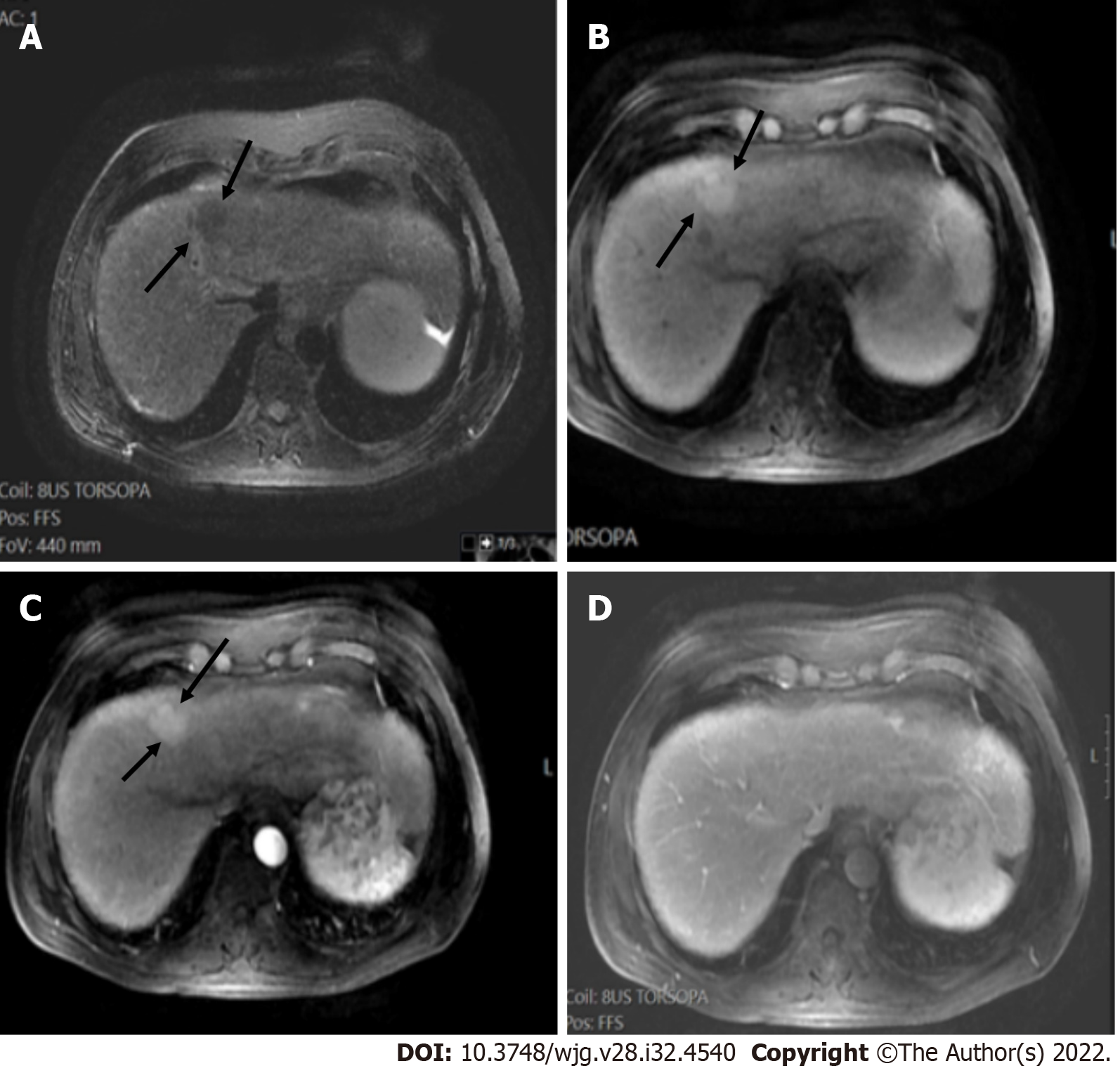
Figure 15 A 60-year-old male with hepatitis B and cirrhosis.
A and B: A < 10 mm segment II observation demonstrated arterial phase hyperenhancement (APHE) (arrows) on arterial post-contrast images (A) without washout (B), categorized as LR-3 observation; C and D: 1-year later, the observation measured 18 mm, showed APHE (arrows) in the arterial phase (C) without definite washout in the portal phase (D). However due to threshold growth, it was categorized as LR-5.
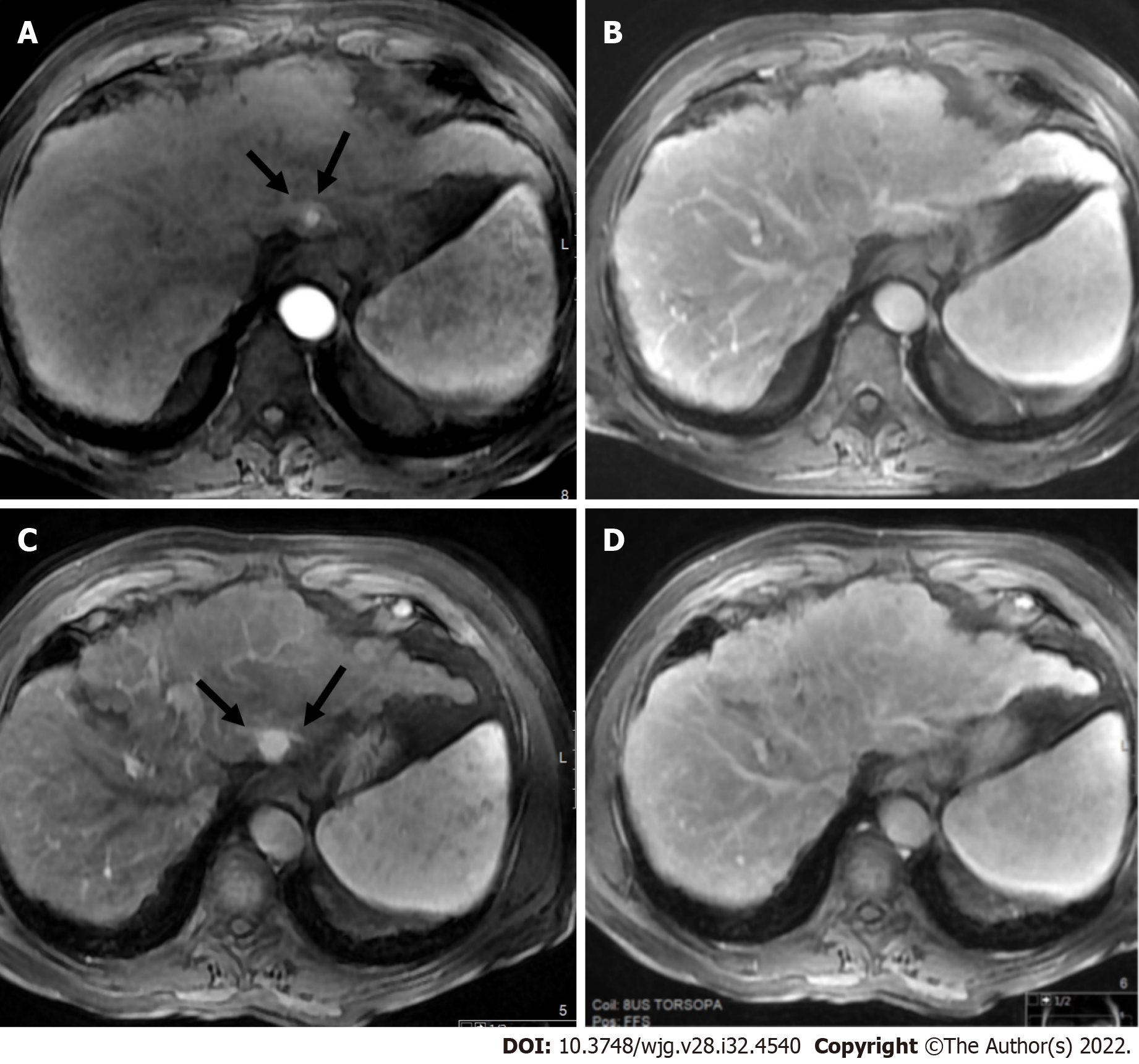
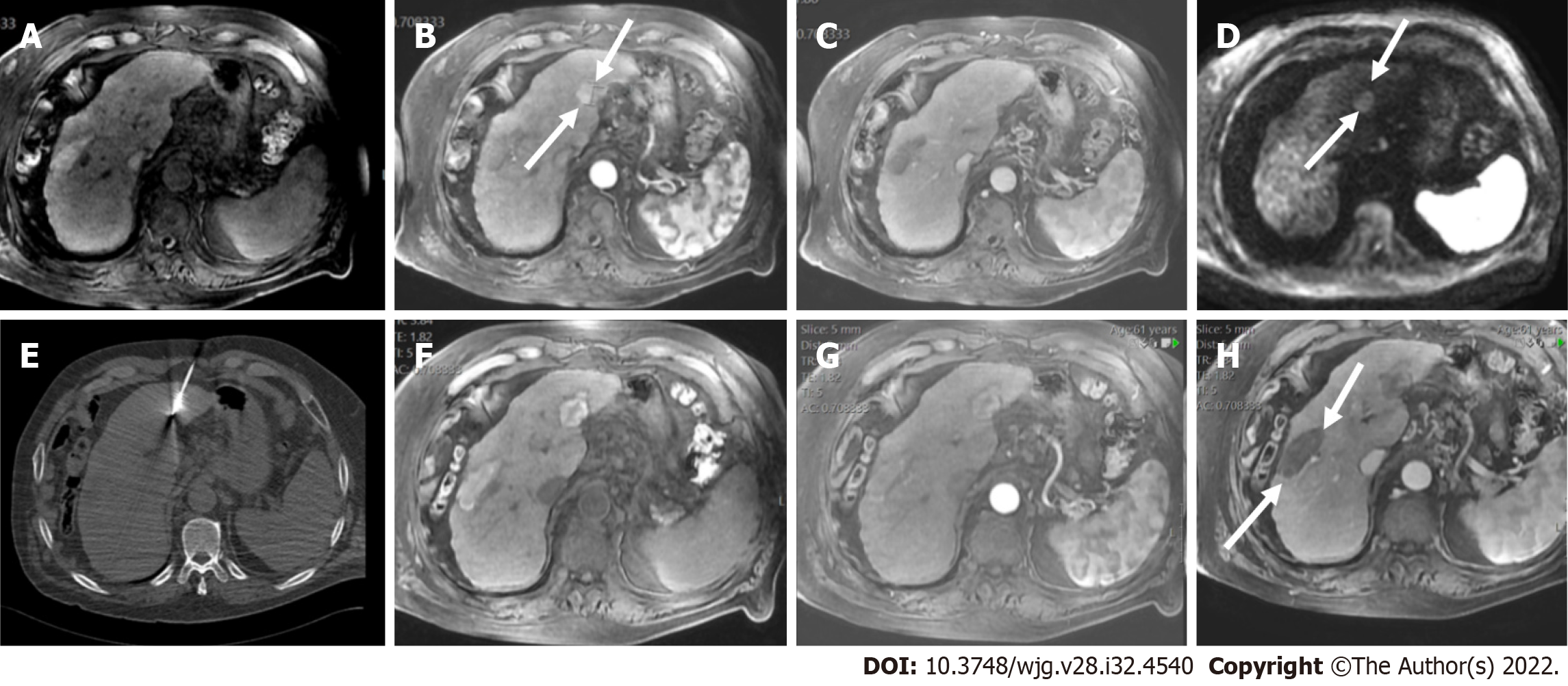
Figure 16 LR-5 observation.
A and B: Axial short tau inversion recovery (A) and T2 weighted (B) showed a segment VI observation with relative high signal intensity (arrows); C: On pre-contrast volumetric interpolated breath-hold examination image, peripherally high signal was seen; D: In the arterial phase, multiple hyperenhanced nodules within nodule were seen (arrows); E: In the portal phase, segmental washout was seen (arrows) categorized as LR-5.
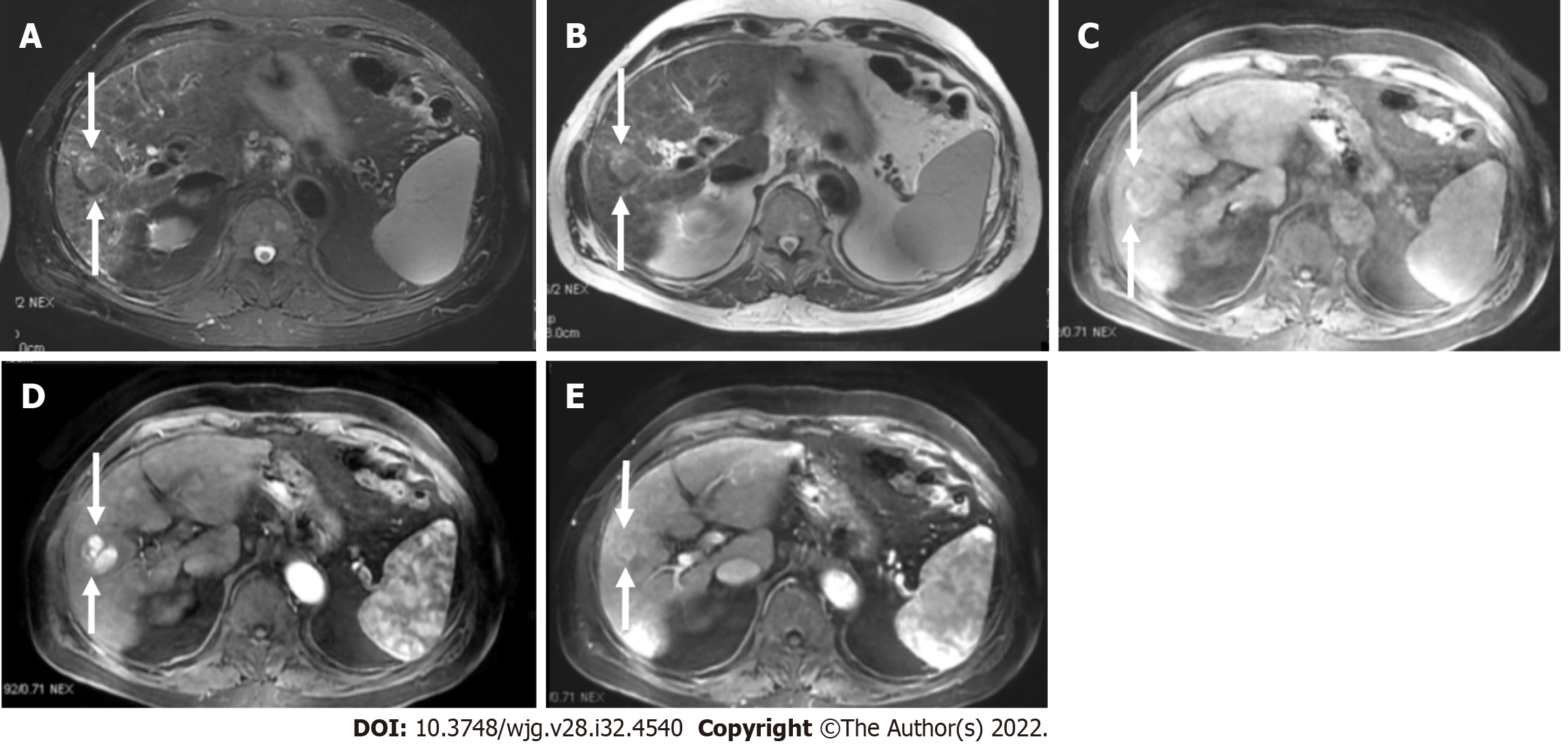
Figure 17 LR-5 observation.
A and B: Axial post-contrast images arterial (A) and portal phase (B) showed an ablation defect in segment VI without residual areas of arterial enhancement or washout. This was classified as LR-treatment response non-viable; C-E: Later pre-contrast (C) arterial (D) and portal (E) phase showed a new nodule (arrows) measuring 12 mm with strong arterial enhancement and washout categorized as LR-5. If a new tumor arises within or adjacent to a treated lesion, this observation should be assigned a new non-treated LI-RADS category.
Figure 18 LR-5 observation.
A and B: Axial T2 weighted (A) and volumetric interpolated breath-hold examination (B) show a segment VI observation with high signal intensity (arrows); C and D: On arterial phase (C) strong enhancement is seen, better depicted on subtracted image (D); E: On portal phase washout is seen categorized as LR-5; F: Unenhanced computed tomography scan after TACE shows accumulation of iodized oil (arrow) within the tumor; G and H: However on post-contrast follow up magnetic resonance imaging on arterial phase (G) there is residual nodular enhancement within a lesion clearly depicted on subtracted image (H) categorized as LR-treatment response viable.
Figure 19 Axial volumetric interpolated breath-hold examination, arterial phase.
A-C: Axial volumetric interpolated breath-hold examination (A), arterial phase (B) showed an observation measuring almost 20 mm with arterial phase hyperenhancement (arrows) without washout on portal image (C) categorized as LR-4; D and E: On diffusion-weighted imaging (D), the observation showed high signal intensity (arrows) but the ancillary features lacked sufficient specificity for hepatocellular carcinoma to allow for an LR-5 upgrade. After multidisciplinary discussion, ablation was performed (E); F-H: On follow-up, an ablation defect was seen without residual areas of arterial enhancement or washout. This was classified as LR-treatment response non-viable. Note a previous ablation defect in the right lobe (arrows).
- Citation: Liava C, Sinakos E, Papadopoulou E, Giannakopoulou L, Potsi S, Moumtzouoglou A, Chatziioannou A, Stergioulas L, Kalogeropoulou L, Dedes I, Akriviadis E, Chourmouzi D. Liver Imaging Reporting and Data System criteria for the diagnosis of hepatocellular carcinoma in clinical practice: A pictorial minireview. World J Gastroenterol 2022; 28(32): 4540-4556
- URL: https://www.wjgnet.com/1007-9327/full/v28/i32/4540.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i32.4540