Copyright
©The Author(s) 2022.
World J Gastroenterol. Jan 21, 2022; 28(3): 275-289
Published online Jan 21, 2022. doi: 10.3748/wjg.v28.i3.275
Published online Jan 21, 2022. doi: 10.3748/wjg.v28.i3.275
Figure 1 Authors.
A: Andrzej S Tarnawski, Gastroenterology Research Department, University of California Irvine and the Veterans Administration Long Beach Healthcare System, Long Beach, CA 90822, United States; B: Amrita Ahluwalia, Research Service, Veterans Administration Long Beach Healthcare System, Long Beach, CA 90822, United States.
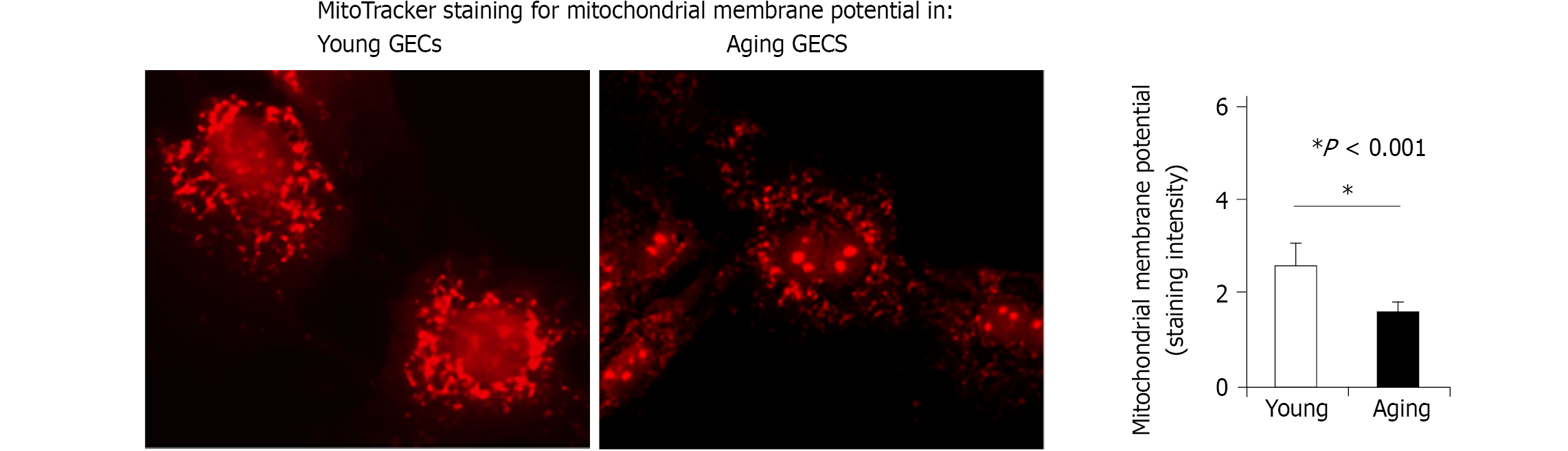
Figure 2 Mitotracker staining for mitochondrial membrane potential in young gastric endothelial cells and aging gastric endothelial cells.
Aging gastric endothelial cells (GECs) have significantly reduced mtMP reflecting impaired mitochondrial function vs young GECs [reproduced with permission from reference[20], which is an open-access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/)]. GECs: Gastric endothelial cells.
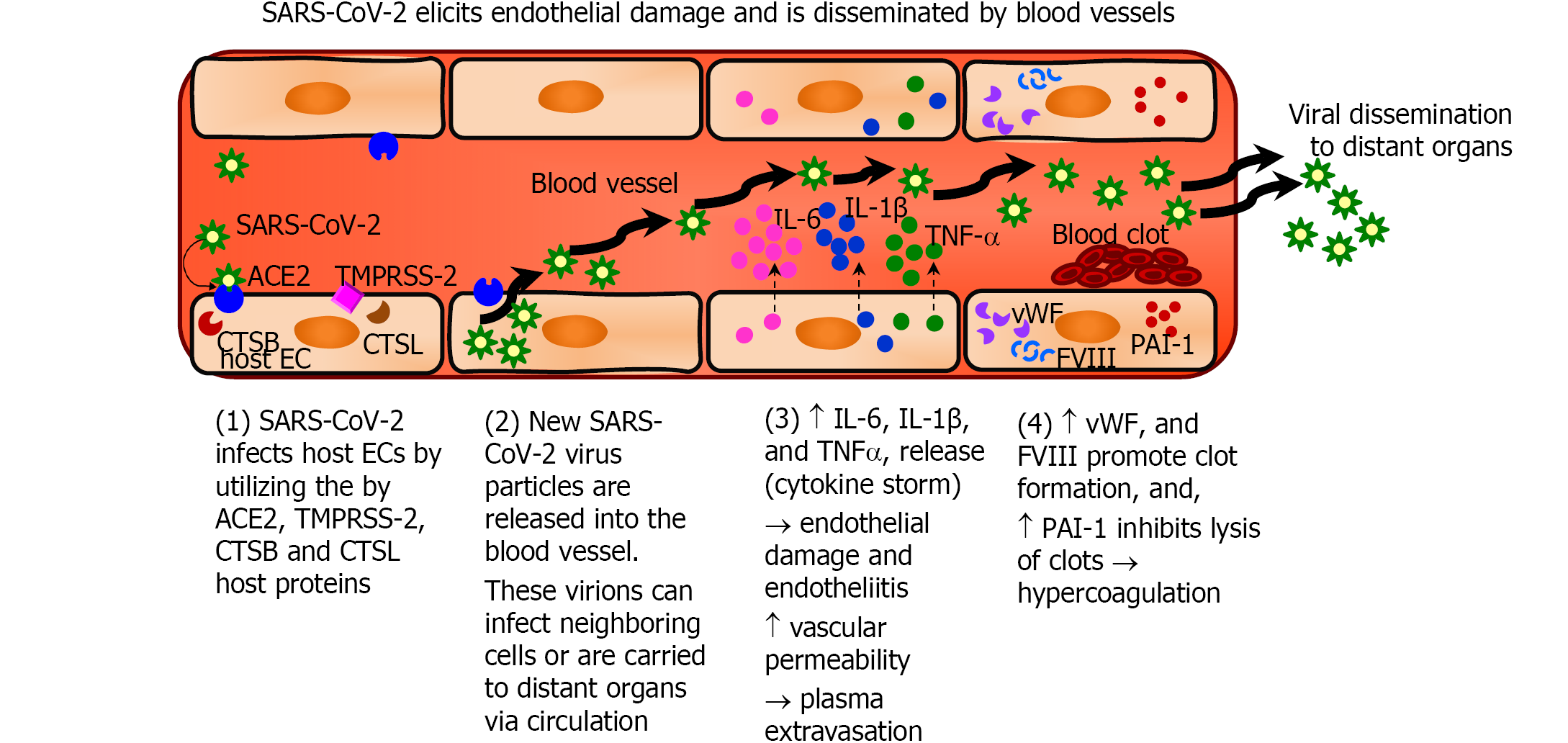
Figure 3 Sequential steps of SARS-CoV-2 infection of endothelial cells and endothelial damage.
SARS-CoV-2 infects endothelial cells (ECs) using the host angiotensin-converting enzyme 2 receptors and cellular proteases (transmembrane serine protease 2, and cathepsin B and L). The virus then replicates within the cells and is released into the blood vessels, which then disseminate the virus to distant organs. Severe COVID-19 results in a cytokine storm wherein there is increased production of pro-inflammatory cytokines such as interleukin-6 (IL-6), IL-1, interleukin-1 β (IL-1 β) and tumor necrosis factor-α (TNF-α), and results in endothelial damage and endotheliitis, and demonstrated increased vascular permeability that cause plasma extravasation. Activated ECs produce increased amounts of vWF and factor VIII, and PAI-1, which induce a pro-coagulant, hypofibrinolytic state. SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; ECs: Endothelial cells; ACE2: Angiotensin-converting enzyme 2; TMPRSS-2: Transmembrane serine protease 2; CTSB: Cathepsin B; CTSL: Cathepsin L; IL: Interleukin; TNF-α: Tumor necrosis factor-α.
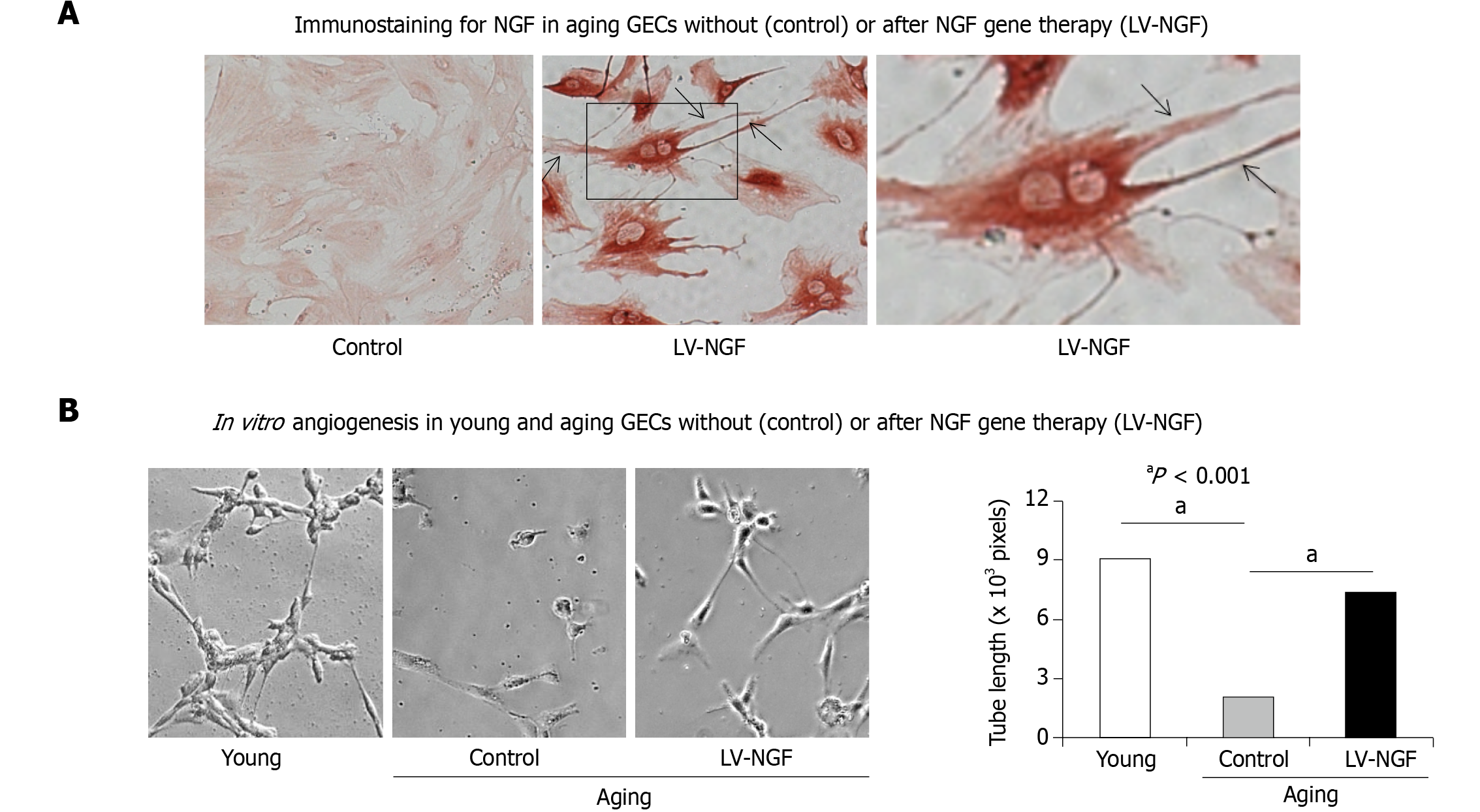
Figure 4 Nerve growth factor gene therapy increases nerve growth factor expression and reverses impaired in vitro angiogenesis in aging gastric endothelial cells.
A: Nerve growth factor (NGF) gene therapy of aging Gastric endothelial cells (GECs) using lentiviral-NGF (LV-NGF) induced NGF expression (brown staining) and extensive, long filopodia (arrows) reflecting a change in these cells to an angiogenic phenotype; aging GECs without gene therapy (negative controls) have minimal NGF expression and lack filopodia; B: NGF gene therapy with LV-NGF resulted in 3.7-fold increased in vitro angiogenesis at 6 h in aging GECs vs negative controls (control). Panels are representative images of capillary-like tube formation. Original magnification: × 200. Data are means ± SD (n = 6). (aP < 0.001). NGF: Nerve growth factor; GEC: Gastric endothelial cells; LV: Lentiviral. Reproduced with permission from reference[20], which is an open-access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
- Citation: Tarnawski AS, Ahluwalia A. Endothelial cells and blood vessels are major targets for COVID-19-induced tissue injury and spreading to various organs. World J Gastroenterol 2022; 28(3): 275-289
- URL: https://www.wjgnet.com/1007-9327/full/v28/i3/275.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i3.275