Copyright
©The Author(s) 2022.
World J Gastroenterol. Jun 21, 2022; 28(23): 2625-2632
Published online Jun 21, 2022. doi: 10.3748/wjg.v28.i23.2625
Published online Jun 21, 2022. doi: 10.3748/wjg.v28.i23.2625
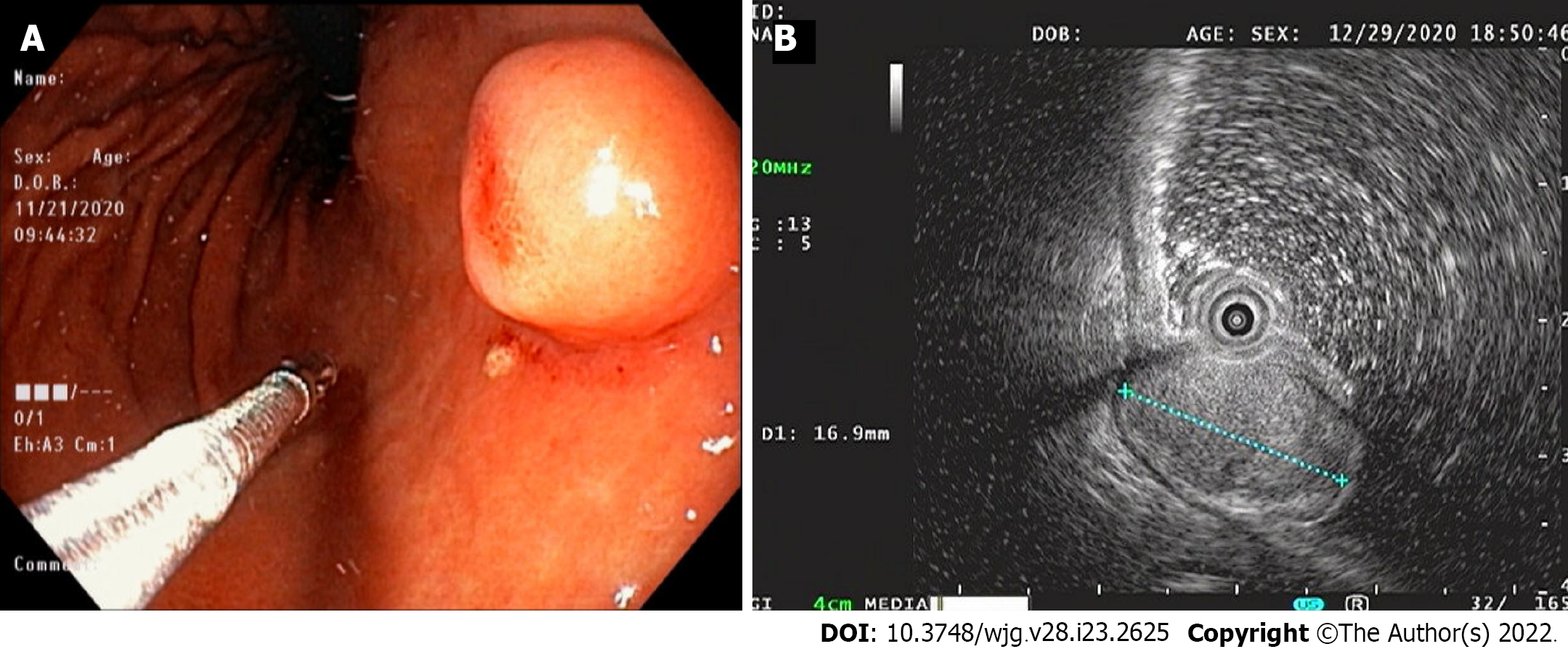
Figure 1 Endoscopy and endoscopic ultrasound images.
A: Endoscopic image showing a 15-mm-sized, submucosal tumor-like, protruding lesion with focal mucosal erythema and depression of overlying mucosa; B: Endoscopic ultrasound image showing a well-circumscribed, slightly heterogeneous, 17 mm × 10 mm sized, isoechoic mass originating from the third sonographic layer.
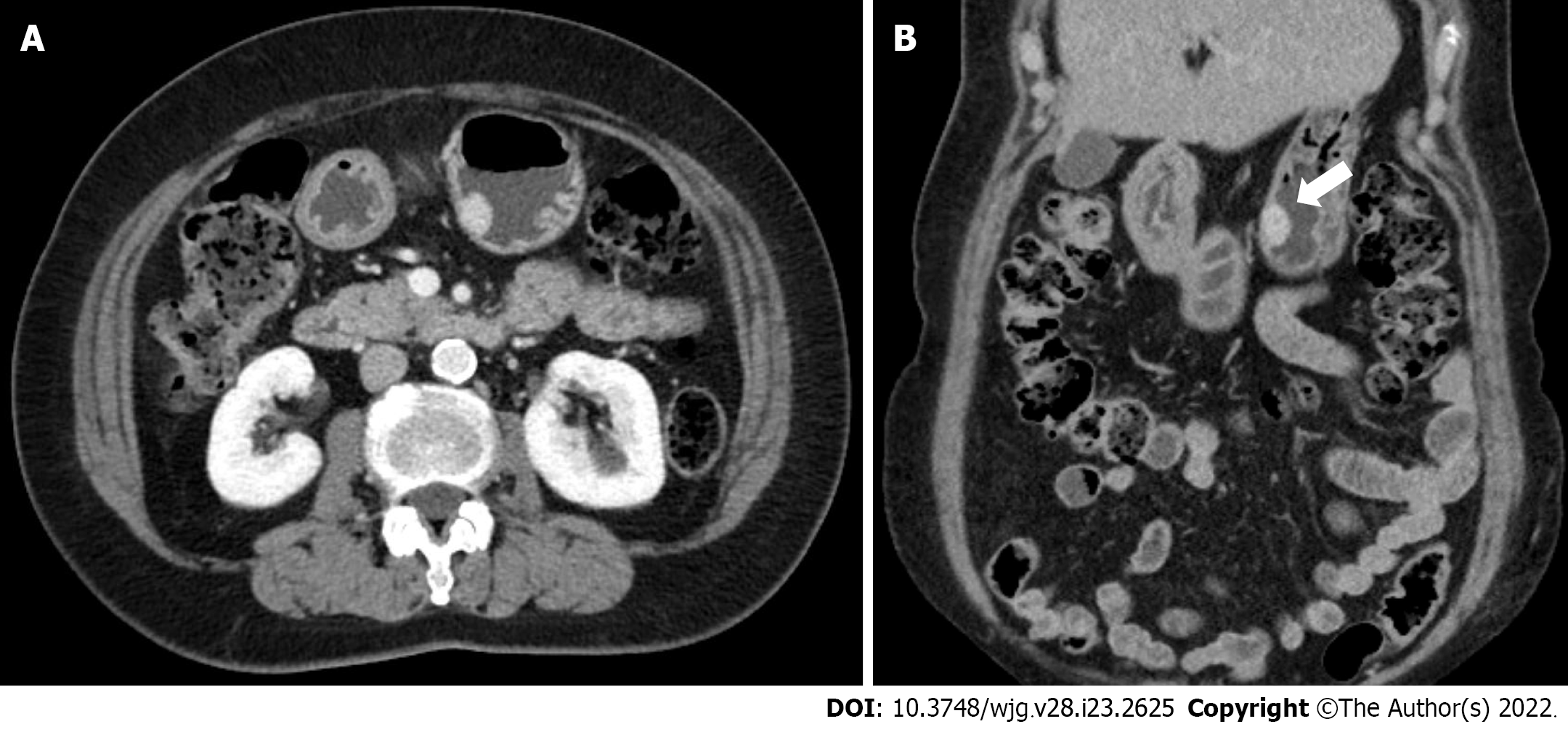
Figure 2 Abdominal computed tomography images.
A and B: Axial and coronal computed tomography images showing a well-enhanced and protruding intraluminal mass in the gastric body.
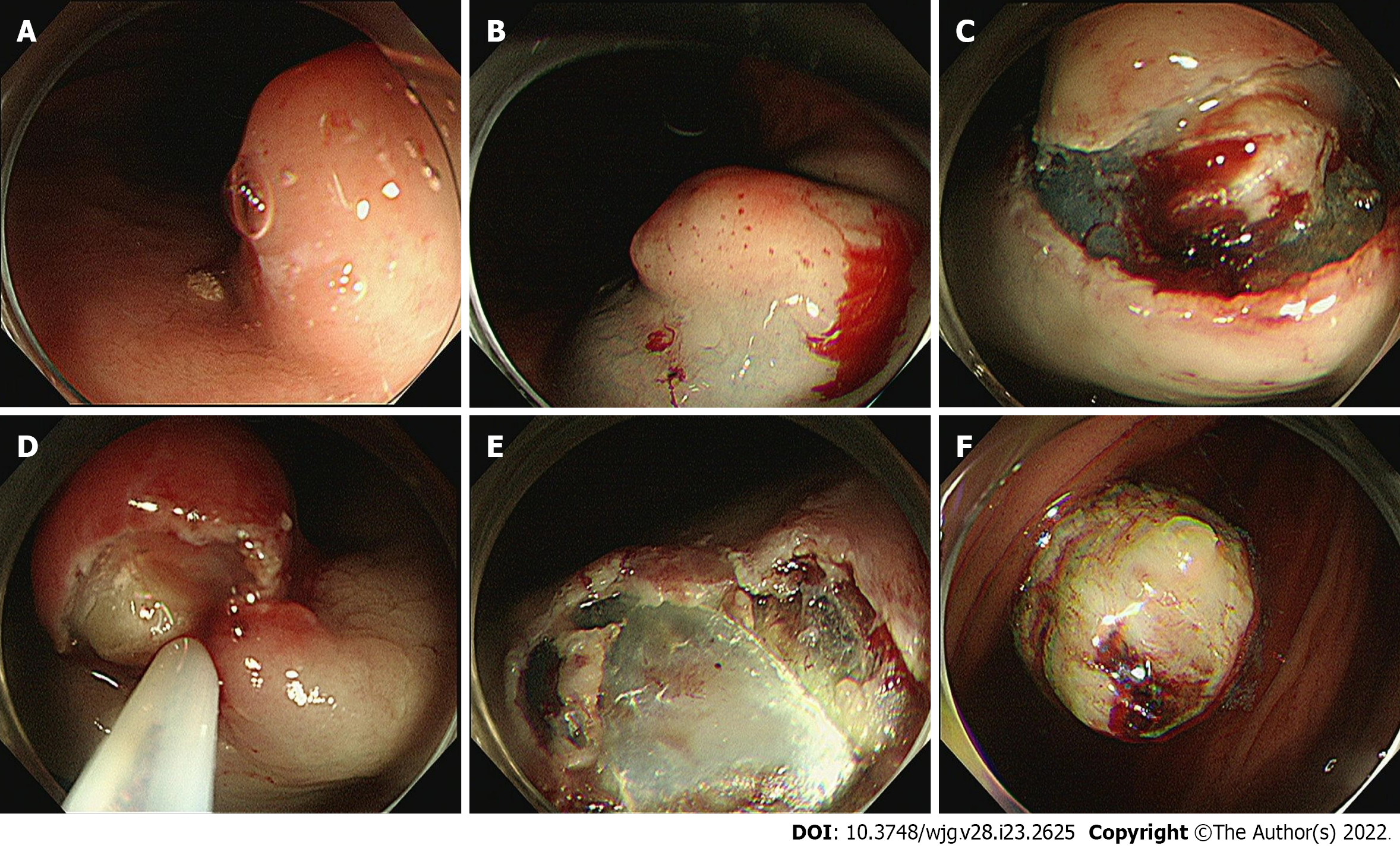
Figure 3 Process of the endoscopic resection.
A: Marking outside the lesion; B: Injection of saline–epinephrine for submucosal lifting; C: Circumferential mucosal incision and partial submucosal dissection; D and E: Resection using a snare; F: Resected tumor.
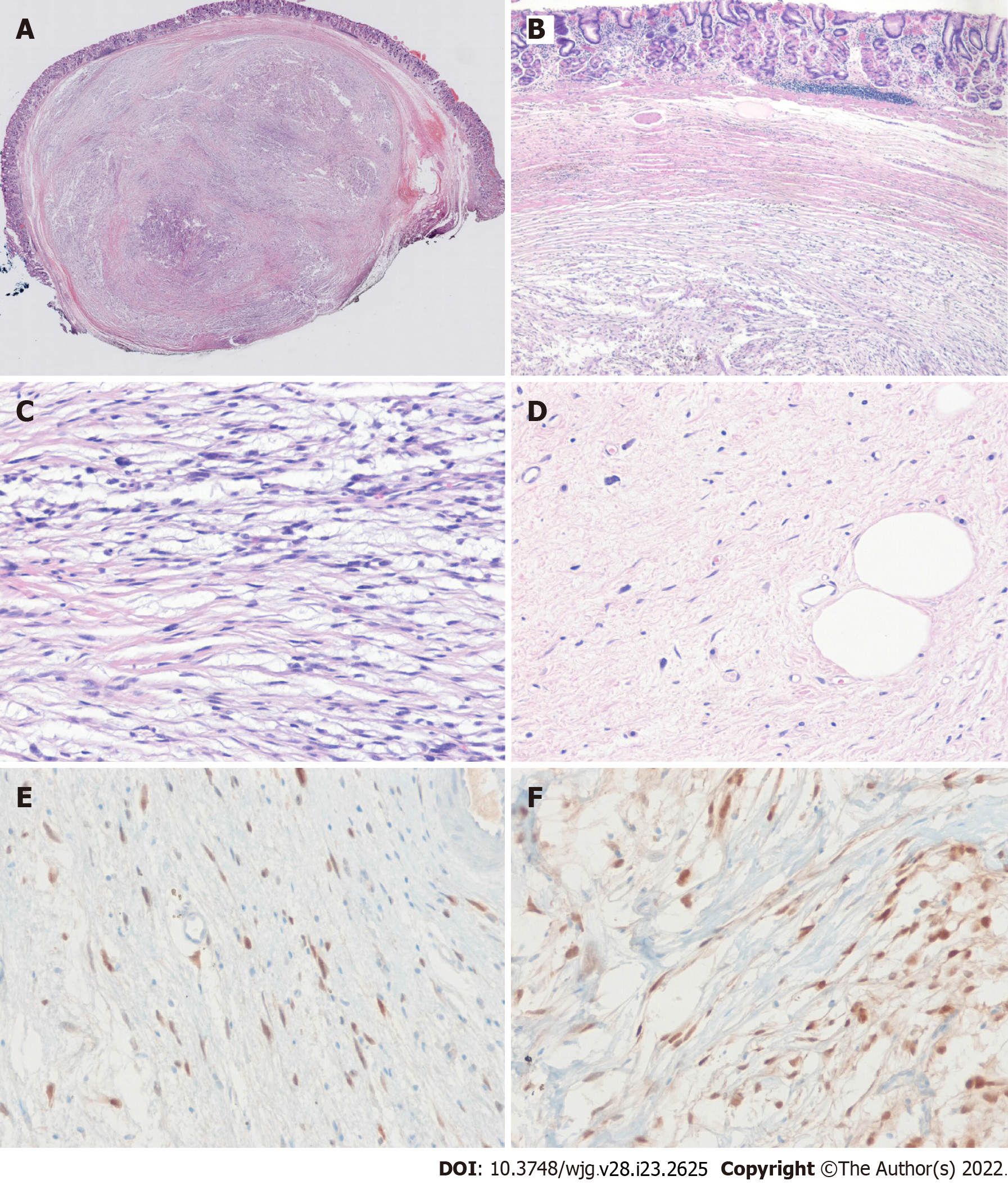
Figure 4 The histopathological diagnosis of the endoscopically resected lesion.
A and B: The tumor had a smooth margin, an internal heterogeneous morphology, and was located in submucosa (H & E, original magnification × 10, × 40); the deep resection margin was positive for tumor; C: The neoplasm consists of infiltrated, atypical spindle-shaped tumor cells with nuclear hyperchromasia (H & E, original magnification × 100); D: Photomicrograph showing highly pleomorphic spindle cells with some rare lipoblasts (H&E, original magnification × 100); E and F: Immunohistochemical staining for tumor cells show diffuse positivity for MDM2 (E) and CDK4 (F).
- Citation: Cho JH, Byeon JH, Lee SH. Primary gastric dedifferentiated liposarcoma resected endoscopically: A case report. World J Gastroenterol 2022; 28(23): 2625-2632
- URL: https://www.wjgnet.com/1007-9327/full/v28/i23/2625.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i23.2625