Copyright
©The Author(s) 2022.
World J Gastroenterol. May 21, 2022; 28(19): 2057-2075
Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2057
Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2057
Figure 1 Classic hepatic arterial anatomy.
A: Digital subtraction angiography showed normal anatomy of the hepatic arteries; B: Axial maximum intensity projection image showed normal anatomy of the hepatic arteries. CHA: Common hepatic artery; GDA: Gastroduodenal artery; LGA: Left gastric artery; LGEA: Left gastroepiploic artery; LHA: Left hepatic artery; PHA: Proper hepatic artery; RHA: Right hepatic artery; SA: Splenic artery.
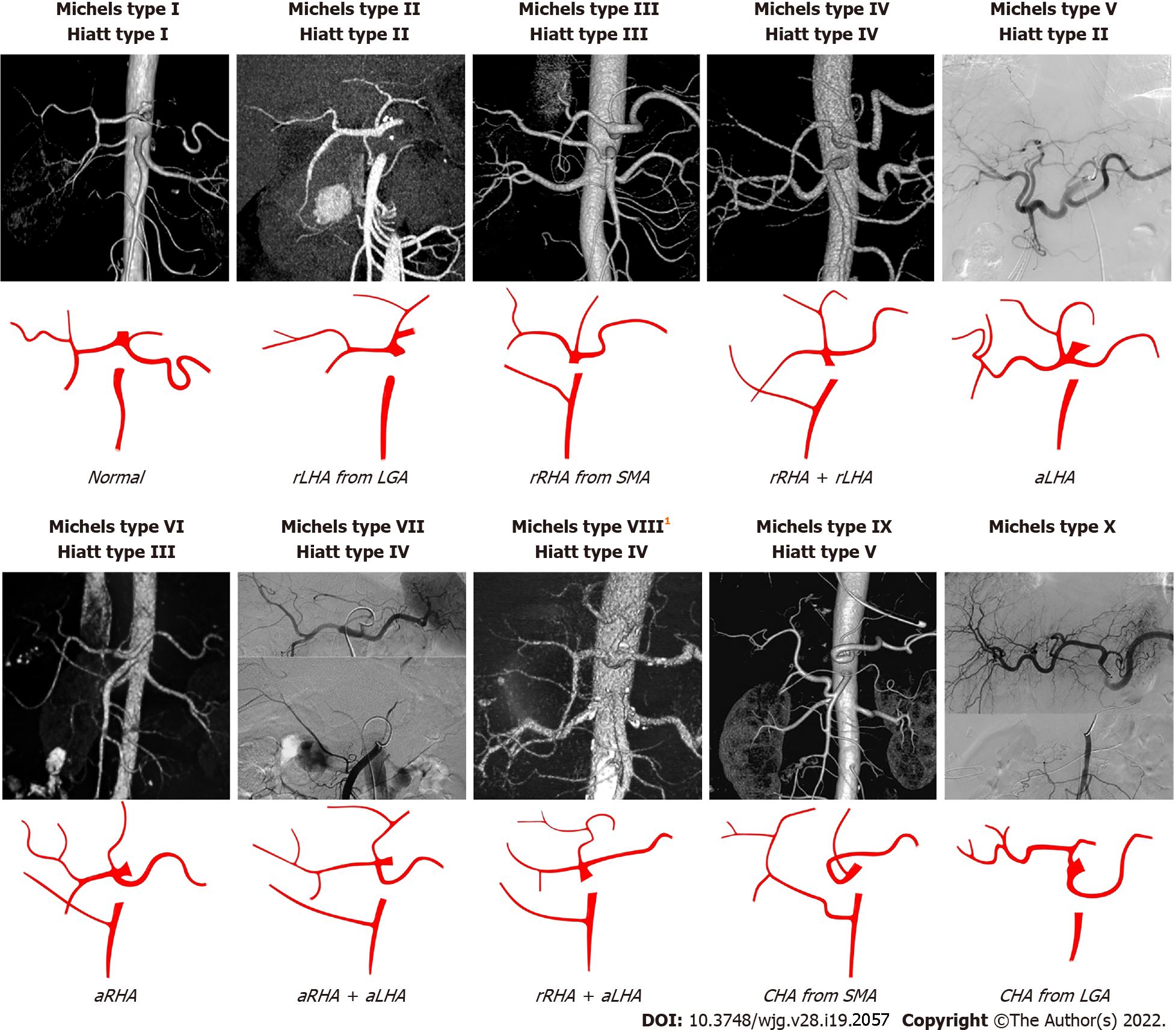
Figure 2 The Michels and Hiatt classifications of hepatic artery.
1Michels type VIII includes replaced right hepatic artery (rRHA) + accessory left hepatic artery (aLHA) or replaced left hepatic artery (rLHA) + accessory right hepatic artery (aRHA). The common hepatic artery (CHA) from aorta is classified as Hiatt type VI. LGA: Left gastric artery; SMA: Superior mesenteric artery; rRHA: Replaced right hepatic artery; aLHA: Accessory left hepatic artery; rLHA: Replaced left hepatic artery; CHA: Common hepatic artery; aRHA: Accessory right hepatic artery.
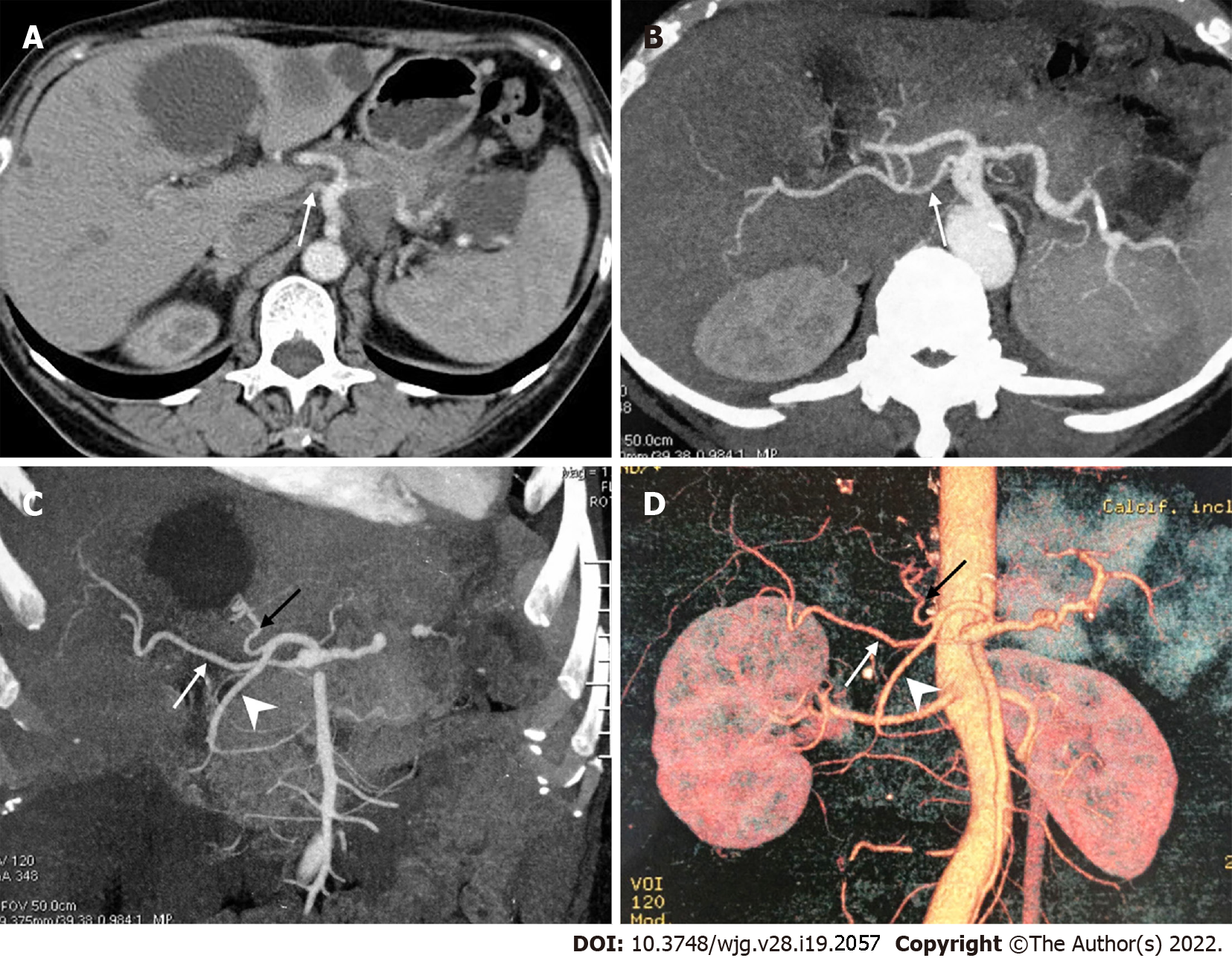
Figure 3 A peculiar replaced right hepatic artery arising directly from the celiac artery.
A: Axial contrast enhanced computed tomography scan; B-D: Axial maximum intensity projection (MIP, B), coronal MIP (C) and 3D-volume rendering (D) images showed that the replaced right hepatic artery (white arrow) originated directly from the celiac artery, and the common hepatic artery divided into the left hepatic artery (black arrow) and gastroduodenal artery (arrowhead).
Figure 4 The hepato-spleno-mesenteric trunk.
3D-volume rendering computed tomography images showed that the hepato-spleno-mesenteric trunk was formed by the common hepatic artery, splenic artery and superior mesenteric artery, and the left gastric artery (LGA) originated from the aorta. A: Coronal view; B: Sagittal view. HSMT: Hepato-spleno-mesenteric trunk; CHA: Common hepatic artery; SA: Splenic artery; SMA: Superior mesenteric artery; LGA: Left gastric artery.
Figure 5 Retrograde flow from the superior mesenteric artery due to tumor involvement of the hepatic artery.
A: Computed tomography scan showed a low-density mass in the pancreatic head with common hepatic artery involvement (arrow); B: Selective celiacography showed involvement of the hepatic artery from the origin of the celiac artery to the bifurcation of the left and right hepatic arteries, as well as involvement of the gastroduodenal artery. Additionally, an accessory right hepatic artery was seen originating from the gastroduodenal artery; C: Superior mesenteric angiography showed retrograde flow to the liver from the superior mesenteric artery via the pancreaticoduodenal arcade.
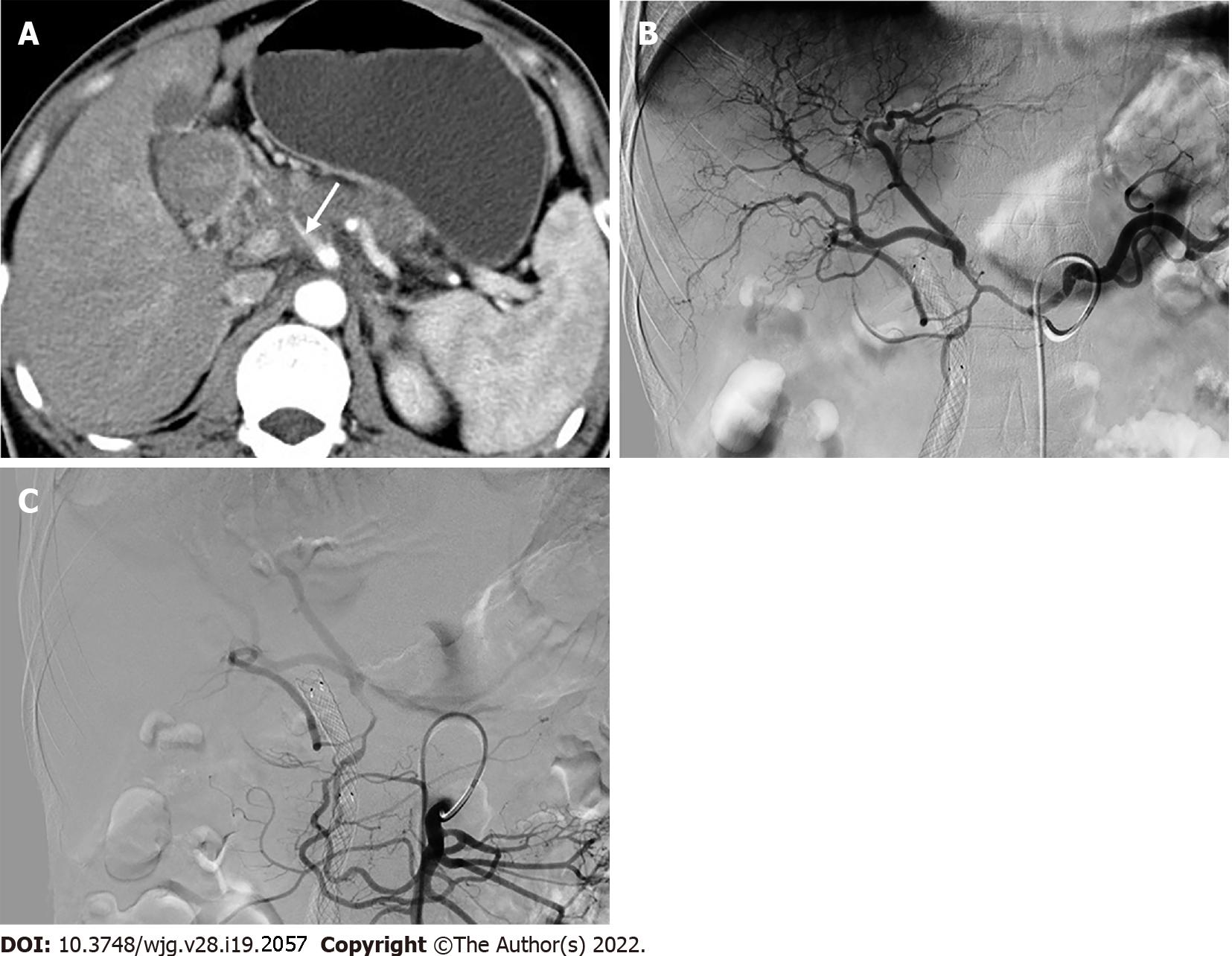
Figure 6 Collateral pathways due to celiac axis stenosis.
A: Computed tomography scan showed a mass in the pancreatic head with dilated biliary-pancreatic duct, and celiac axis stenosis (CAS, arrow); B: Sagittal maximum intensity projection image demonstrated CAS (arrow); C: Selective celiac angiographic examination revealed the left gastric artery and splenic artery, with no hepatic arteries depicted, which is compatible with occlusion of the common hepatic artery; D: Superior mesenteric arteriogram demonstrated retrograde filling of the celiac branches via the pancreaticoduodenal arcades (arrow) by way of the gastroduodenal artery and anomalous blood vessels traversing the pancreas (arrowhead).
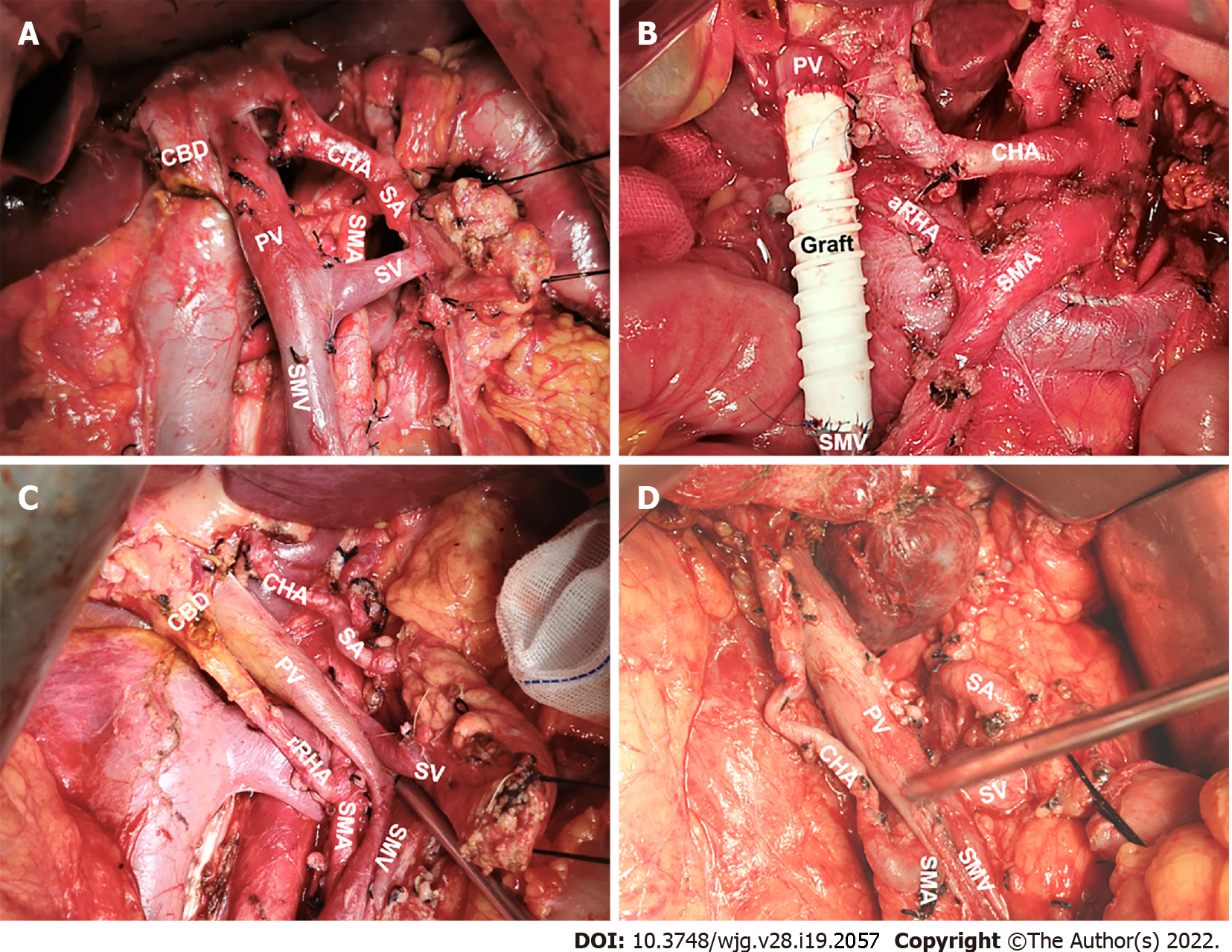
Figure 7 Significant hepatic artery variants during open pancreaticoduodenectomy.
A: Normal anatomy of hepatic artery; B: Accessory right hepatic artery from the superior mesenteric artery (SMA); C: Replaced right hepatic artery from the SMA; D: Common hepatic artery from the SMA. CBD: Common bile duct; PV: Portal vein; SA: Splenic artery; SV: Splenic vein; SMV: Superior mesenteric vein.
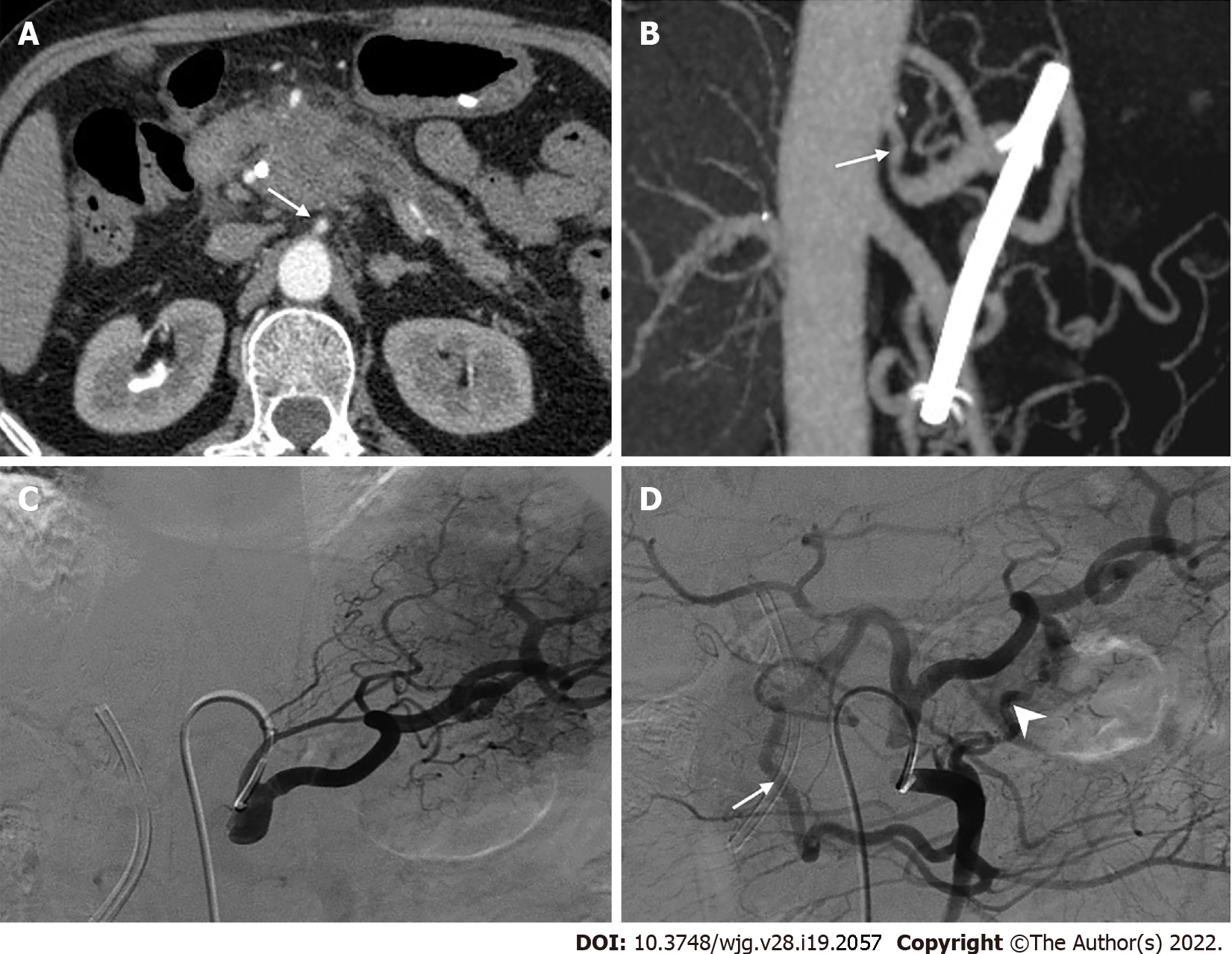
Figure 8 A rare replaced right hepatic artery from the superior mesenteric artery susceptible to injury during pancreaticoduodenectomy.
A: Coronal maximum intensity projection image showed Michels type IV hepatic artery variant; B. Intraoperative image showed that replaced right hepatic artery (rRHA) originated from the superior mesenteric artery and traveled to the right behind the inferior margin of the pancreatic neck via the superior mesenteric vein anteriorly and gave rise to the gastroduodenal artery and proper hepatic artery. LGA: Left gastric artery; rLHA: Replaced left hepatic artery; SMA: Superior mesenteric artery; GDA: Gastroduodenal artery; SMV: Superior mesenteric vein; PHA: Proper hepatic artery; rRHA: Replaced right hepatic artery.
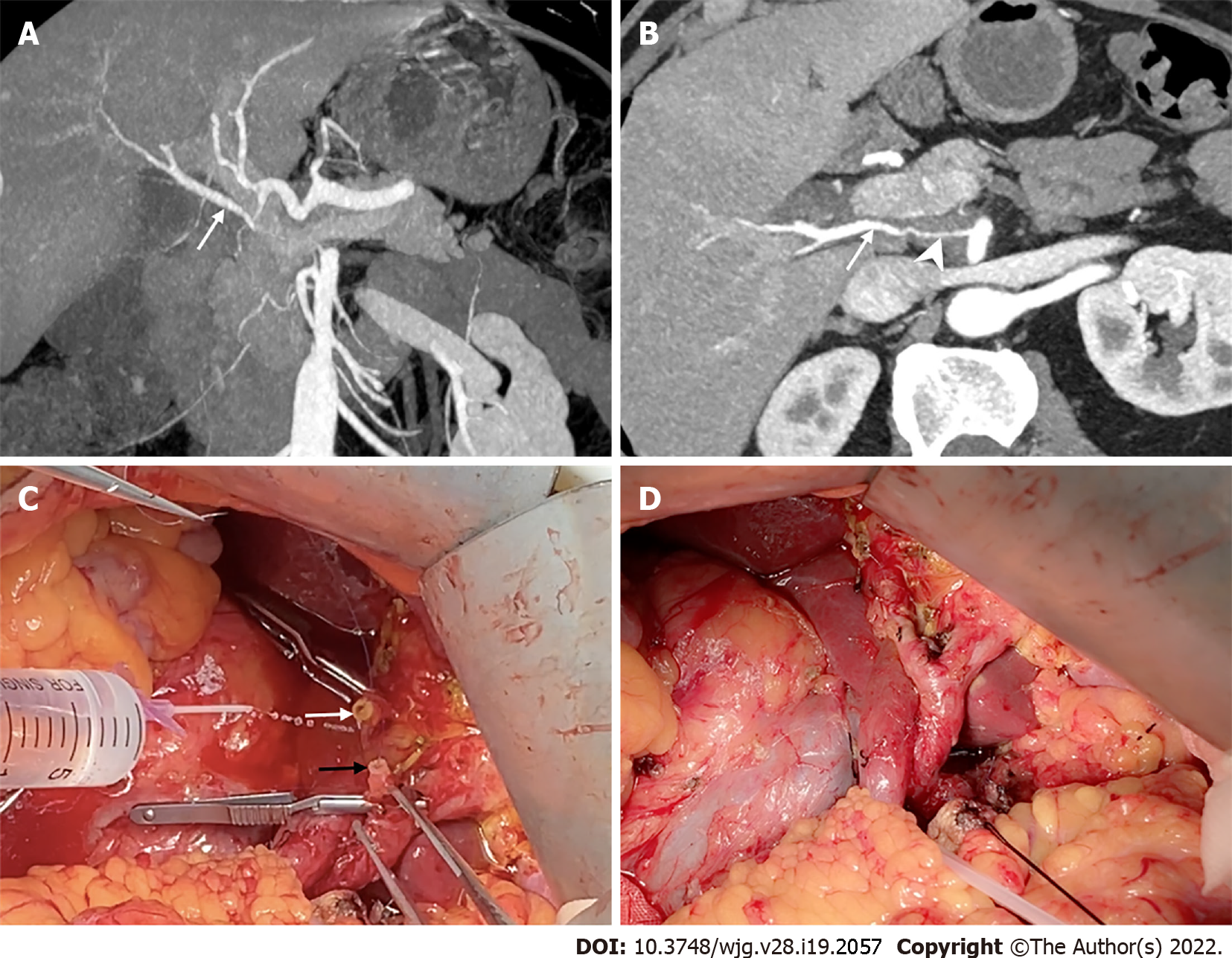
Figure 9 The replaced right hepatic artery reconstruction with gastroduodenal artery remnant during pancreaticoduodenectomy.
A and B: Coronal and axial maximum intensity projection images showed the replaced right hepatic artery (rRHA, arrow) originated from the superior mesenteric artery and penetrated through the pancreatic head with tumor invasion resulting in significant stenosis (arrowhead); C: Intraoperative image showed a long length of the gastroduodenal artery (GDA) remnant (black arrow) was available for direct end-to-end anastomosis with the rRHA (white arrow); D: The rRHA-GDA anastomosis is complete.
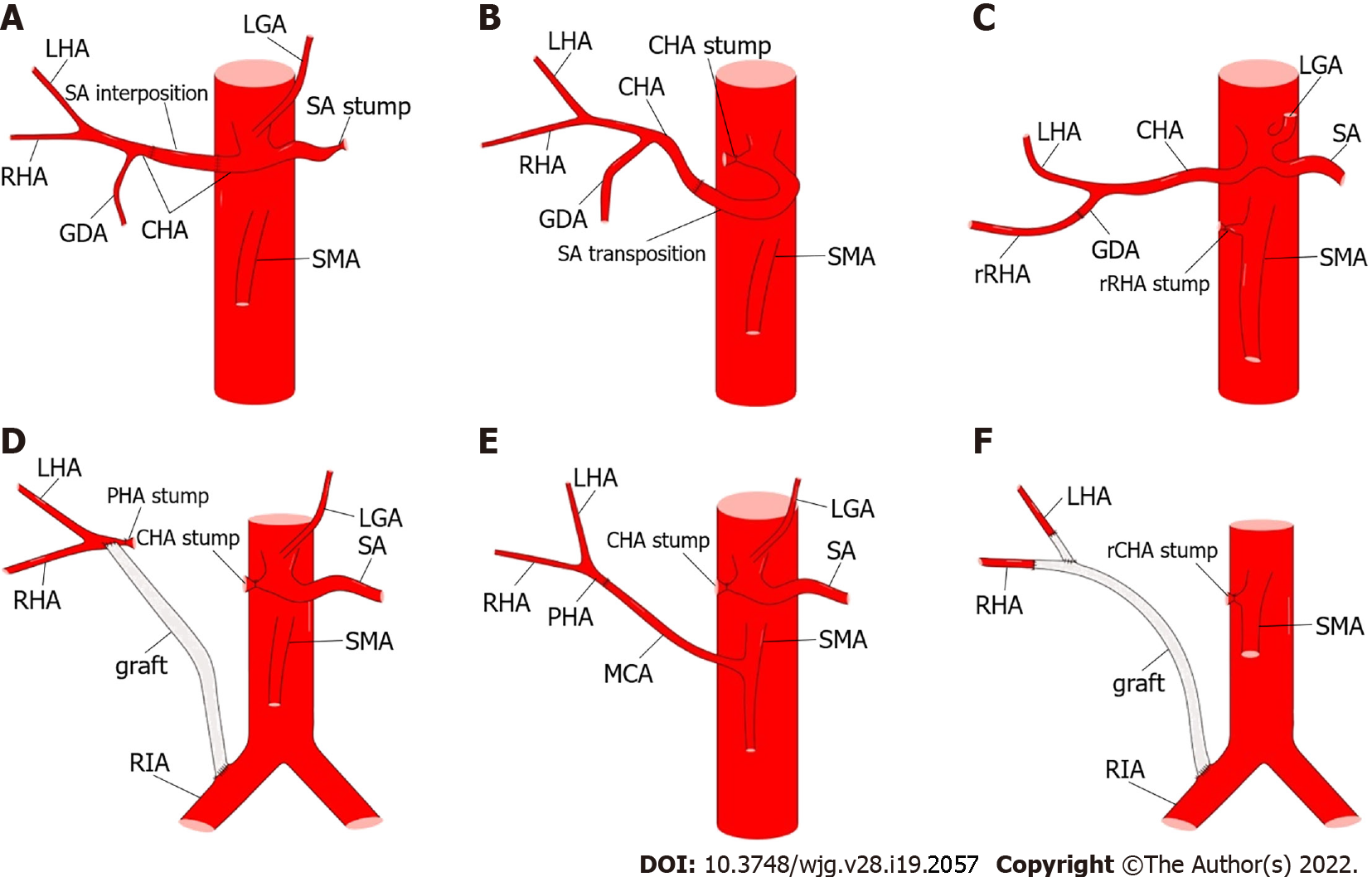
Figure 10 Methods of hepatic artery reconstruction during pancreaticoduodenectomy.
A: Splenic artery (SA) interposition between two ends of the common hepatic artery (CHA); B: SA transposition to be anastomosed with the CHA; C: Direct end-to-end anastomosis between replaced right hepatic artery (rRHA) and gastroduodenal artery (GDA); D: Graft interposition between proper hepatic artery (PHA) and right iliac artery (RIA); E: Direct end-to-end anastomosis between PHA and middle colic artery; F: Graft interposition between RHA and RIA, and end-to-side anastomosis between left hepatic artery and graft. CA: Celiac artery; LGA: Left gastric artery; rCHA: Replaced common hepatic artery; SMA: Superior mesenteric artery; rRHA: Replaced right hepatic artery; CHA: Common hepatic artery; GDA: Gastroduodenal artery; LHA: Left hepatic artery; MCA: Middle colic artery; SA: Splenic artery.
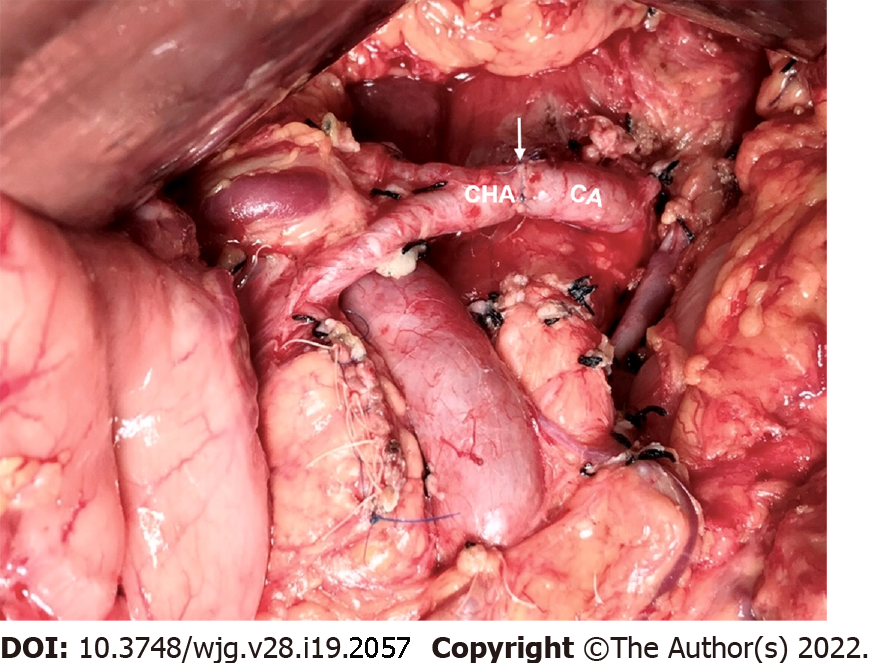
Figure 11 The common hepatic artery-celiac artery anastomosis during the modified Appleby procedure.
Intraoperative image showed direct end-to-end anastomosis between common hepatic artery and celiac artery following distal pancreatectomy with celiac axis resection. The white arrow marks the anastomosis. CHA: Common hepatic artery; CA: Celiac artery.
Figure 12 Methods of hepatic artery reconstruction during pancreatectomy with en bloc celiac axis resection.
A: Direct end-to-end anastomosis between common hepatic artery (CHA) and celiac artery (CA); B: Graft interposition between CHA and CA; C: Direct end-to-end anastomosis between CHA and abdominal aorta (AA); D: Graft interposition between CHA and AA; E: Graft interposition between proper hepatic artery (PHA) and CA; F: Direct end-to-end anastomosis between CHA and left gastric artery [LGA, with replaced left hepatic artery (rLHA) from it]; G: Graft interposition between PHA and AA; H: Graft interposition between CHA and left iliac artery; I: Direct end-to-end anastomosis between PHA and middle colic artery. GDA: Gastroduodenal artery; LHA: Left hepatic artery; RHA: Right hepatic artery; SMA: Superior mesenteric artery.
- Citation: Xu YC, Yang F, Fu DL. Clinical significance of variant hepatic artery in pancreatic resection: A comprehensive review. World J Gastroenterol 2022; 28(19): 2057-2075
- URL: https://www.wjgnet.com/1007-9327/full/v28/i19/2057.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i19.2057