Copyright
©The Author(s) 2022.
World J Gastroenterol. May 21, 2022; 28(19): 2034-2056
Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2034
Published online May 21, 2022. doi: 10.3748/wjg.v28.i19.2034
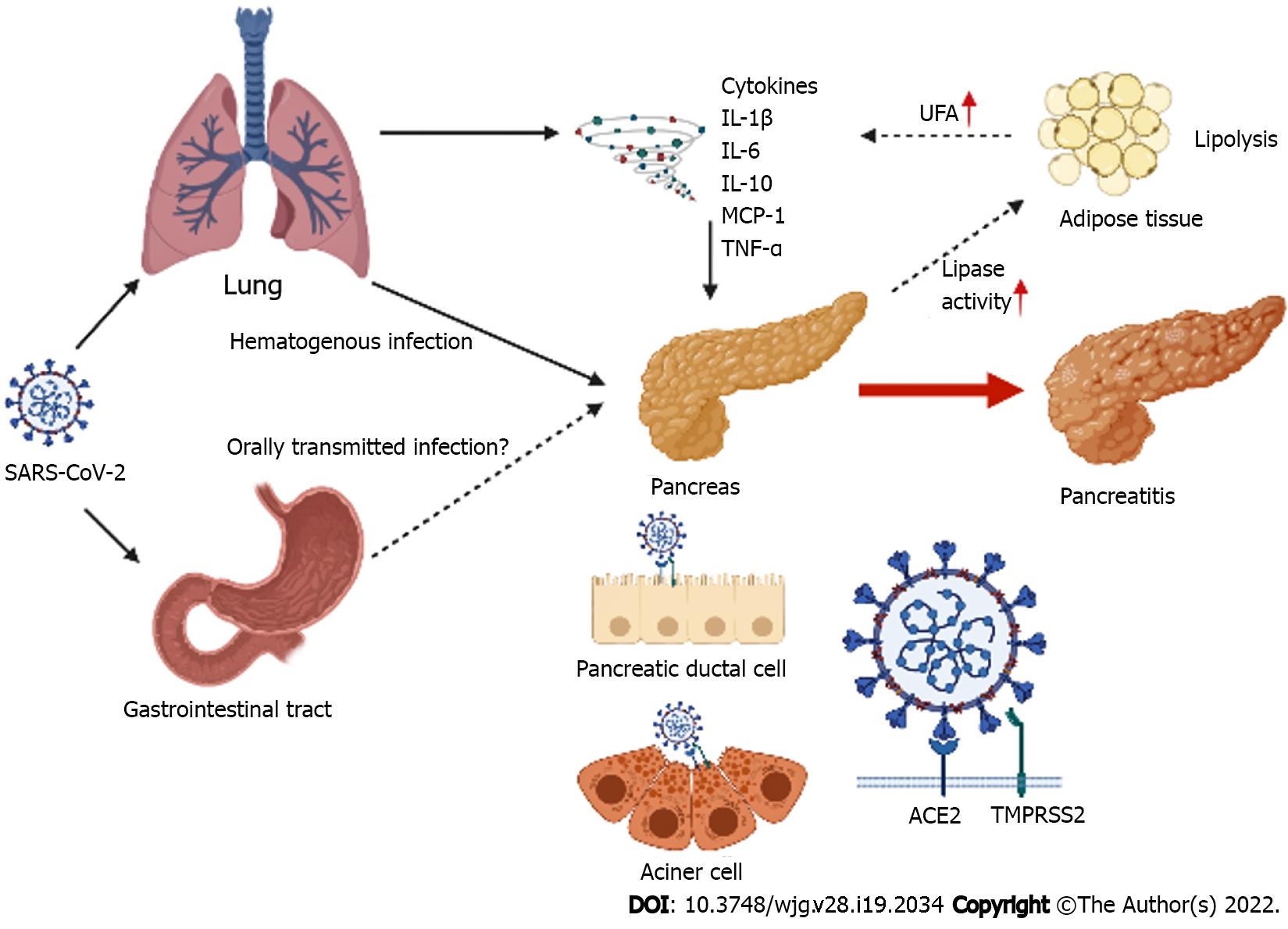
Figure 1 Direct and indirect pathways of pancreatic injury caused by severe acute respiratory syndrome coronavirus-2.
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) disseminates through the bloodstream mainly to the pancreas. SARS-CoV-2 may be transported to the pancreas via the gastrointestinal tract. The pancreas expresses angiotensin converting enzyme-2 (ACE2) and the transmembrane protease serine 2 (TMPRSS2). SARS-CoV-2 binds to ACE2 after the viral spike (S) protein is primed by TMPRSS2 for cell entry. Therefore, SARS-CoV-2 may potentially cause direct pancreatic injury, including acute pancreatitis. However, indirect pancreatic injury may also be caused by systemic inflammatory responses from respiratory failure induced by SARS-CoV-2 infection. Levels of proinflammatory immune mediators associated with pancreatitis, including interleukin (IL)-1β, IL-6, IL-10, interferon-γ, monocyte chemotactic protein-1, and tumor necrosis factor-α are higher in the plasma of patients with coronavirus disease 2019. These mediators may indirectly cause pancreatic injury. An increase in lipase activity triggers lipolysis in the adipose tissues, and enhances levels of serum unsaturated fatty acids (UFA). UFA may cause an increase in levels of proinflammatory immune mediators that lead to systemic inflammation. SARS-CoV-2: Severe acute respiratory syndrome coronavirus-2; ACE2: Angiotensin converting enzyme-2; TMPRSS2: Transmembrane protease serine 2; IL: Interleukin, IFN-γ: Interferon-γ; MCP-1: Monocyte chemotactic protein-1; TNF-α: Tumor necrosis factor-α; UFA: Unsaturated fatty acids.
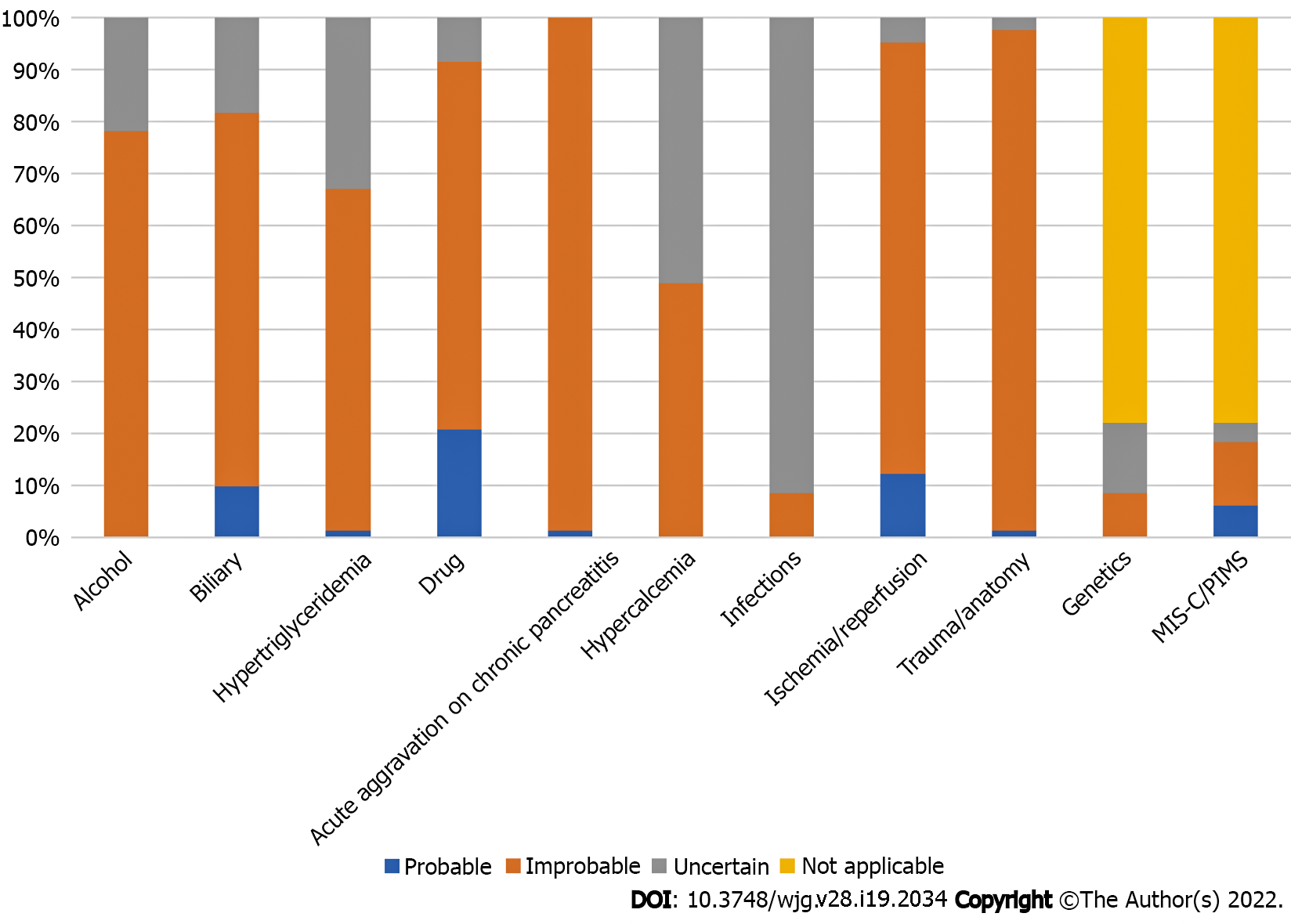
Figure 2 The probability of other etiologies of acute pancreatitis in cases with concurrent coronavirus disease 2019 and acute pancreatitis.
The potential of other etiologies, including alcoholism, biliary, hypertriglyceridemia, hypercalcemia, drug-induced, acute aggravation on chronic pancreatitis, ischemia/reperfusion, and trauma/anatomy. In children, the potential of genetic and multisystemic inflammatory syndrome in children/pediatric inflammatory multisystem syndrome-induced acute pancreatitis (AP) are also evaluated. Moreover, these causes are regarded as inapplicable etiologies of AP in adults. The probability of AP is disregarded in cases with insufficient information on the etiologies of AP. Some etiologies of AP, such as alcohol, acute aggravation on chronic pancreatitis, and trauma/anatomy are well verified. Furthermore, the etiological workup for infections and hypercalcemia is insufficient. Moreover, some cases of AP may have been caused by drug and biliary disease as it may be difficult to exclude them from the etiology of AP. MIS-C: Multisystemic inflammatory syndrome in children; PIMS: Pediatrics inflammatory multisystem syndrome; AP: Acute pancreatitis.
- Citation: Onoyama T, Koda H, Hamamoto W, Kawahara S, Sakamoto Y, Yamashita T, Kurumi H, Kawata S, Takeda Y, Matsumoto K, Isomoto H. Review on acute pancreatitis attributed to COVID-19 infection. World J Gastroenterol 2022; 28(19): 2034-2056
- URL: https://www.wjgnet.com/1007-9327/full/v28/i19/2034.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i19.2034