Copyright
©The Author(s) 2022.
World J Gastroenterol. May 7, 2022; 28(17): 1845-1859
Published online May 7, 2022. doi: 10.3748/wjg.v28.i17.1845
Published online May 7, 2022. doi: 10.3748/wjg.v28.i17.1845
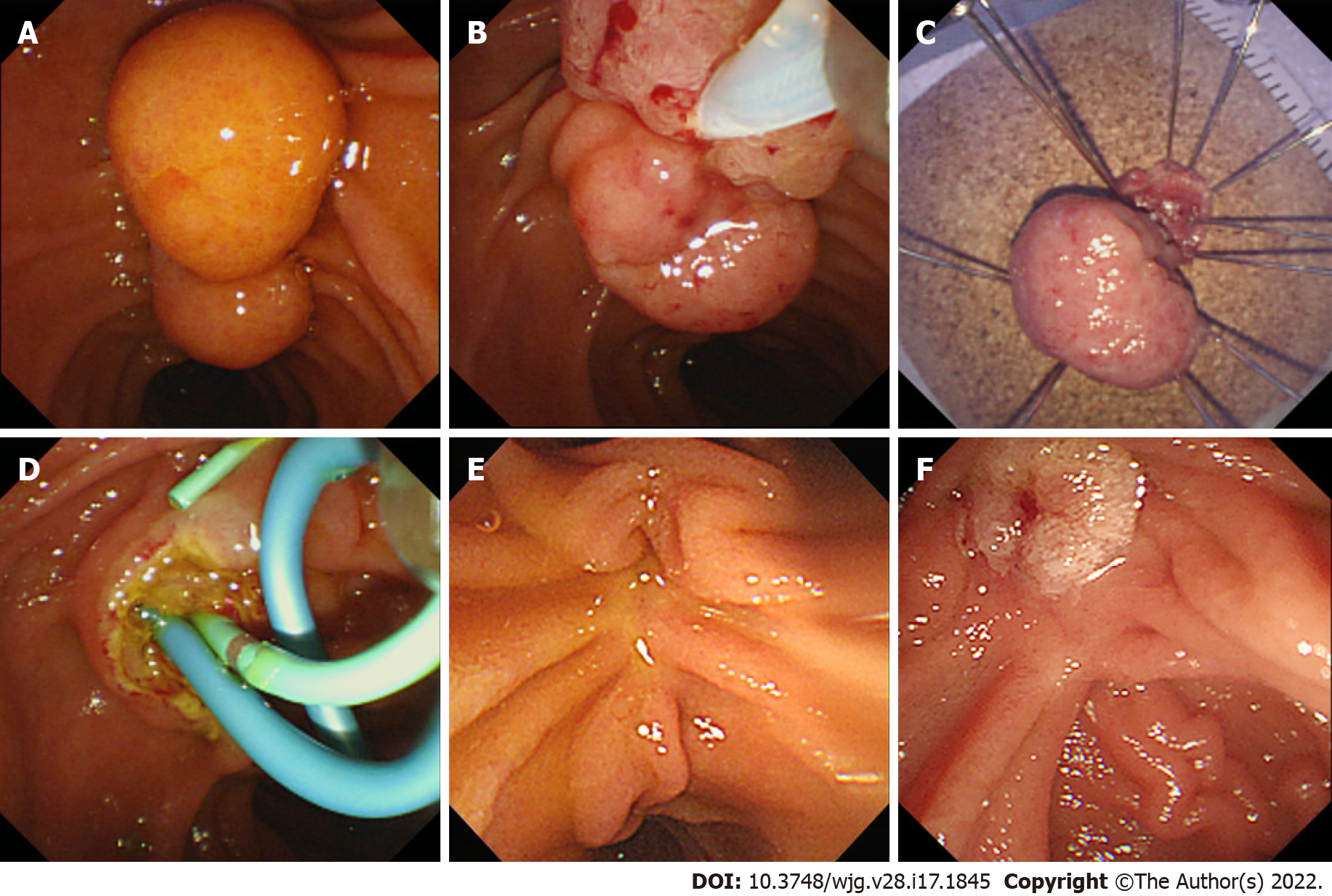
Figure 1 Endoscopic papillectomy of ampullary adenoma.
A: Careful inspection of the ampulla was required before the procedure; B: Endoscopic papillectomy was performed using a conventional polypectomy snare; C: The resected specimen was retrieved and pinned on a cork with nails for pathological evaluation; D: The resected area was carefully inspected, and an additional procedure including common bile duct stenting (blue stent) or pancreatic duct stenting (green stent) was performed; E: Endoscopic surveillance was mandatory; F: If recurrence was suspected, additional treatment was considered.
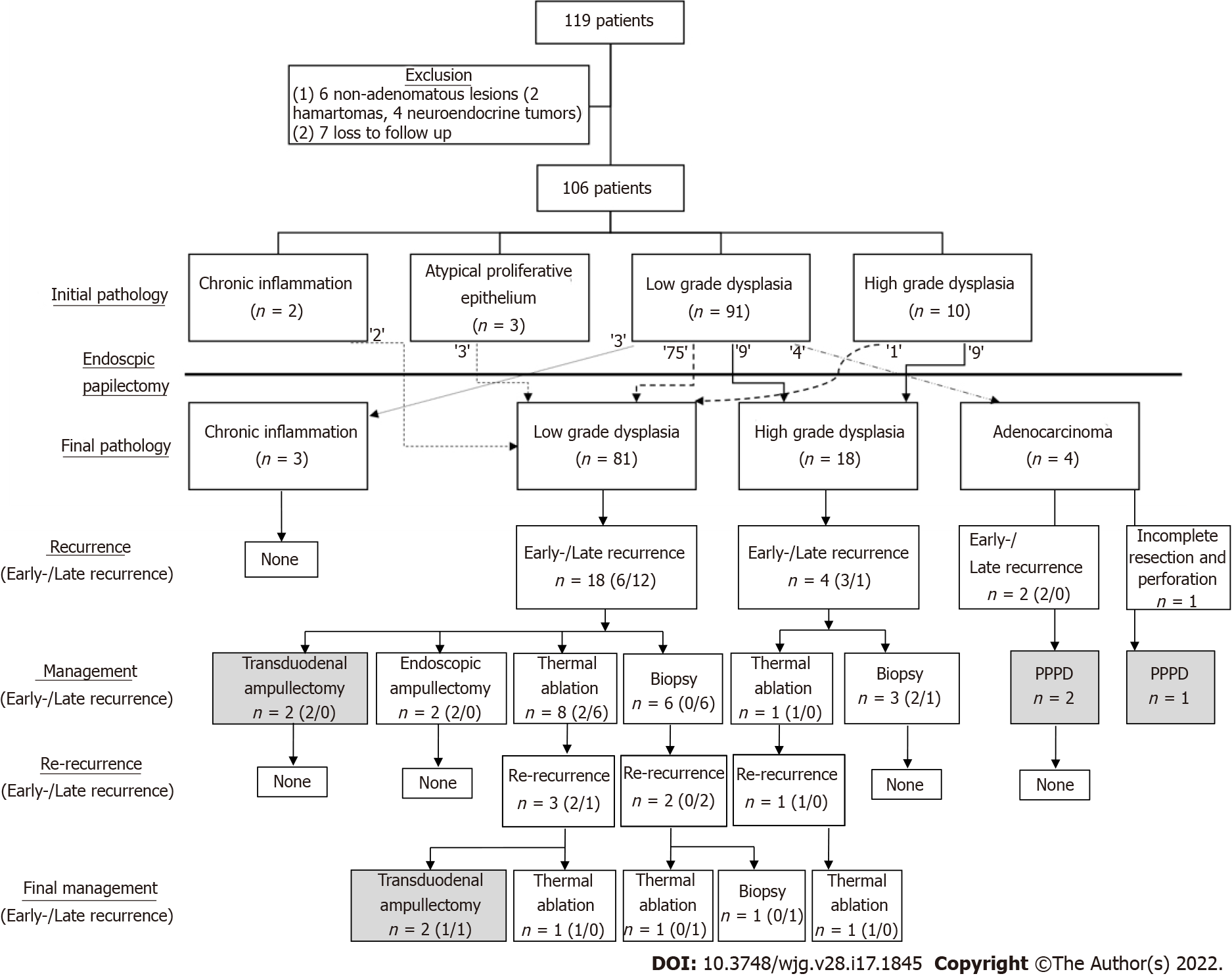
Figure 2 Flowchart of the study.
After applying the exclusion criteria, 106 patients were enrolled, showing the correlation between the initial and final pathology. After the procedure, remnant and recurrent lesions were identified in follow-up surveillances. Most of these lesions were successfully managed with endoscopy. The gray-colored box indicates surgical management.
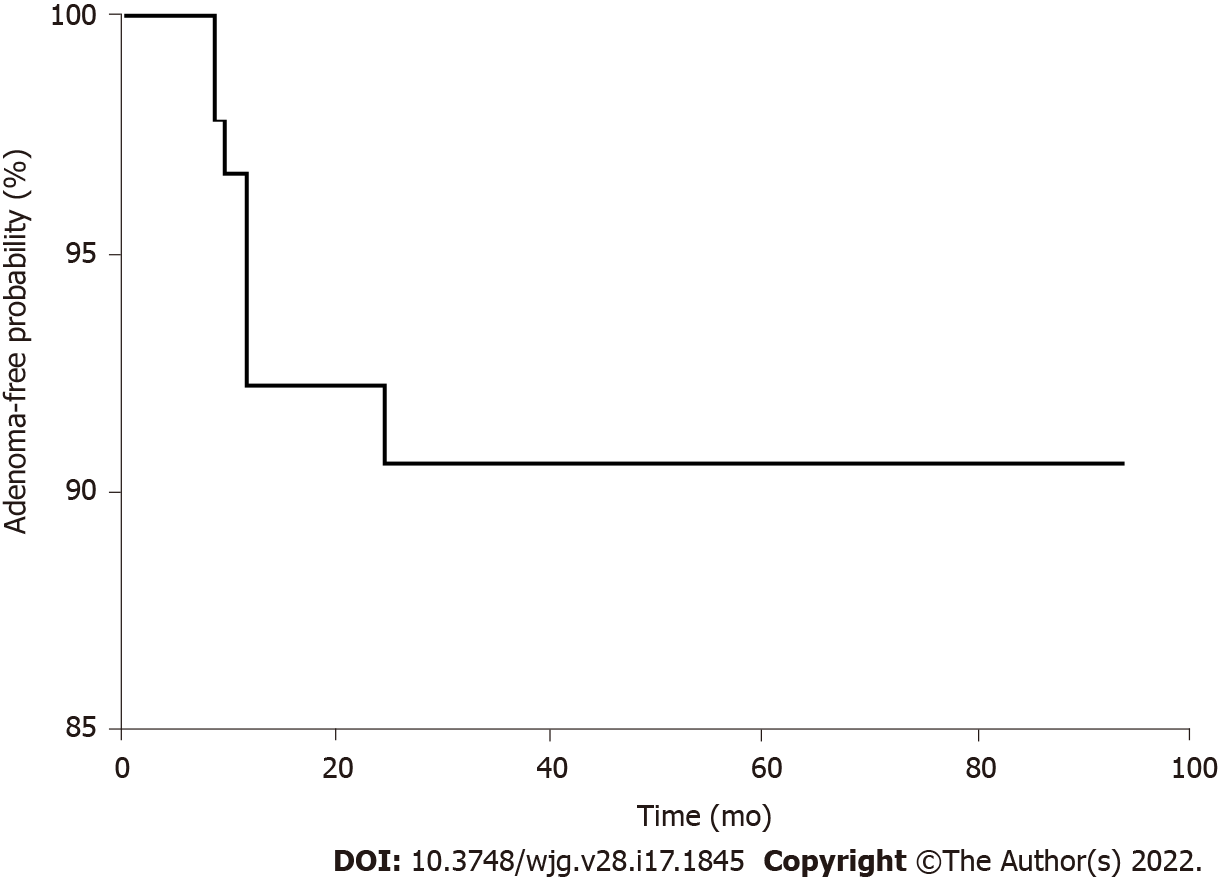
Figure 3 Adenoma-free survival after endoscopic papillectomy.
The vertical axis of the graph indicates the adenoma-free probability, and the horizontal axis shows time to remnant or recurrence after endoscopic papillectomy. The longest adenoma-free period before recurrence was 27 mo, and the longest adenoma-free period without recurrence was 94 mo.
- Citation: Choi SJ, Lee HS, Kim J, Choe JW, Lee JM, Hyun JJ, Yoon JH, Kim HJ, Kim JS, Choi HS. Clinical outcomes of endoscopic papillectomy of ampullary adenoma: A multi-center study. World J Gastroenterol 2022; 28(17): 1845-1859
- URL: https://www.wjgnet.com/1007-9327/full/v28/i17/1845.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i17.1845