Copyright
©The Author(s) 2021.
World J Gastroenterol. Sep 7, 2021; 27(33): 5460-5473
Published online Sep 7, 2021. doi: 10.3748/wjg.v27.i33.5460
Published online Sep 7, 2021. doi: 10.3748/wjg.v27.i33.5460
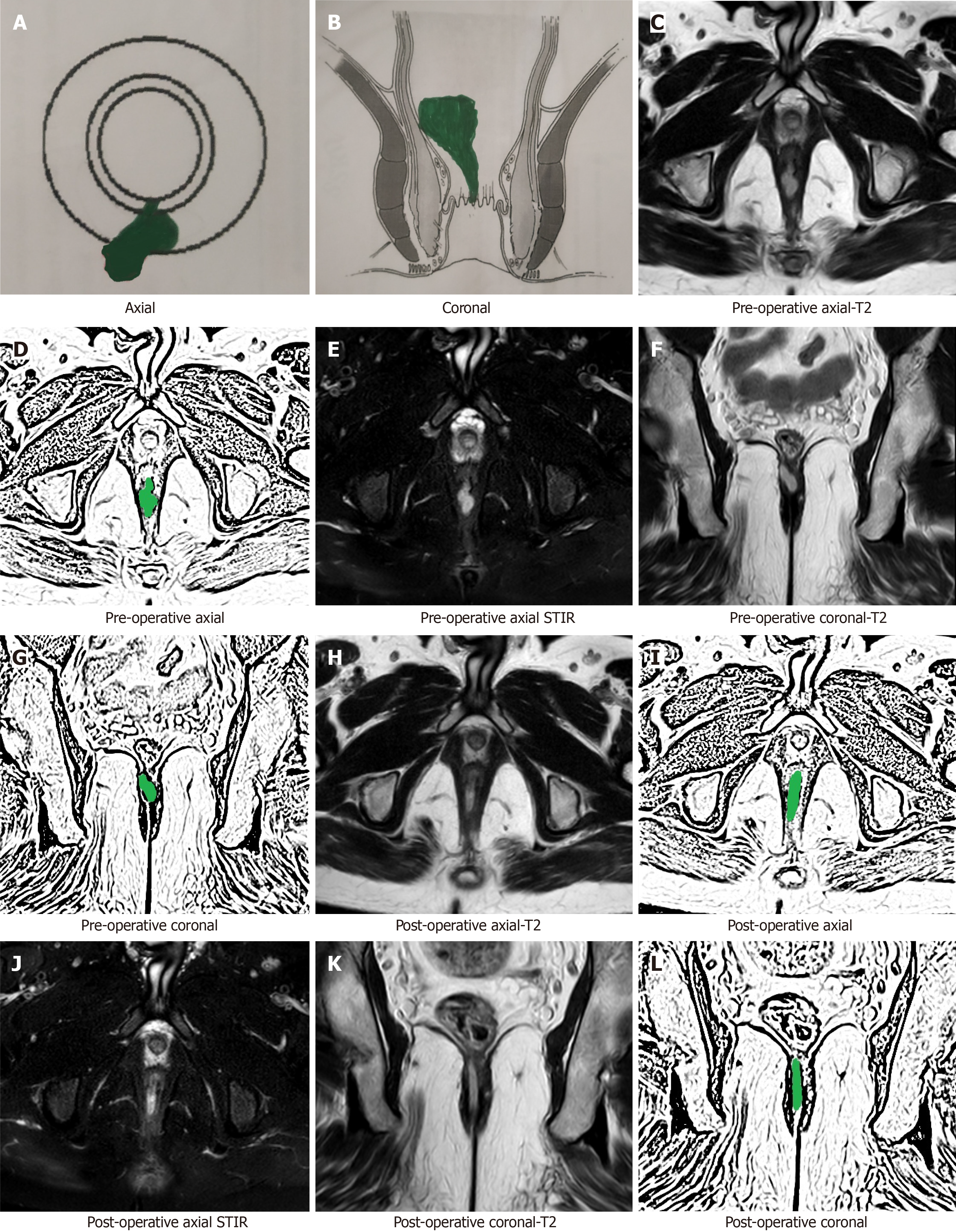
Figure 1 A 37-year-old male patient with a high posterior intersphincteric abscess was drained by transanal opening of the inter
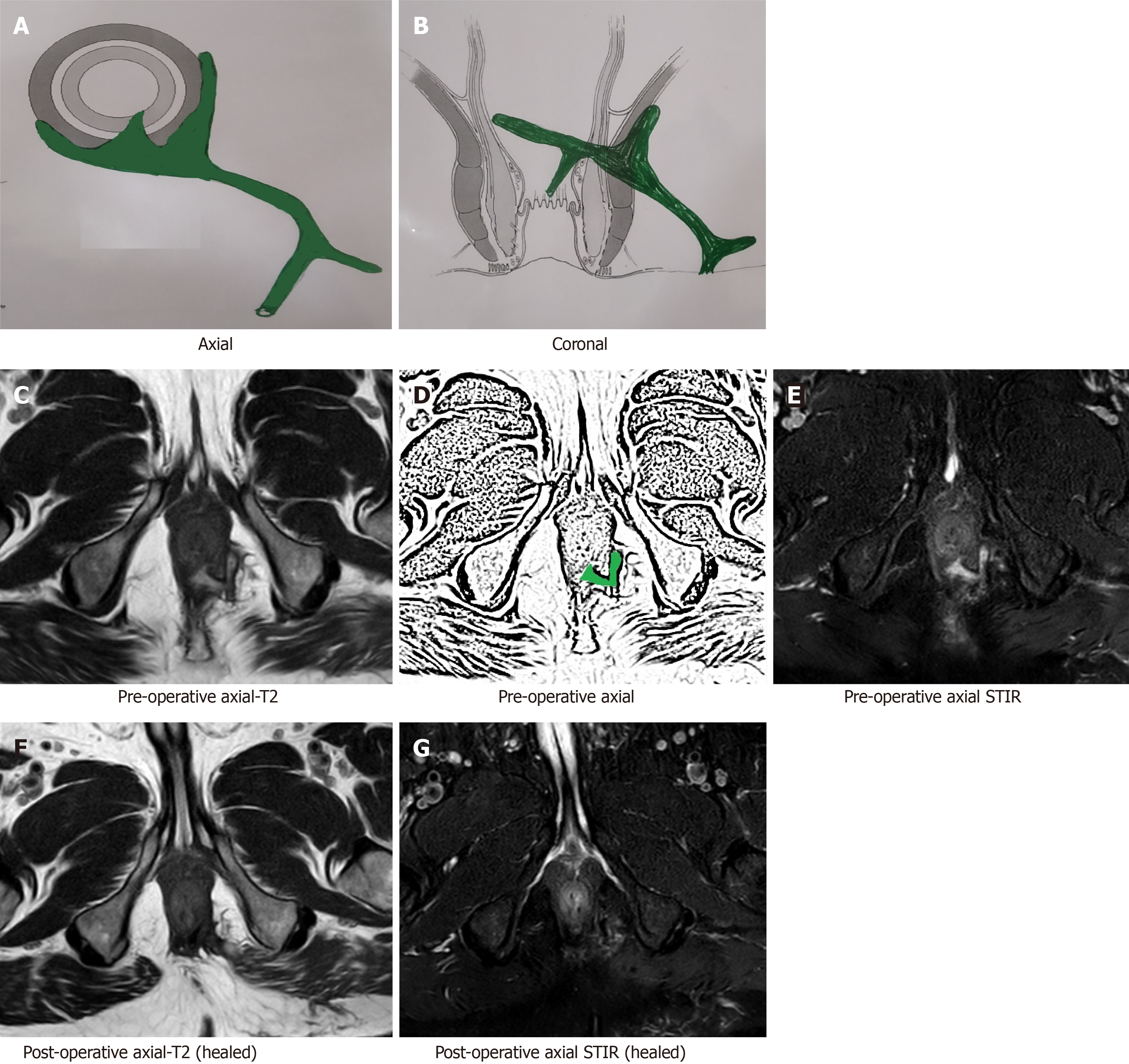
Figure 2 A 64-year-old male patient with a high transsphincteric fistula with multiple branches.
Magnetic resonance imaging (MRI) done after 19 wk post-surgery showing fistula has healed completely. The hyperintense signal (white) in the preoperative images has turned hypointense (black). A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Pre-operative T2-weighted axial MRI; D: Sketch of pre-operative axial MRI image highlighting internal opening and the intersphincteric portion of fistula tract (green color); E: Pre-operative short-T1 inversion recovery (STIR) axial MRI; F: Postoperative T2-weighted axial MRI (after 19 wk) showing completely healed fistula; G: Postoperative STIR axial MRI (after 19 wk) showing completely healed fistula. STIR: Short-T1 inversion recovery.
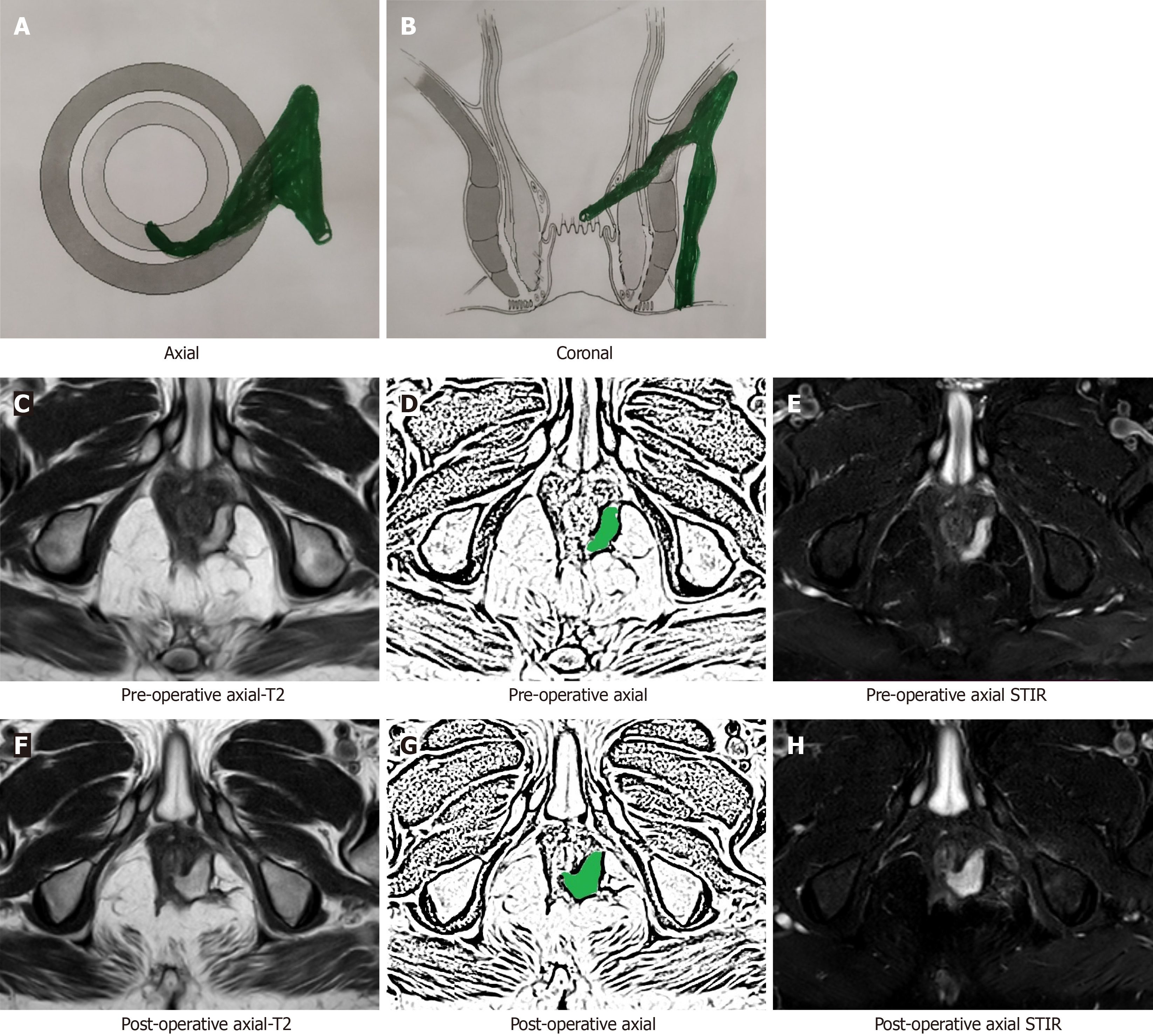
Figure 3 A 54-year-old male patient with a high transsphincteric fistula.
The fistula appeared to have ‘clinically’ healed as the external opening had closed with cessation of all pus. However, magnetic resonance imaging (MRI) done after 28 wk post-surgery showed patent internal opening and widening of intersphincteric portion of fistula tract. A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Pre-operative T2-weighted MRI; D: Sketch of pre-operative axial MRI image highlighting internal opening and the intersphincteric portion of fistula tract (green color); E: Pre-operative short-T1 inversion recovery (STIR) axial MRI; F: Postoperative T2-weighted axial MRI (after 28 wk) showing patent internal opening and persistent intersphincteric portion of fistula tract; G: Sketch of postoperative axial MRI image highlighting patent internal opening and persistent intersphincteric portion of fistula tract; H: Postoperative STIR axial MRI (after 28 wk) showing patent internal opening and persistent intersphincteric portion of fistula tract. STIR: Short-T1 inversion recovery.
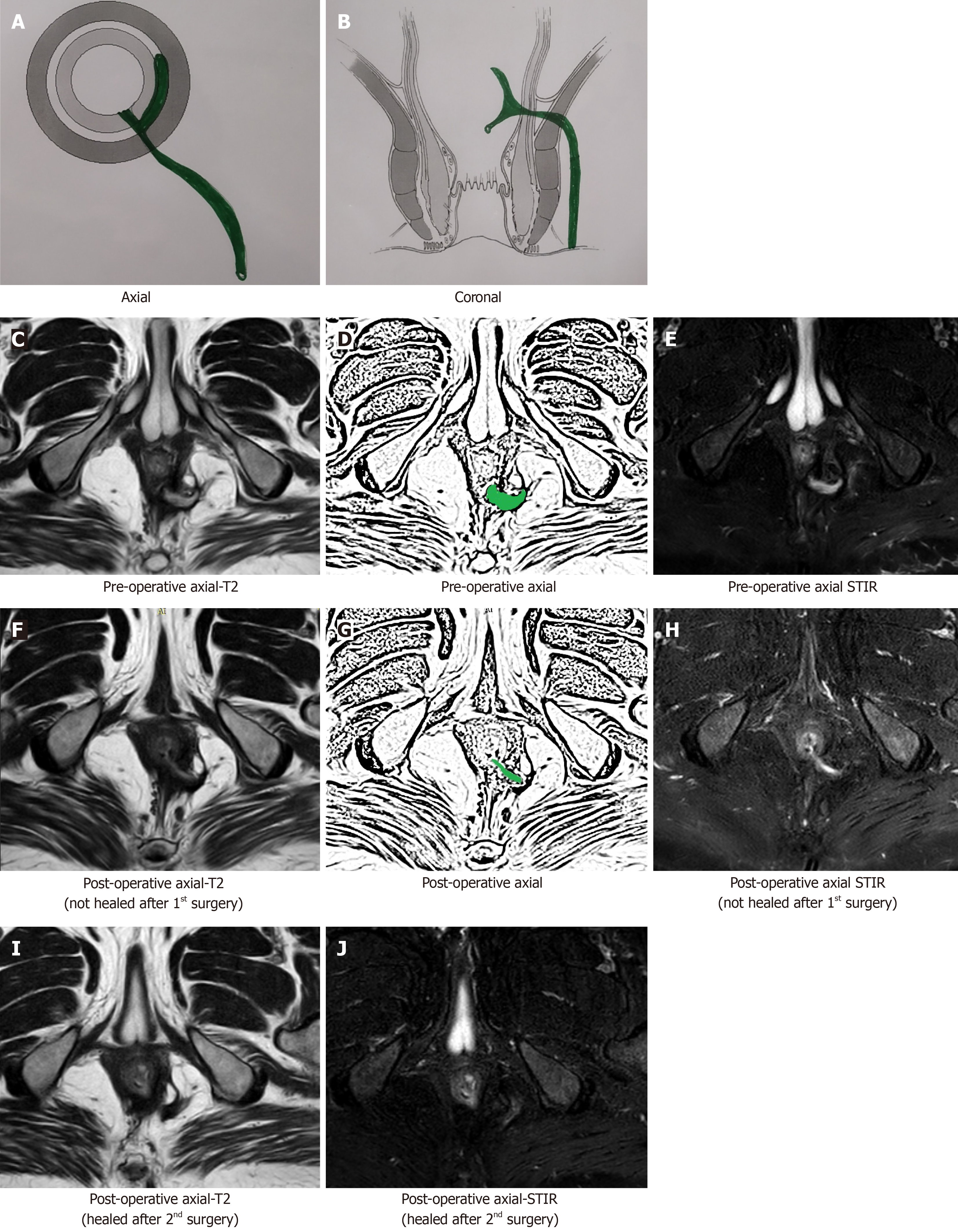
Figure 4 A 47-year-old male patient with a high transsphincteric fistula with supralevator extension.
The fistula appeared to have ‘clinically’ healed as the external opening had closed with cessation of all pus. Magnetic resonance imaging (MRI) done after 26 wk post-surgery showed patent internal opening and active intersphincteric portion of the fistula tract [hyperintense on T2 and short-T1 inversion recovery (STIR)]. The patient was operated again. MRI done after 14 wk after 2nd surgery showed fistula has healed completely. The hyperintense signal (white) in the preoperative images has turned hypointense (black). A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Pre-operative T2-weighted MRI; D: Sketch of pre-operative axial MRI image highlighting internal opening and the intersphincteric portion of fistula tract (green color); E: Pre-operative STIR axial MRI; F: Postoperative (26 wk after 1st surgery) T2-weighted axial MRI showing patent internal opening and persistent intersphincteric portion of fistula tract; G: Sketch highlighting patent internal opening and intersphincteric portion of fistula tract (green color); H: Postoperative (26 wk after 1st surgery) STIR axial MRI showing patent internal opening and persistent intersphincteric portion of fistula tract; I: Postoperative (14 wk after 2nd surgery) T2-weighted axial MRI showing completely healed fistula; J: Postoperative (14 wk after 2nd surgery) STIR axial MRI showing completely healed fistula. STIR: Short-T1 inversion recovery.
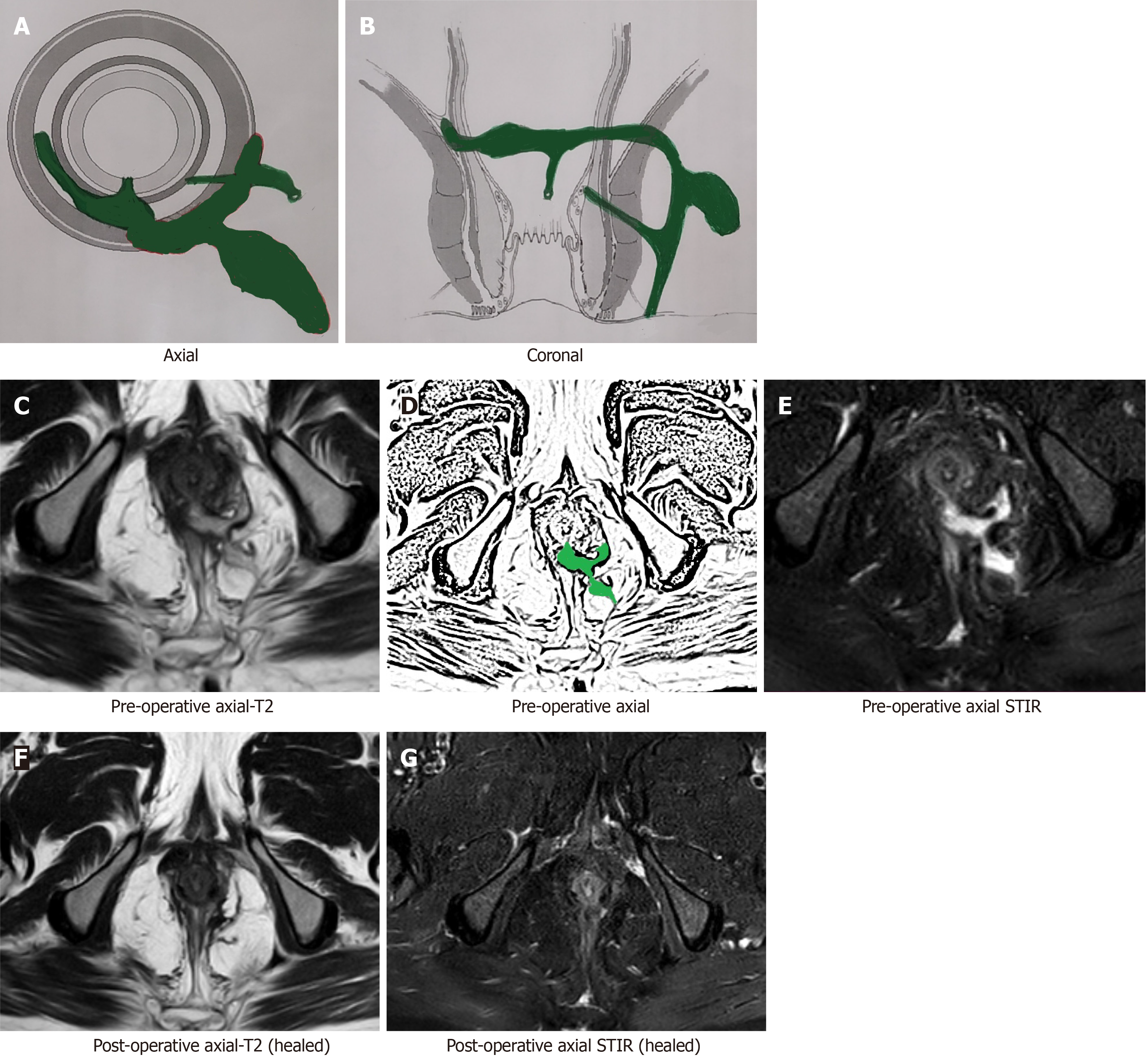
Figure 5 A 51-year-old male patient with a high transsphincteric fistula with multiple branches.
Magnetic resonance imaging (MRI) done after 8 wk post-surgery showing fistula has healed completely. The hyperintense signal (white) in the preoperative images has turned hypointense (black). A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Pre-operative T2-weighted axial MRI; D: Sketch of pre-operative axial MRI image highlighting internal opening, the intersphincteric portion of fistula tract and transsphincteric fistula tract (green color); E: Pre-operative short-T1 inversion recovery (STIR) axial MRI; F: Postoperative T2-weighted axial MRI (after 8 wk) showing completely healed fistula; G: Postoperative STIR axial MRI (after 8 wk) showing completely healed fistula. STIR: Short-T1 inversion recovery.
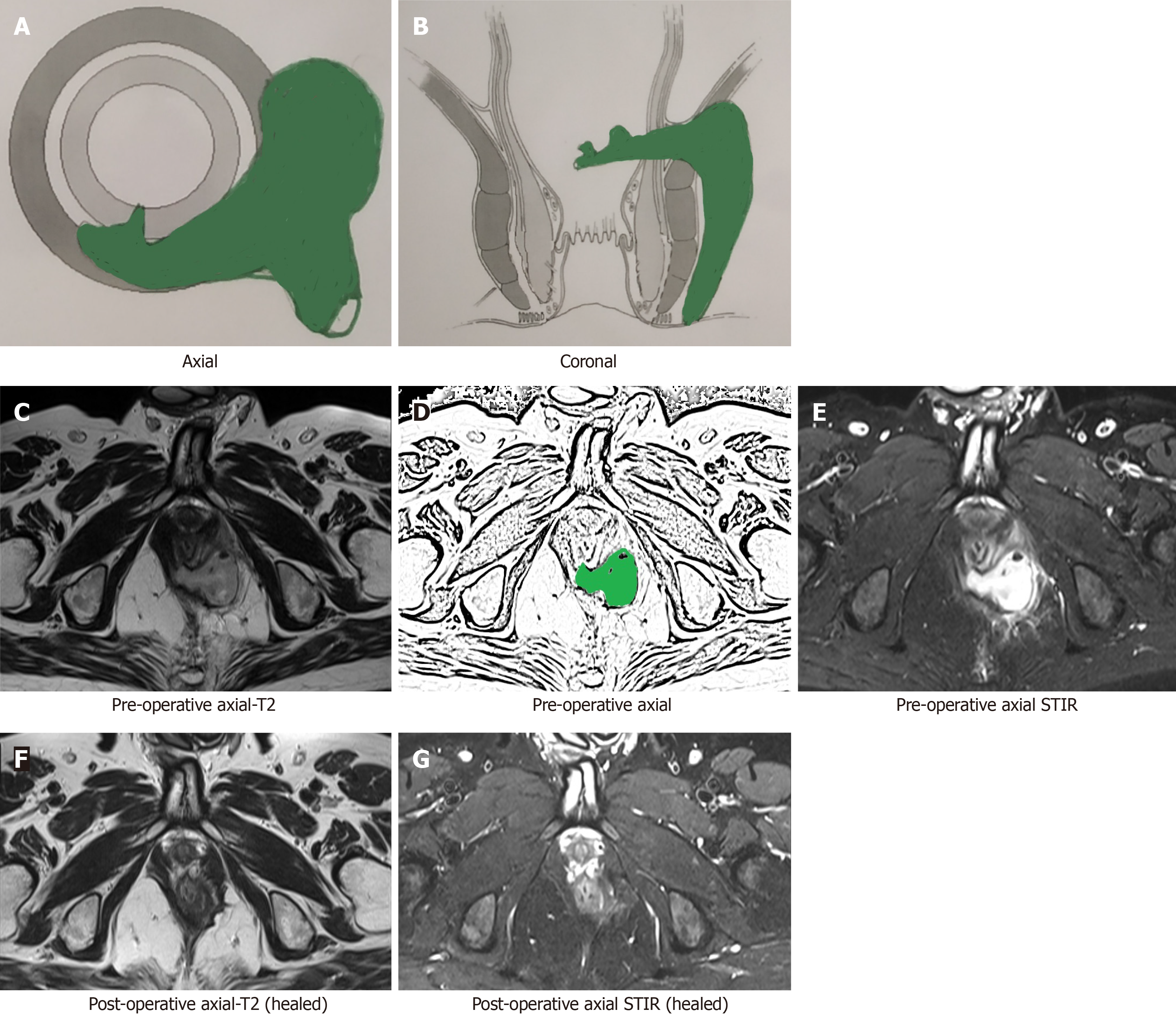
Figure 6 A 40-year-old male patient with a suprasphincteric fistula.
Magnetic resonance imaging (MRI) done after 16 wk post-surgery showing fistula has healed completely. The hyperintense signal (white) in the preoperative images has turned hypointense (black). A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Pre-operative T2-weighted axial MRI; D: Sketch of pre-operative axial MRI image highlighting internal opening and the intersphincteric portion of fistula tract (green color); E: Pre-operative short-T1 inversion recovery (STIR) axial MRI; F: Postoperative T2-weighted axial MRI (after 16 wk) showing completely healed fistula; G: Postoperative STIR axial MRI (after 16 wk) showing completely healed fistula. STIR: Short-T1 inversion recovery.
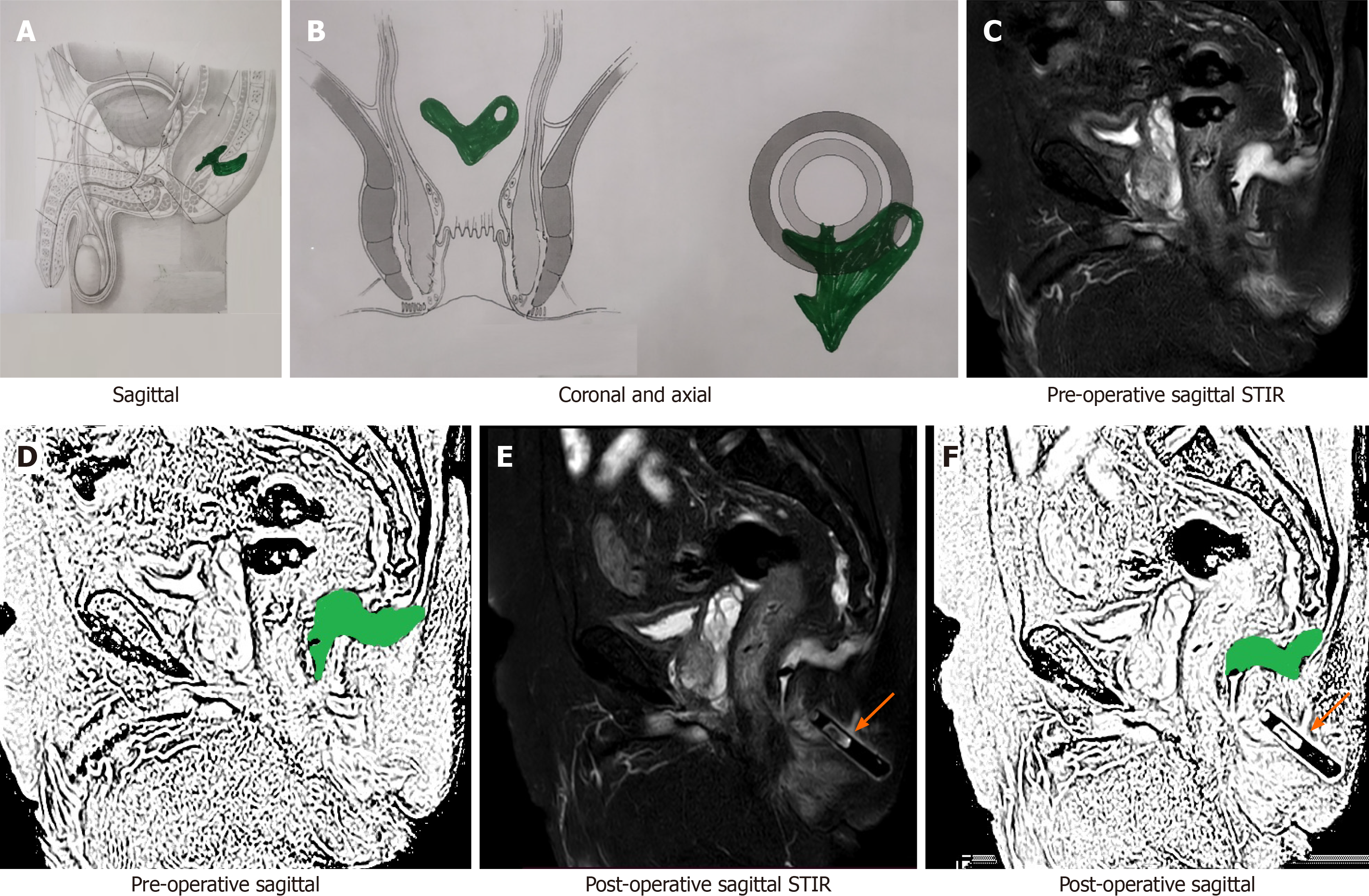
Figure 7 A 69-year-old male patient with a posterior fistula with a presacral abscess.
A wide bore drainage tube was inserted into the cavity intraoperatively. However, the patient did not improve. Postoperative check magnetic resonance imaging (MRI) demonstrated that the tube was in the wrong plane and the presacral abscess was not properly drained. A: Axial section (schematic diagram); B: Coronal section (schematic diagram); C: Preoperative short-T1 inversion recovery (STIR) sagittal MRI; D: Sketch of pre-operative sagittal MRI image highlighting anal fistula and presacral abscess (green color); E: Postoperative STIR sagittal MRI showing drainage tube in the wrong plane and persistent presacral abscess; F: Sketch of postoperative sagittal MRI highlighting persisting anal fistula and presacral abscess (green color) (orange arrows show the drainage tube). STIR: Short-T1 inversion recovery.
- Citation: Garg P, Kaur B, Yagnik VD, Dawka S, Menon GR. Guidelines on postoperative magnetic resonance imaging in patients operated for cryptoglandular anal fistula: Experience from 2404 scans. World J Gastroenterol 2021; 27(33): 5460-5473
- URL: https://www.wjgnet.com/1007-9327/full/v27/i33/5460.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i33.5460