Copyright
©The Author(s) 2021.
World J Gastroenterol. Aug 21, 2021; 27(31): 5201-5218
Published online Aug 21, 2021. doi: 10.3748/wjg.v27.i31.5201
Published online Aug 21, 2021. doi: 10.3748/wjg.v27.i31.5201
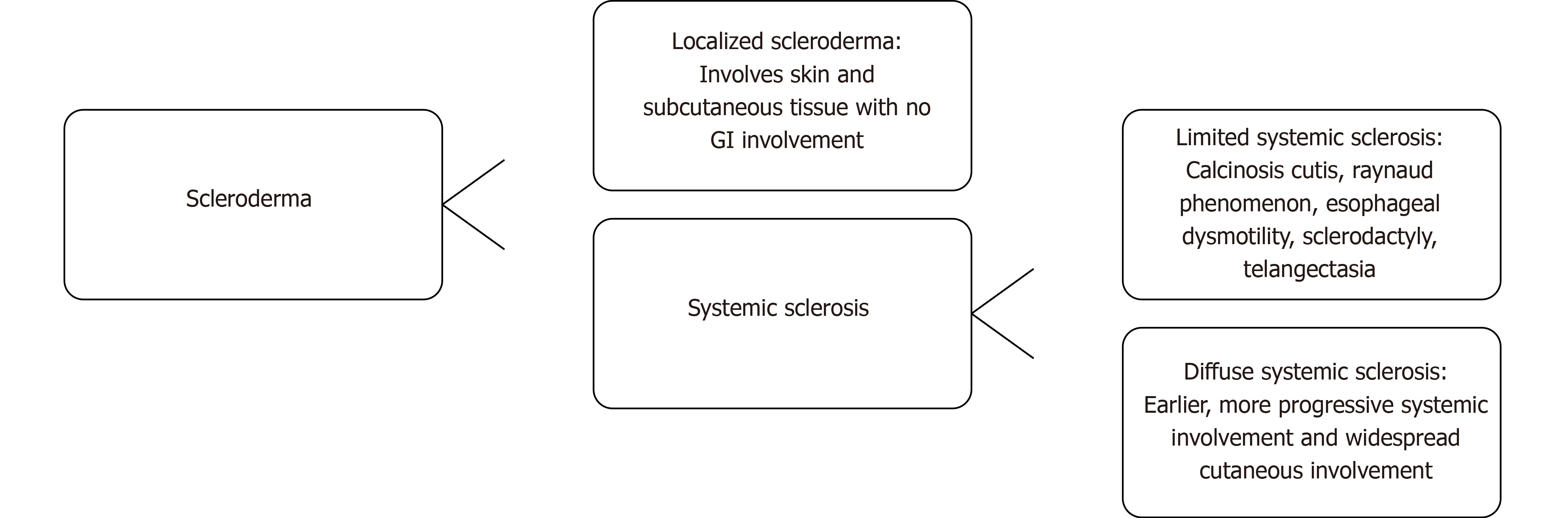
Figure 1 The types of scleroderma and features of each disease.
Scleroderma can be broken down into localized scleroderma or systemic sclerosis. Systemic sclerosis can be further broken down into limited and diffuse types. GI: Gastrointestinal.
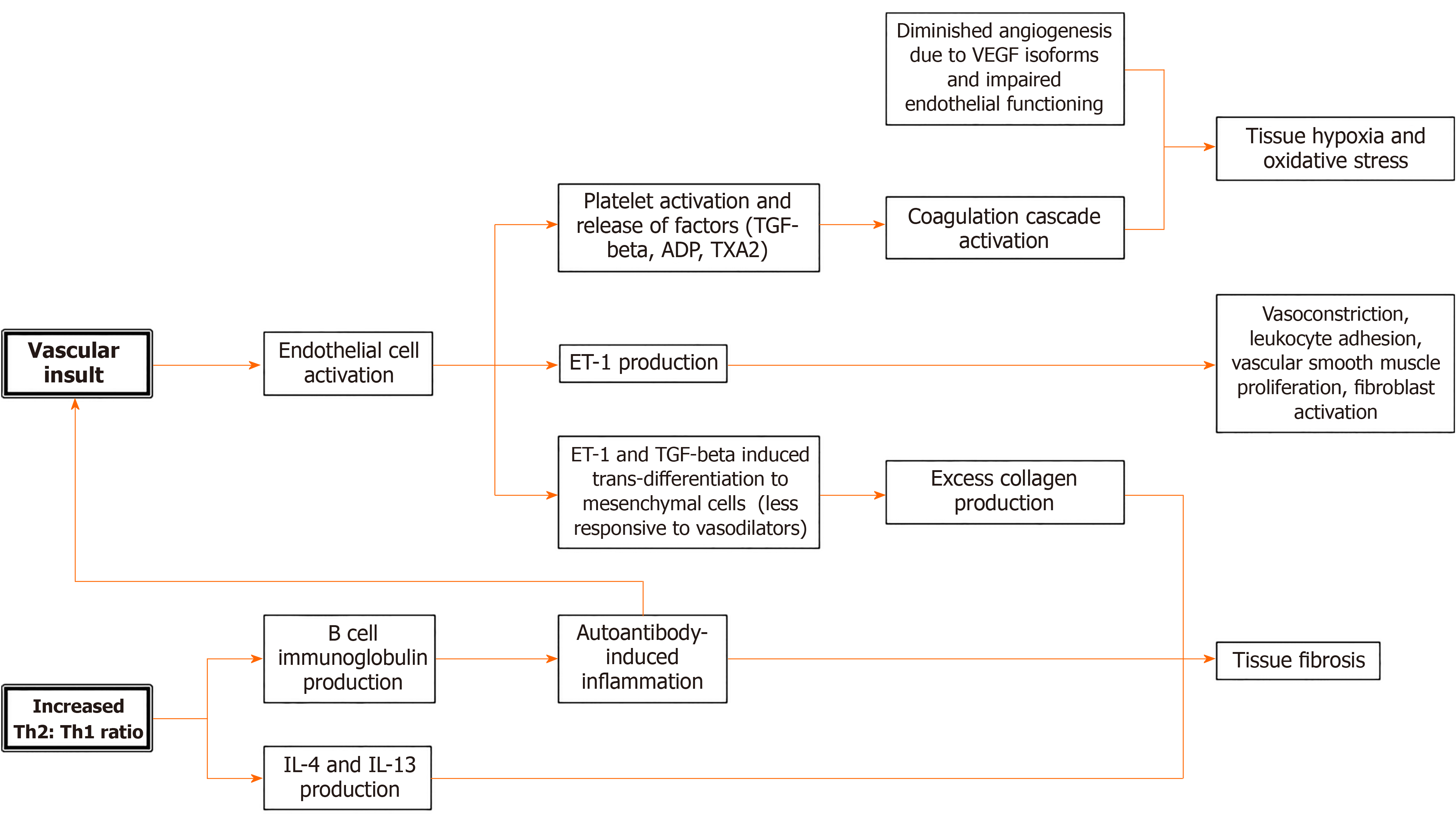
Figure 2 Simplified pathophysiology of systemic sclerosis.
SSc: Systemic sclerosis; Th2: Type 2 T helper; Th1: Type 1 T helper; TGF-beta: Transforming growth factor beta; TXA2: Thromboxane A2; ET-1: Endothelin 1; VEGF: Vascular endothelial growth factor; IL: Interleukin.
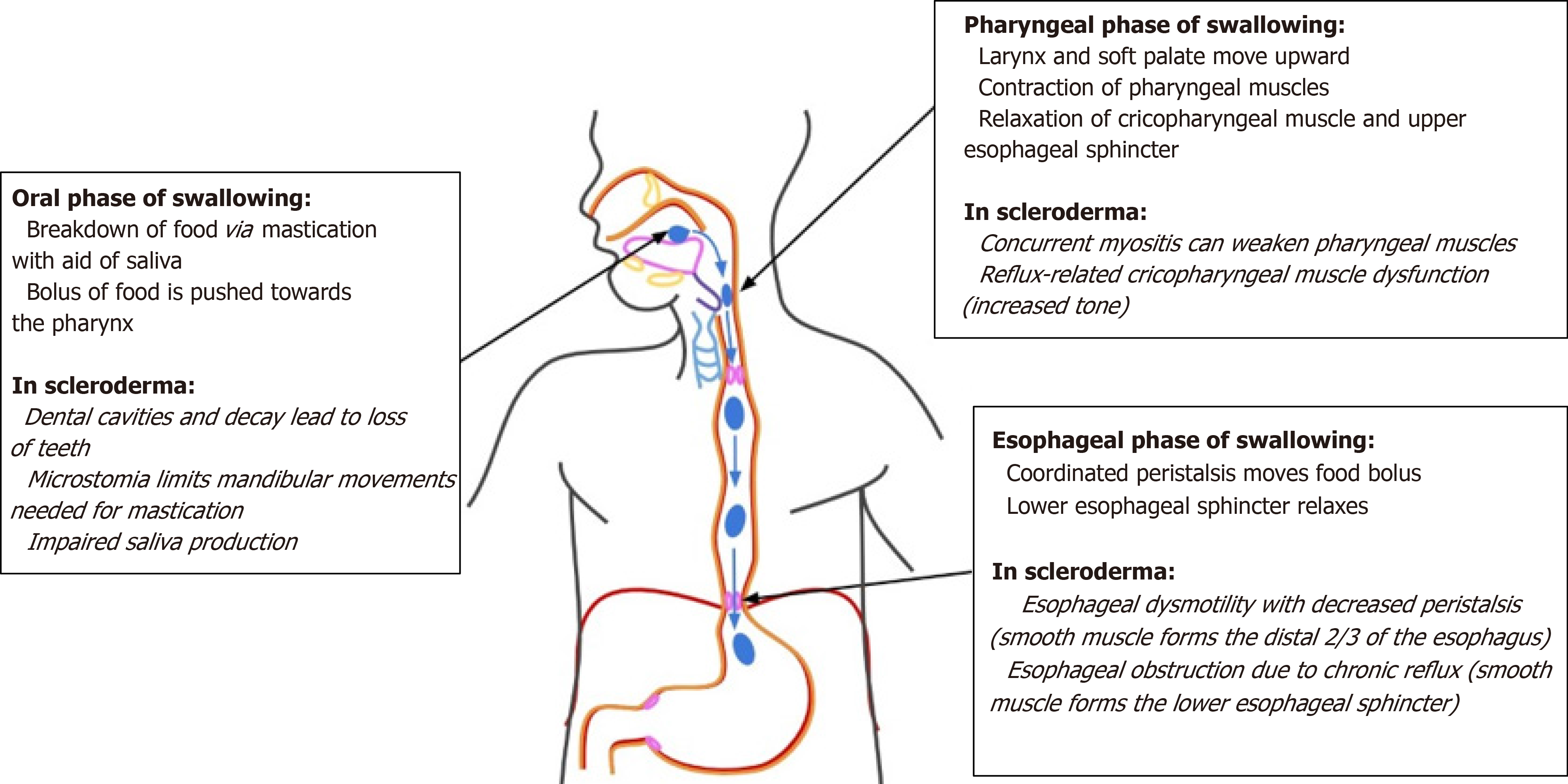
Figure 3 Disruptions of normal swallowing physiology due to disease processes of scleroderma.
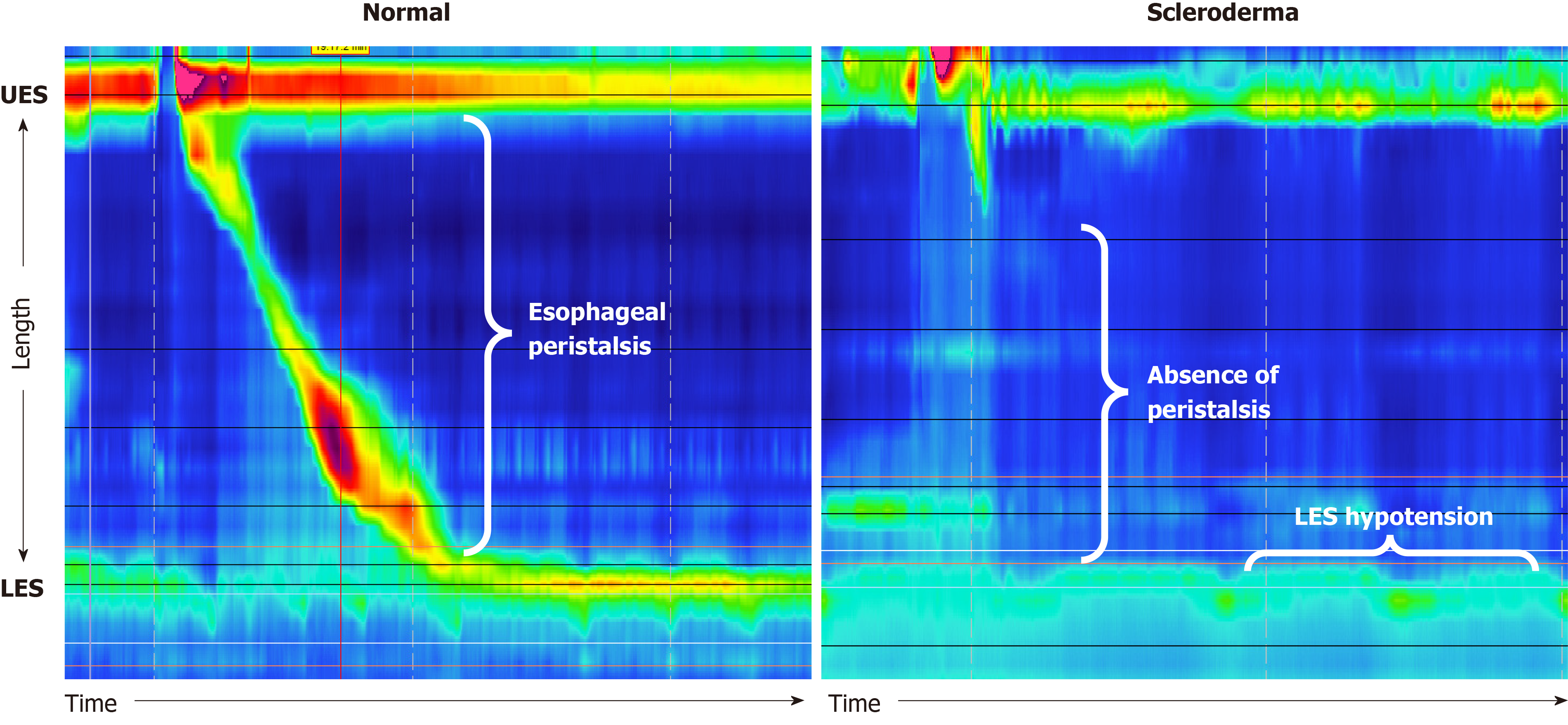
Figure 4 Normal manometry findings showing peristalsis during swallowing and lower esophageal sphincter tone compared to manometry findings in scleroderma showing an absence of peristalsis and lower esophageal sphincter hypotension.
LES: Lower esophageal sphincter; UES: Upper esophageal sphincter.
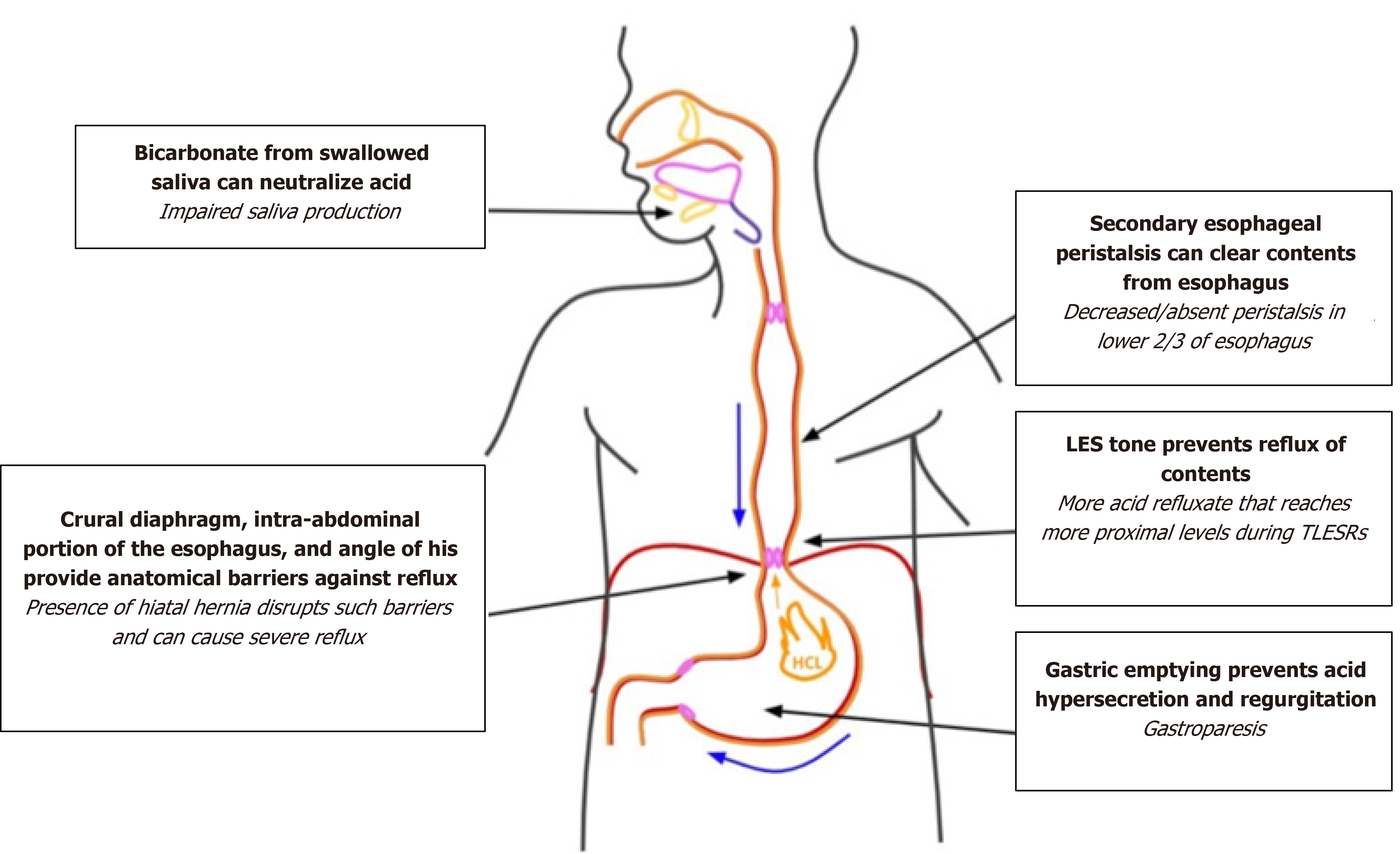
Figure 5 Disturbances of defense mechanisms against reflux in scleroderma.
LES: Lower esophageal sphincter.
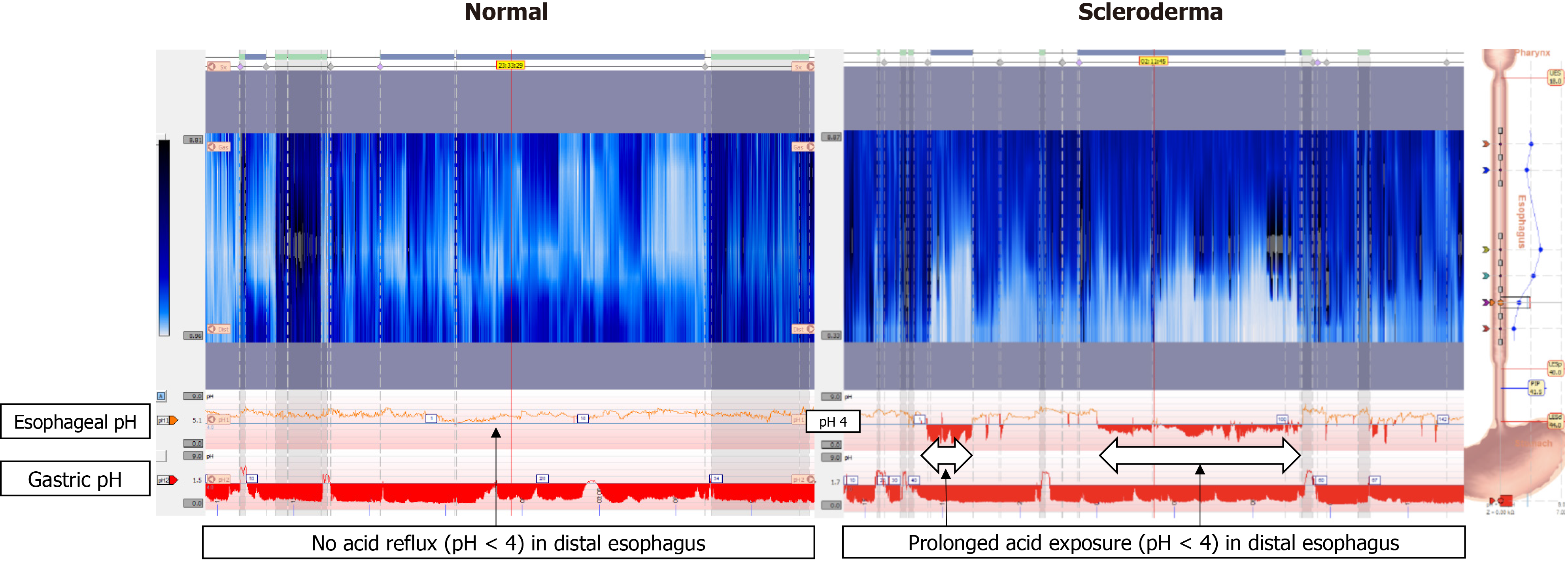
Figure 6 Twenty-four hour impedance pH monitoring normal findings compared to findings in scleroderma.
In normal esophagus, there are no episodes of acid reflux, as indicated by no drops of pH below 4 in the esophagus. In scleroderma esophagus, there is prolonged acid exposure in the distal esophagus.
- Citation: Kadakuntla A, Juneja A, Sattler S, Agarwal A, Panse D, Zakhary N, Pasumarthi A, Shapiro L, Tadros M. Dysphagia, reflux and related sequelae due to altered physiology in scleroderma. World J Gastroenterol 2021; 27(31): 5201-5218
- URL: https://www.wjgnet.com/1007-9327/full/v27/i31/5201.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i31.5201