Copyright
©The Author(s) 2021.
World J Gastroenterol. Jul 14, 2021; 27(26): 3984-4003
Published online Jul 14, 2021. doi: 10.3748/wjg.v27.i26.3984
Published online Jul 14, 2021. doi: 10.3748/wjg.v27.i26.3984
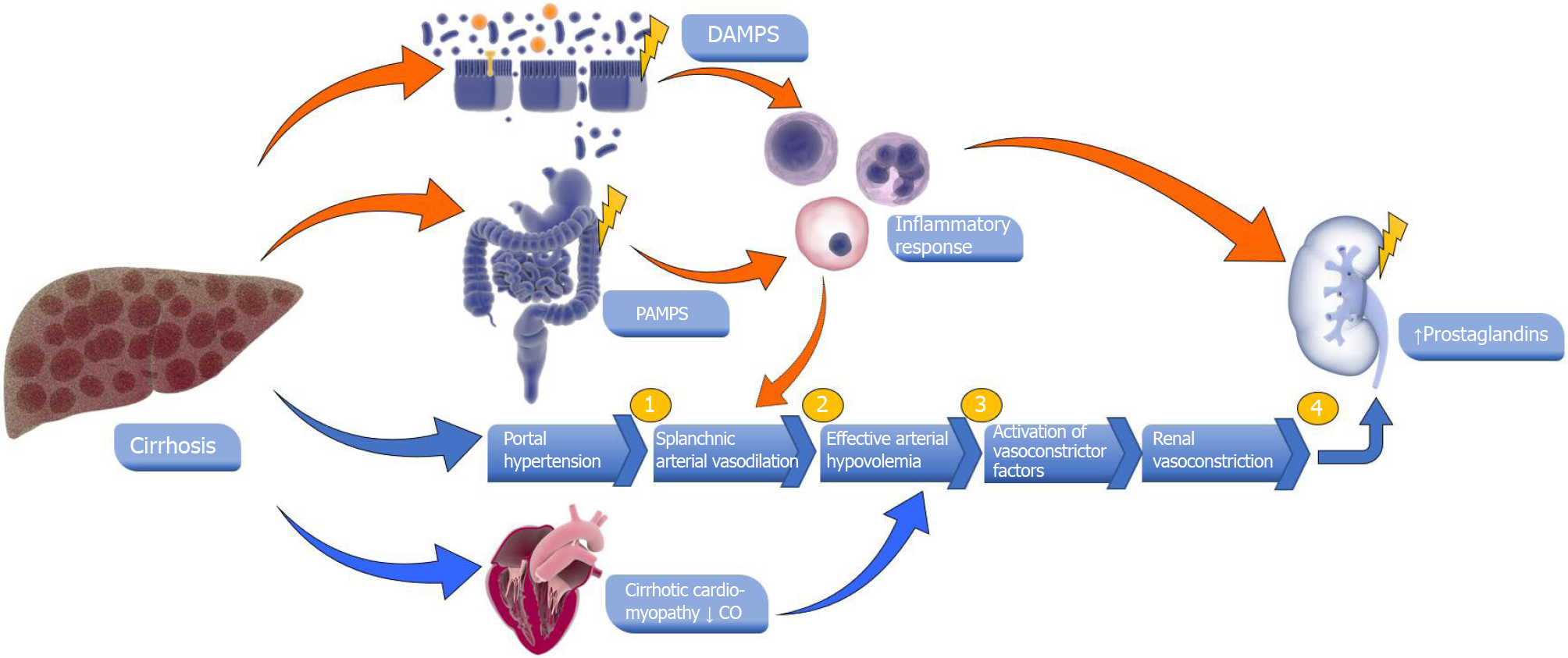
Figure 1 Pathogenesis of hepatorenal syndrome and acute kidney injury in cirrhosis.
(1) Patients with cirrhosis present with a marked splanchnic arterial vasodilation due to portal hypertension; (2) Splanchnic vasodilation causes a decrease in systemic vascular resistance leading to effective arterial hypovolemia; (3) There is activation of endogenous vasoconstrictors such as the renin-angiotensin-aldosterone system, sympathetic nervous system and arginine vasopressin; and (4) The activation of these systems leads to renal vasoconstriction inducing a decrease in glomerular filtration rate and development of hepatorenal syndrome. A decrease in cardiac output may contribute to a decrease in effective arterial blood volume. Pathogen-associated molecular patterns and damage-associated molecular patterns, derived from bacterial translocation and from injured liver, may activate circulating innate immune cells, leading to an inflammatory response. The Inflammatory mediators may lead to impairment of circulatory dysfunction and consequently, kidney tissue damage. Library of Science & Medical Illustrations were utilized in part to create this figure (https://creativecommons.org/Licenses/by-nc-sa/4.0/). DAMPs: Damage-associated molecular patterns; PAMPs: Pathogen-associated molecular patterns.
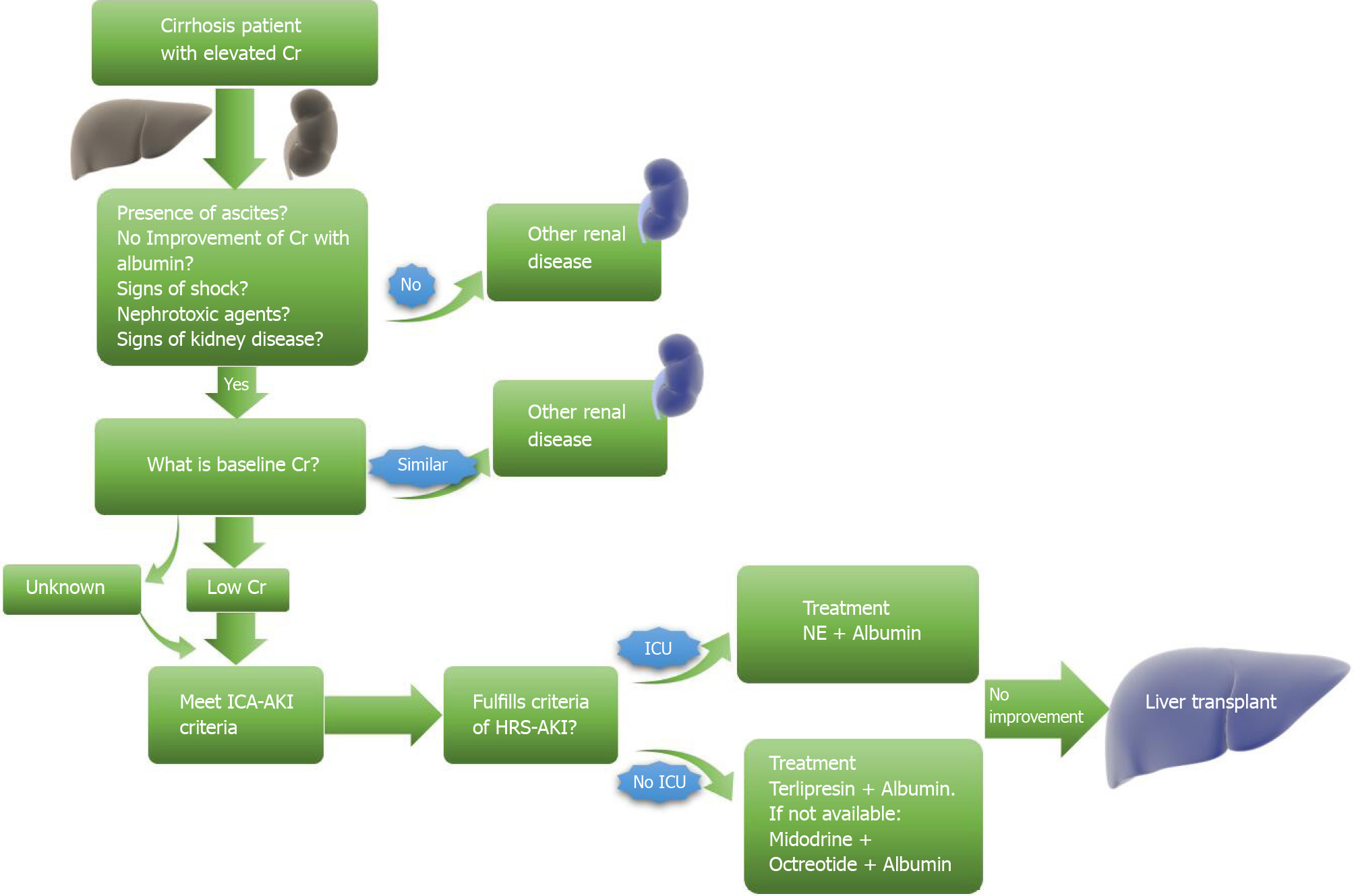
Figure 2 Algorithm of the diagnosis and treatment of hepatorenal syndrome.
The algorithm indicates differential diagnosis, diagnosis of hepatorenal syndrome (HRS) and HRS treatment. Library of Science & Medical Illustrations were utilized in part to create this figure (https://creativecommons.org/Licenses/by-nc-sa/4.0/). Cr: Creatinine; ICA: International club ascites; AKI: Acute kidney injury; HRS: Hepatorenal syndrome; ICU: Intensive care unit; NE: Norepinephrine.
- Citation: Gupta K, Bhurwal A, Law C, Ventre S, Minacapelli CD, Kabaria S, Li Y, Tait C, Catalano C, Rustgi VK. Acute kidney injury and hepatorenal syndrome in cirrhosis. World J Gastroenterol 2021; 27(26): 3984-4003
- URL: https://www.wjgnet.com/1007-9327/full/v27/i26/3984.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i26.3984