Copyright
©The Author(s) 2021.
World J Gastroenterol. Apr 7, 2021; 27(13): 1321-1329
Published online Apr 7, 2021. doi: 10.3748/wjg.v27.i13.1321
Published online Apr 7, 2021. doi: 10.3748/wjg.v27.i13.1321
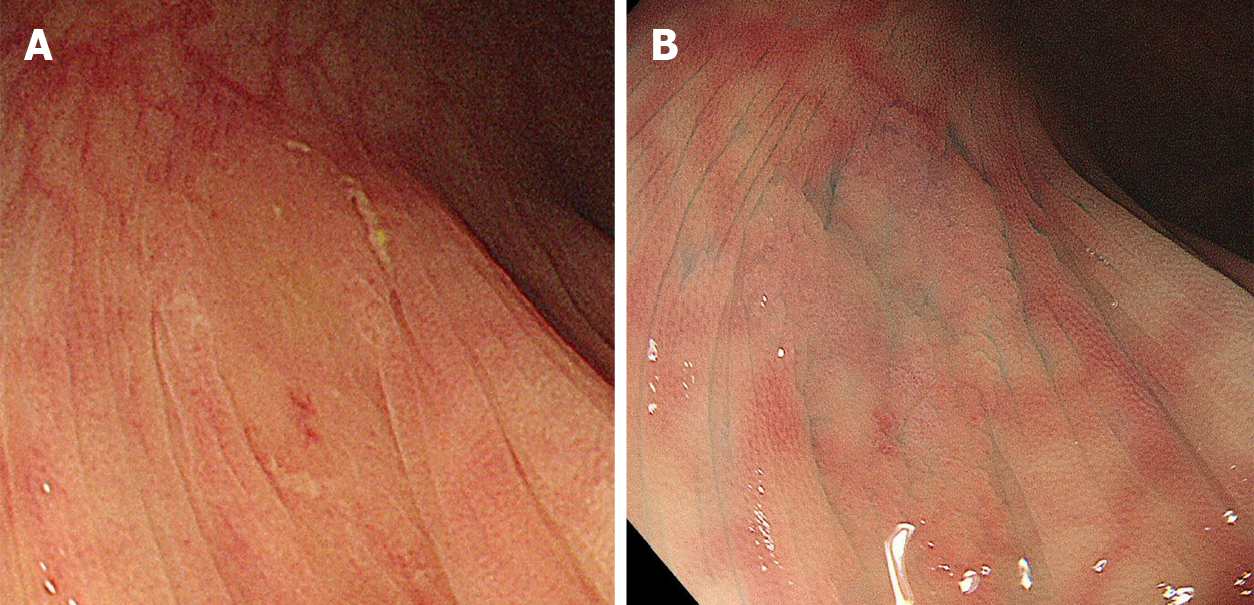
Figure 1 Endoscopic findings regarding sessile serrated lesions.
A: ‘‘Mucus cap’’ was defined as coverage with abundant mucus; and B: Indistinct borders were defined as vague demarcations of the lesion border.
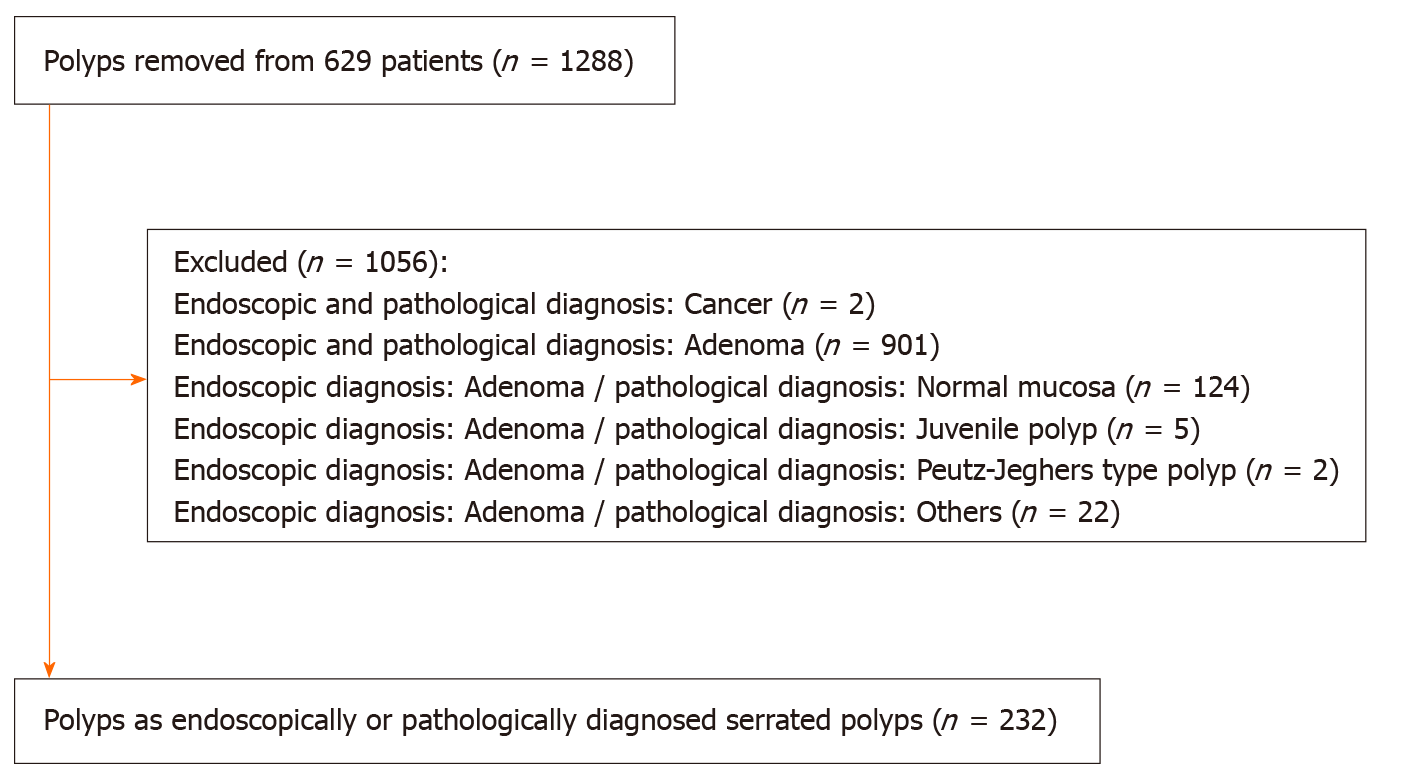
Figure 2
Flowchart of polyp enrollment.
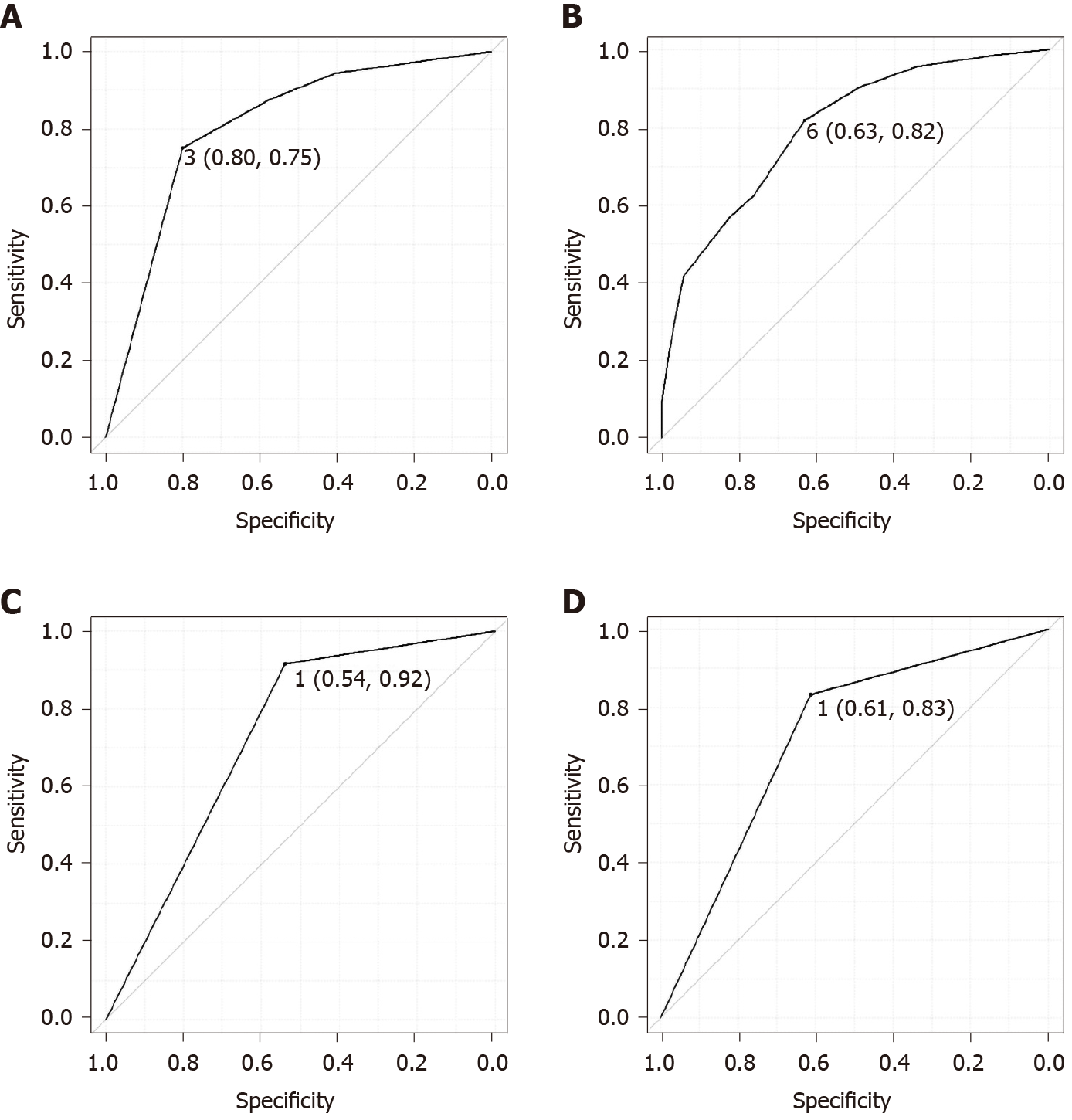
Figure 3 Receiver-operating characteristic curve for predicting sessile serrated lesions.
A: Receiver-operating characteristic (ROC) curve for predicting sessile serrated lesion (SSL) based on the endoscopic SSL diagnosis score: The area under the curve (AUC) was 0.806. The optimal cutoff value was 3, for which the endoscopic SSL diagnosis score predicted pathological SSLs with 75% sensitivity and 80% specificity; B: ROC curve for predicting SSL based on polyp size: AUC was 0.801. Size ≥ 6 mm predicted pathological SSLs with 82% sensitivity, and 63% specificity; C: ROC curve for predicting SSL based on mucus cap: AUC was 0.727. The presence of mucus cap predicted pathological SSLs with 92% sensitivity, and 54% specificity; and D: ROC curve for predicting SSL based on indistinct borders: AUC was 0.723. The presence of indistinct borders predicted pathological SSLs with 83% sensitivity, and 61% specificity.
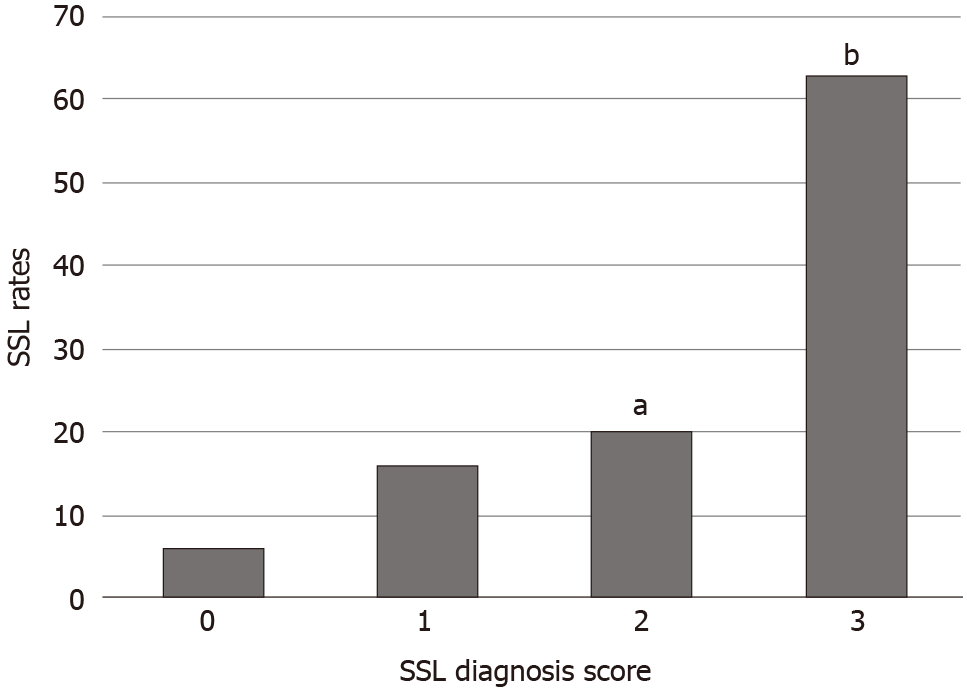
Figure 4 Sessile serrated lesion diagnosis rates based on the endoscopic sessile serrated lesion diagnosis score.
aP < 0.05 compared to an endoscopic Sessile serrated lesion diagnosis score of 0; bP < 0.001 compared to an endoscopic sessile serrated lesion diagnosis score of 0, 1, or 2. SSL: Sessile serrated lesion.
- Citation: Nishizawa T, Yoshida S, Toyoshima A, Yamada T, Sakaguchi Y, Irako T, Ebinuma H, Kanai T, Koike K, Toyoshima O. Endoscopic diagnosis for colorectal sessile serrated lesions. World J Gastroenterol 2021; 27(13): 1321-1329
- URL: https://www.wjgnet.com/1007-9327/full/v27/i13/1321.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i13.1321