Copyright
©The Author(s) 2020.
World J Gastroenterol. Dec 28, 2020; 26(48): 7707-7718
Published online Dec 28, 2020. doi: 10.3748/wjg.v26.i48.7707
Published online Dec 28, 2020. doi: 10.3748/wjg.v26.i48.7707
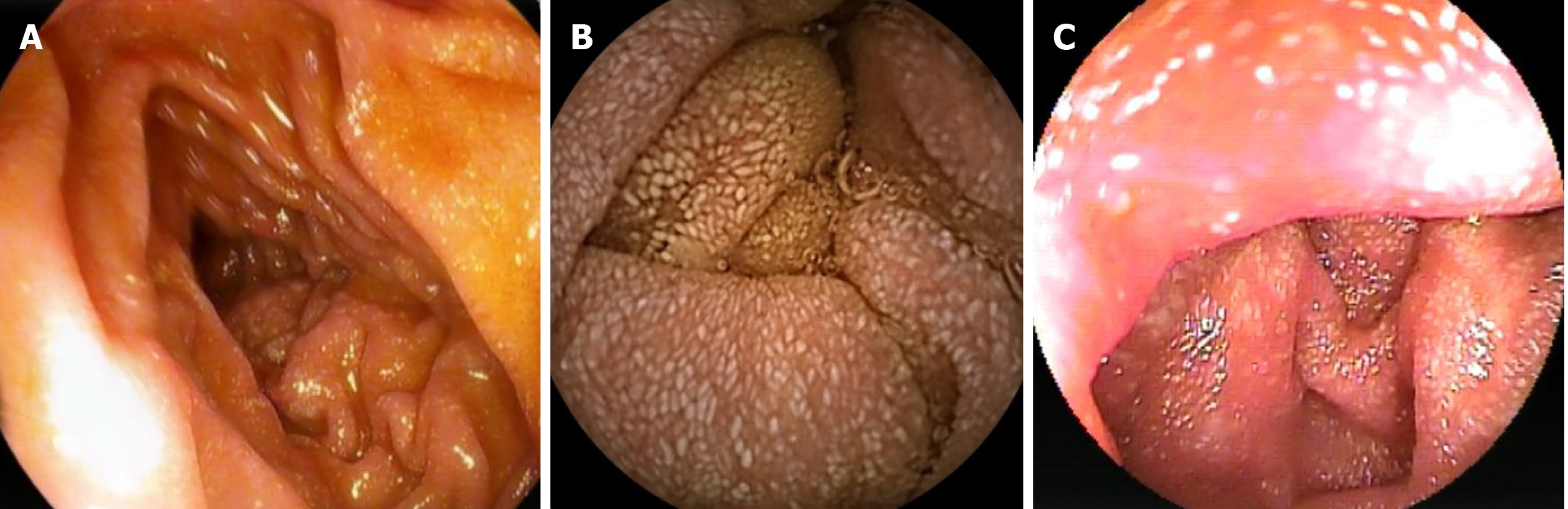
Figure 1 Imaging examinations.
A: Endoscopic view of the descending part of the duodenum showing spots of lymphangiectasia suggestive for lymphedema; B: Video capsule endoscopy with a snowflake appearance of the jejunum compatible with dilated mucosal lymphatic vessels; and C: Double-balloon enteroscopy of the jejunum with an almost identical image to video capsule endoscopy.
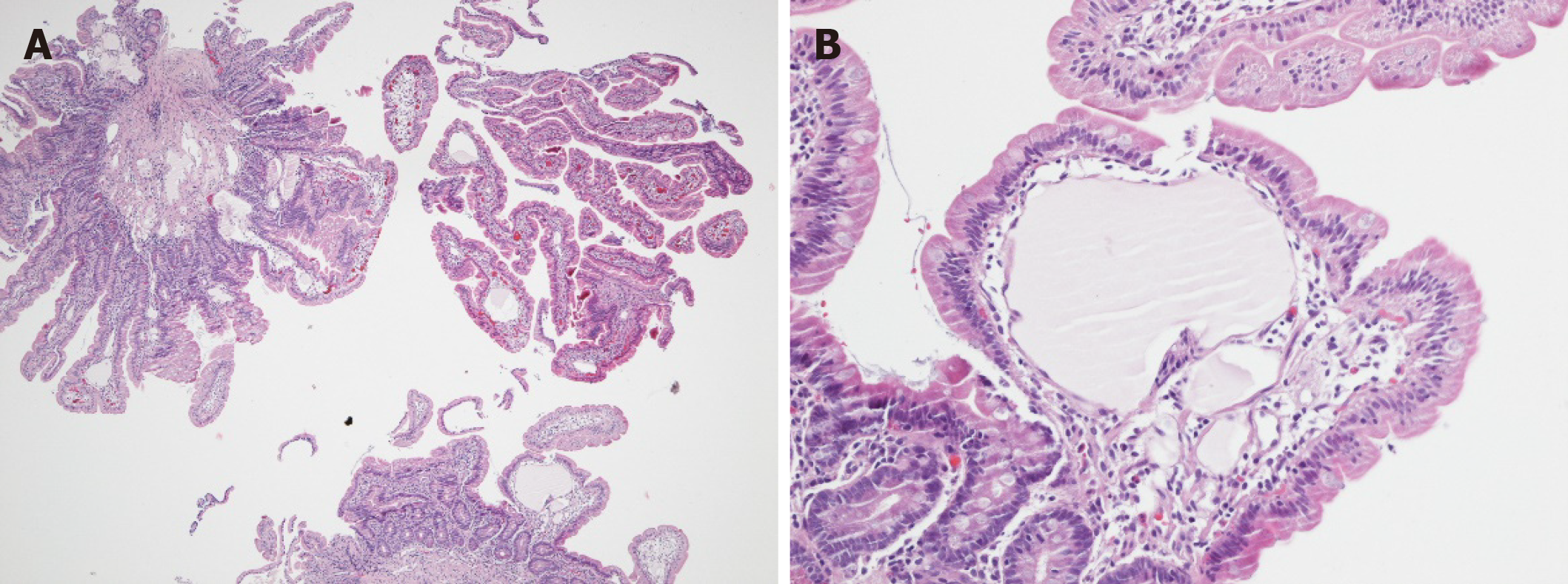
Figure 2 Histological and immunohistological analyses.
A: Jejunal biopsies showing a mild and focal blunting of the villi in particular above the prominent ecstatic mucosal lymph vessels (4-fold magnification); B: Ecstatic lymph vessel without inflammatory changes or abnormalities of the epithelial intestinal cell lining (200-fold magnification).
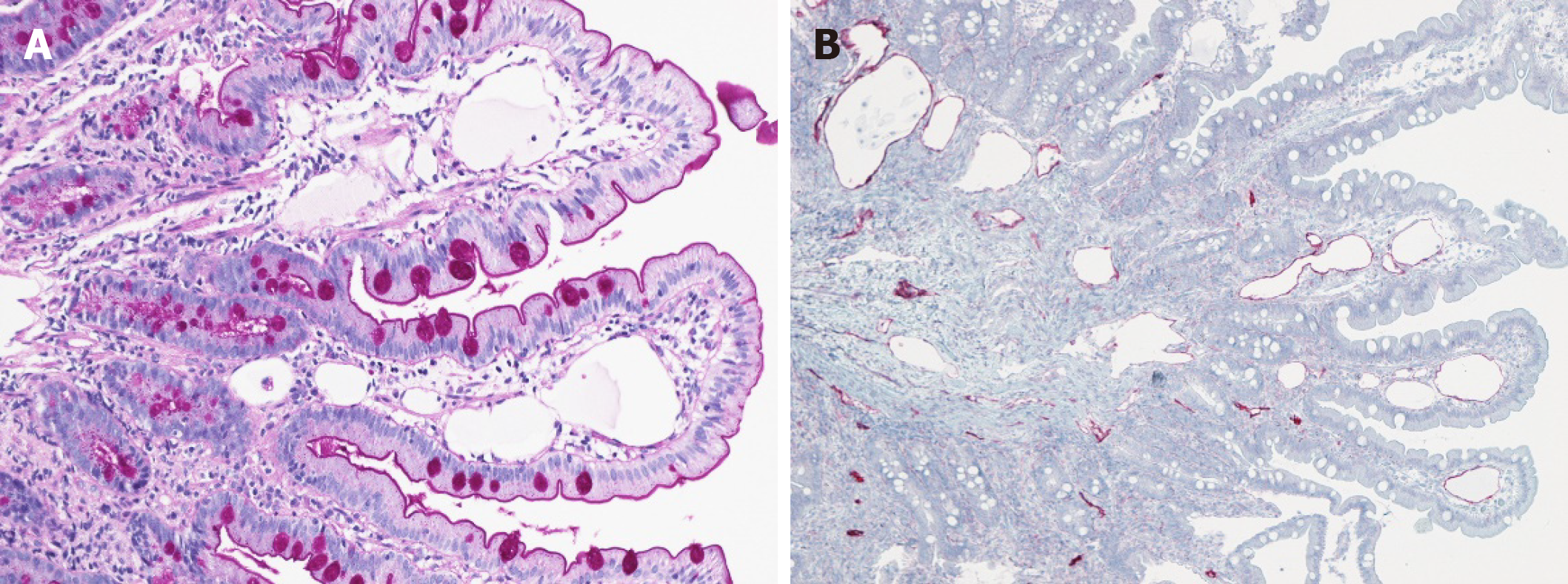
Figure 3 Histological and immunohistological analyses.
A: Periodic Acid-Schiff staining did not reveal any collections of periodic acid-schiff positive histiocytes or inclusions, demonstrating the perfectly normal intestinal brush border (200-fold magnification); B: Immunohistochemistry for D2-40, a marker of lymphatic endothelial cells, confirms the endothelium to be of lymphatic origin and highlights the presence of multiple ecstatic lymph vessels in both the mucosa and submucosa (100-fold magnification).
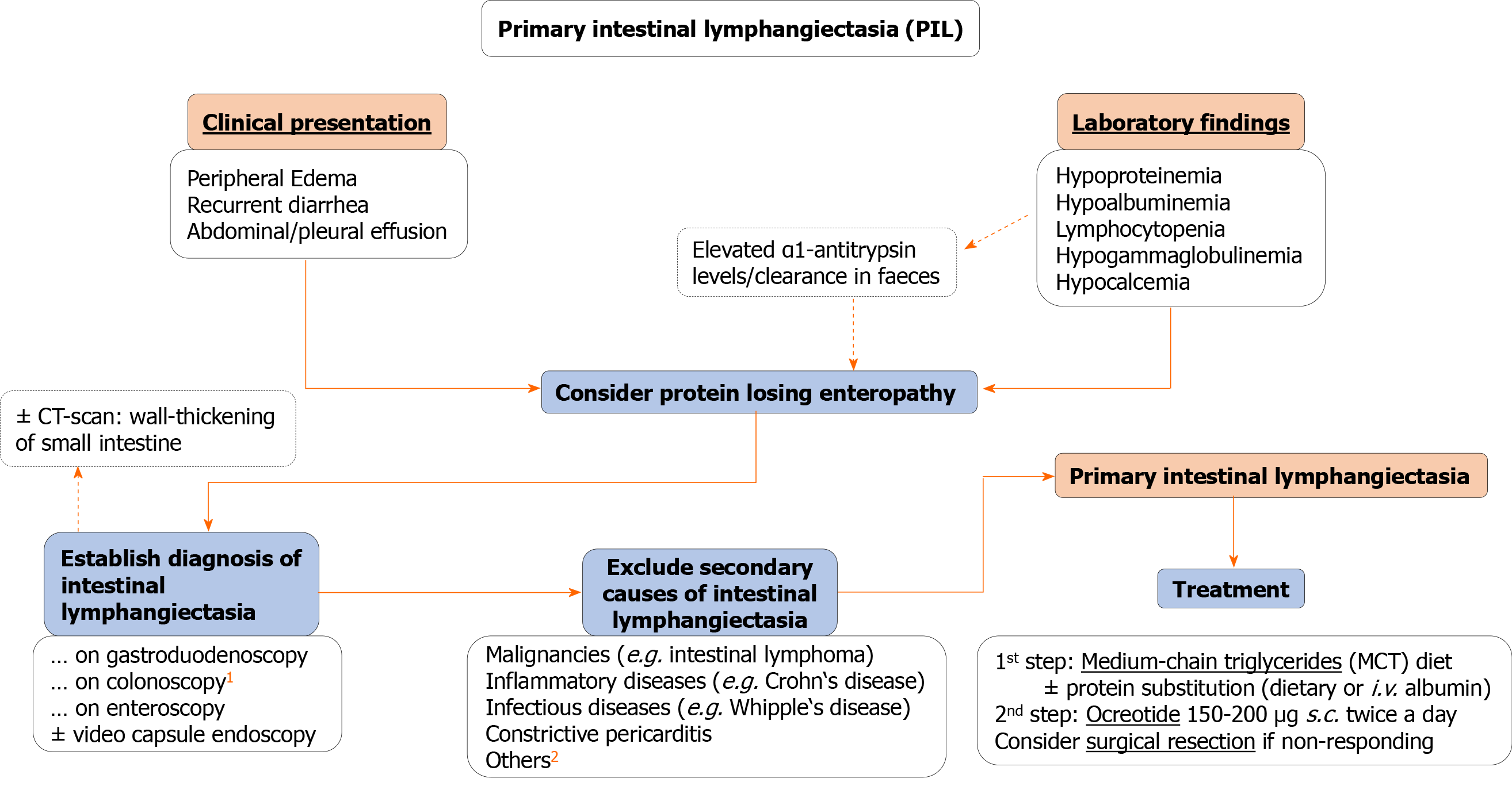
Figure 4 Proposed algorithm for diagnosis and therapy of primary intestinal lymphangiectasia in adults.
1Including intubation of the terminal ileum. 2Other secondary causes include: Retroperitoneal fibrosis following radio-/chemotherapy, sarcoidosis, intestinal tuberculosis, systemic sclerosis, human immunodeficiency virus-related enteropathy, Fontan-surgery.
- Citation: Huber R, Semmler G, Mayr A, Offner F, Datz C. Primary intestinal lymphangiectasia in an adult patient: A case report and review of literature. World J Gastroenterol 2020; 26(48): 7707-7718
- URL: https://www.wjgnet.com/1007-9327/full/v26/i48/7707.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i48.7707