Copyright
©The Author(s) 2020.
World J Gastroenterol. Nov 28, 2020; 26(44): 7005-7021
Published online Nov 28, 2020. doi: 10.3748/wjg.v26.i44.7005
Published online Nov 28, 2020. doi: 10.3748/wjg.v26.i44.7005
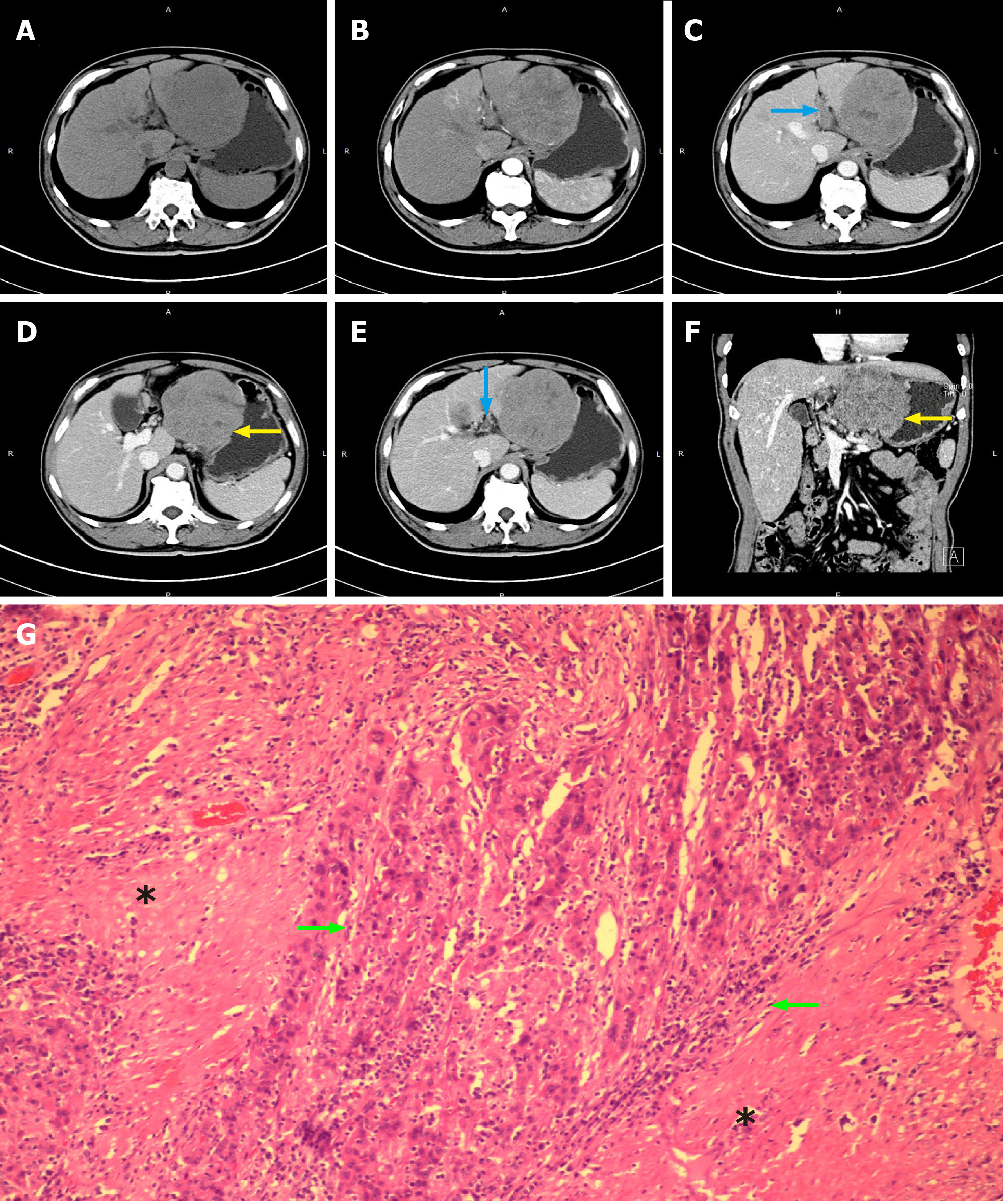
Figure 1 Computed tomography images of patient No.
1 who was diagnosed as hepatocellular carcinoma with microscopic tumor thrombus in bile duct. A, B: Xxxx; C-F: The blue arrows indicate the portal vein tumor thrombus (C and E) and the yellow arrows indicated the large hepatocellular carcinoma tumor which invaded the full thickness of the gastric wall (D and F); G: Bile duct tumor thrombus was only detectable under the microscope. The green arrows indicate bile duct tumor thrombus, and the black stars indicate the intrahepatic bile duct muscularis.
Figure 2 Positron emission tomography-computed tomography (A), computed tomography (B and C), and positron emission tomography (D and E) images of patient No.
2 who was diagnosed as recurrent hepatocellular carcinoma with bile duct tumor thrombus located in the common bile duct but did not have visible metastatic lesions in the liver. The blue arrow indicates the portal vein, the red arrow indicates the hepatic artery, and the green arrow indicates the bile duct tumor thrombus in common hepatic duct and common bile duct.
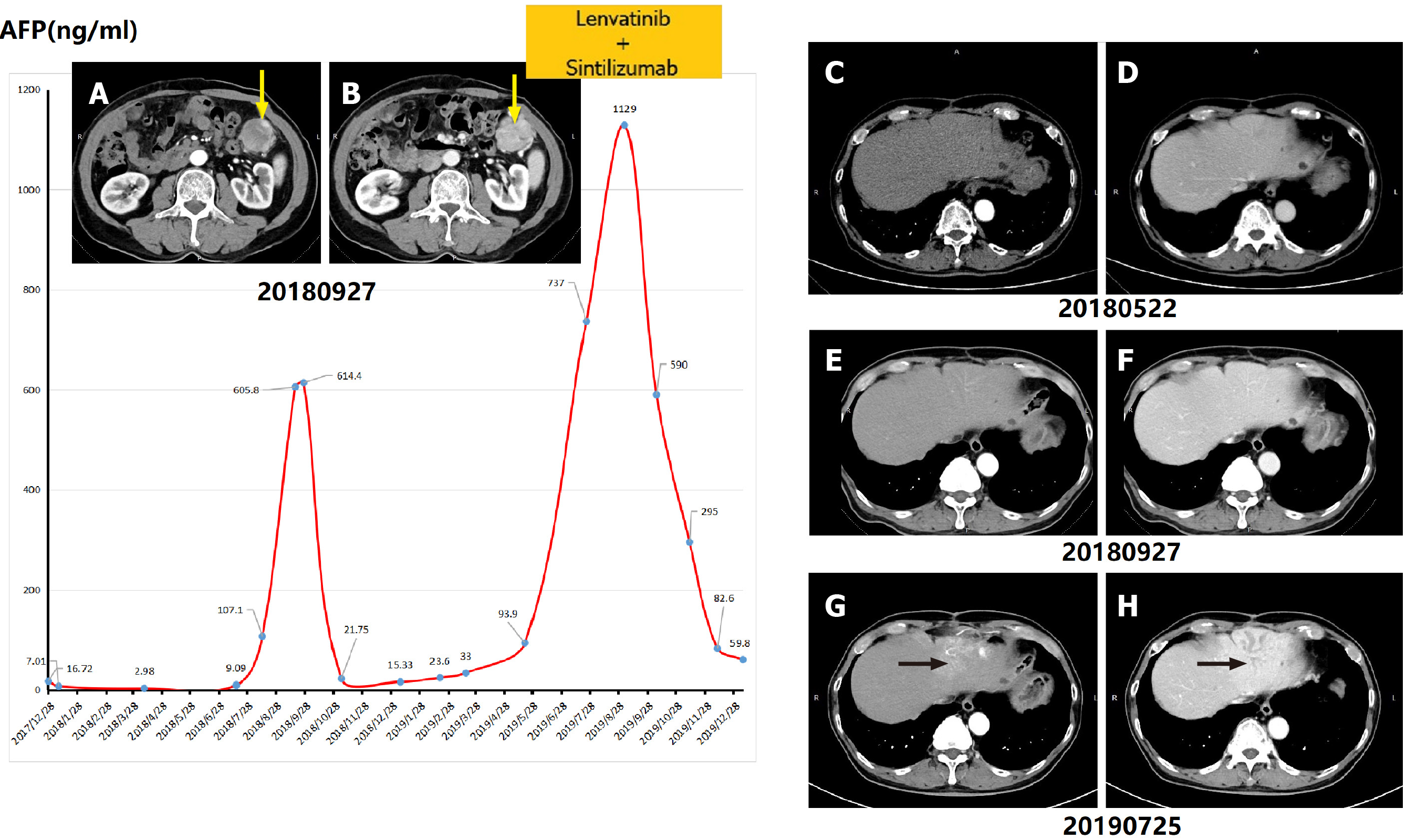
Figure 3 Variation trend of serum alpha-fetoprotein value and computed tomography images of patient No.
3. A, B: The yellow arrow indicated the first recurrent hepatocellular carcinoma lesion in the abdominal cavity in September 2018; C, D: Computed tomography images taken in May 2018 did not show any tumor lesion or dilated bile ducts in the liver parenchyma; G, H: The black arrows indicate the dilated intrahepatic bile ducts in June 2019. AFP: Alpha-fetoprotein.
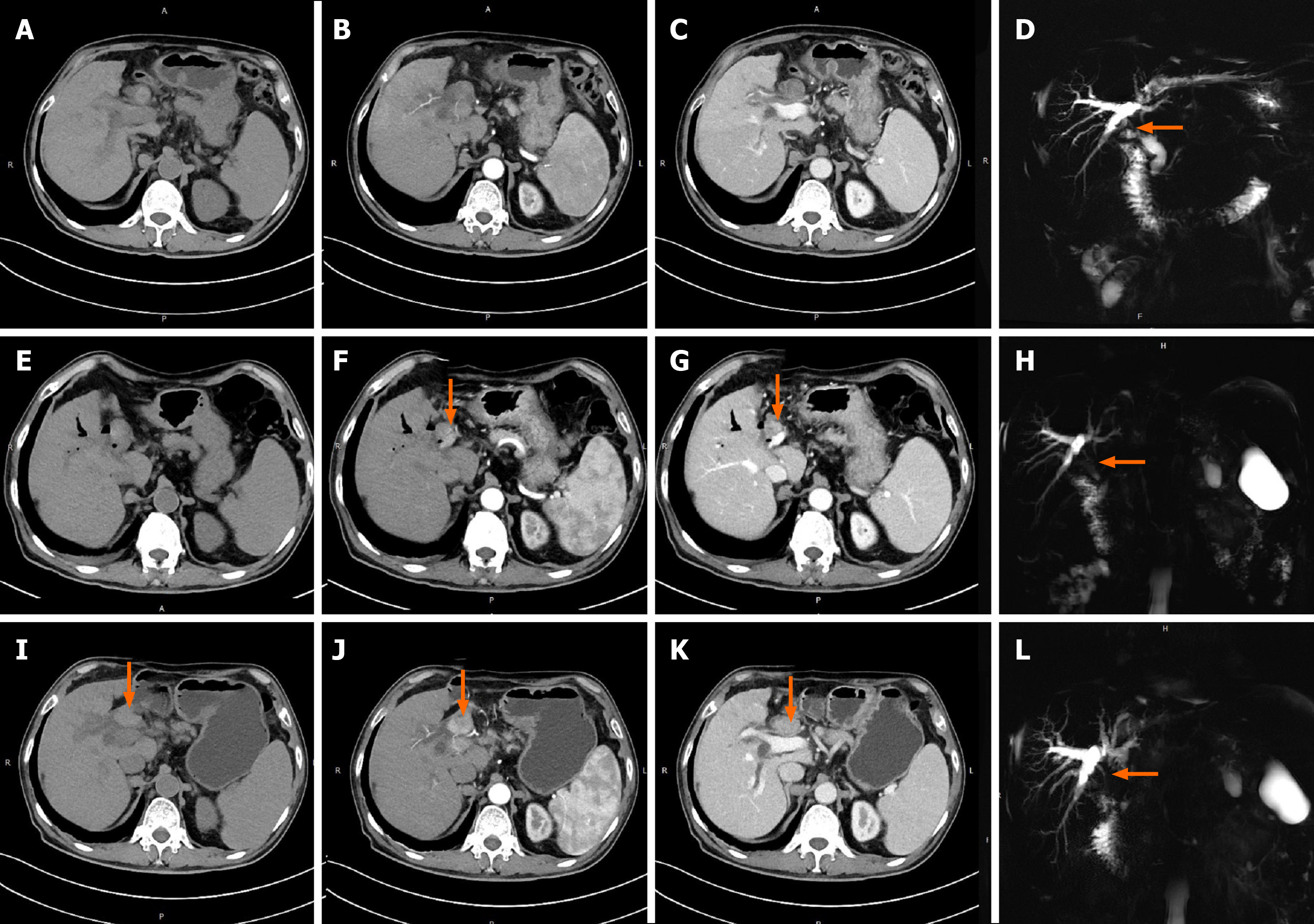
Figure 4 Computed tomography and magnetic resonance cholangiopancreatography images of patient No.
5. A-D: Computed tomography images of suspected bile duct tumor thrombus (without obvious enhancement in arterial phase) taken before it was misdiagnosed and mistreated as common bile duct stone by endoscopic retrograde cholangiopancreatography during the patient’s first admission; E-H: Computed tomography images of the bile duct tumor thrombus (green arrow) taken in outpatient follow-up 3 mo after last endoscopic retrograde cholangiopancreatography treatment; I-L: Computed tomography images of the bile duct tumor thrombus (green arrows) taken before receiving thrombus extraction during the patient’s second admission.
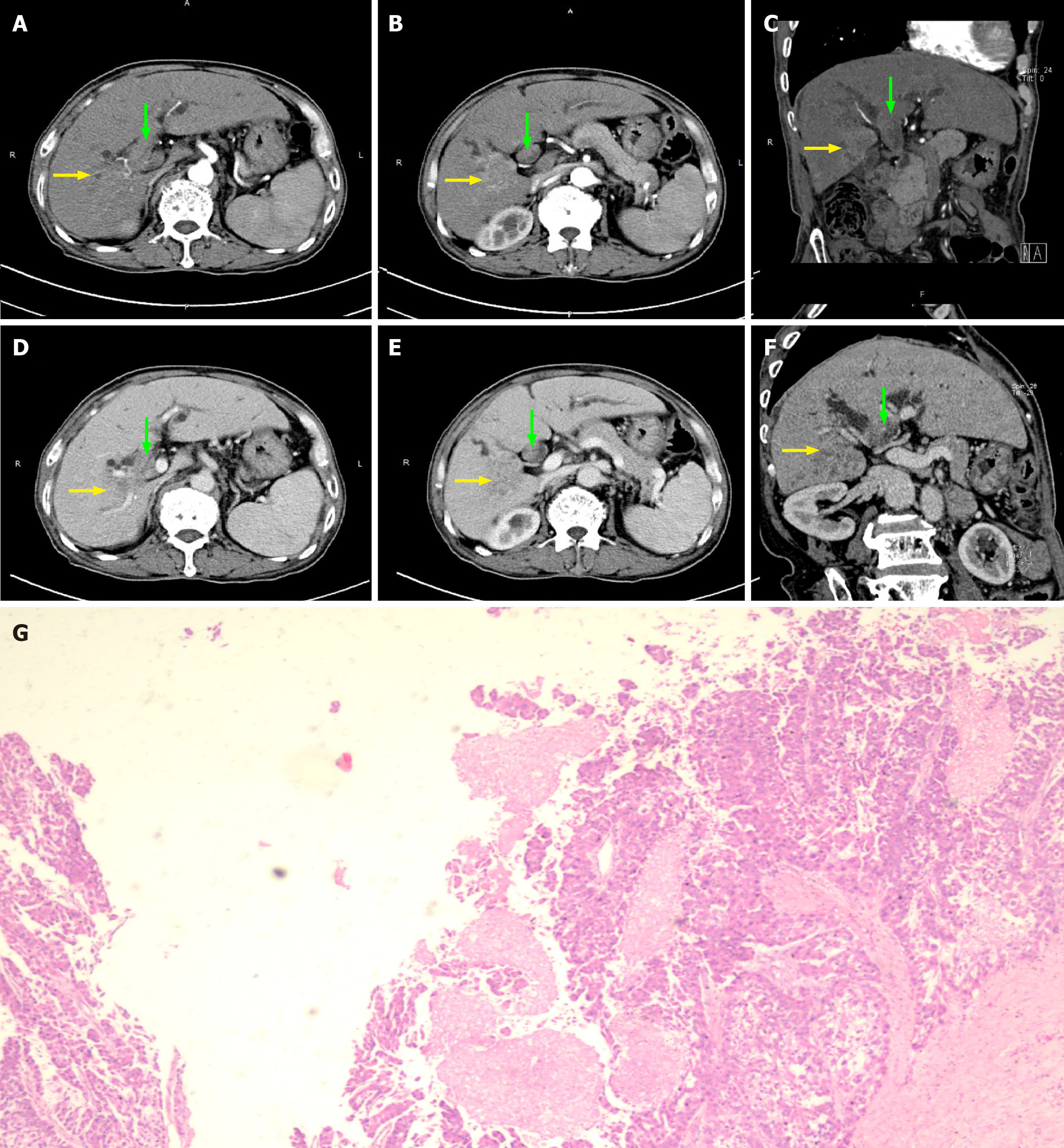
Figure 5 Computed tomography images of patient No.
4. A-F: The yellow arrows indicate hepatocellular carcinoma lesion in hepatic arterial phase (A-C) and portal-vessel phase (D-F). The green arrows indicate bile duct tumor thrombus in the common bile duct.
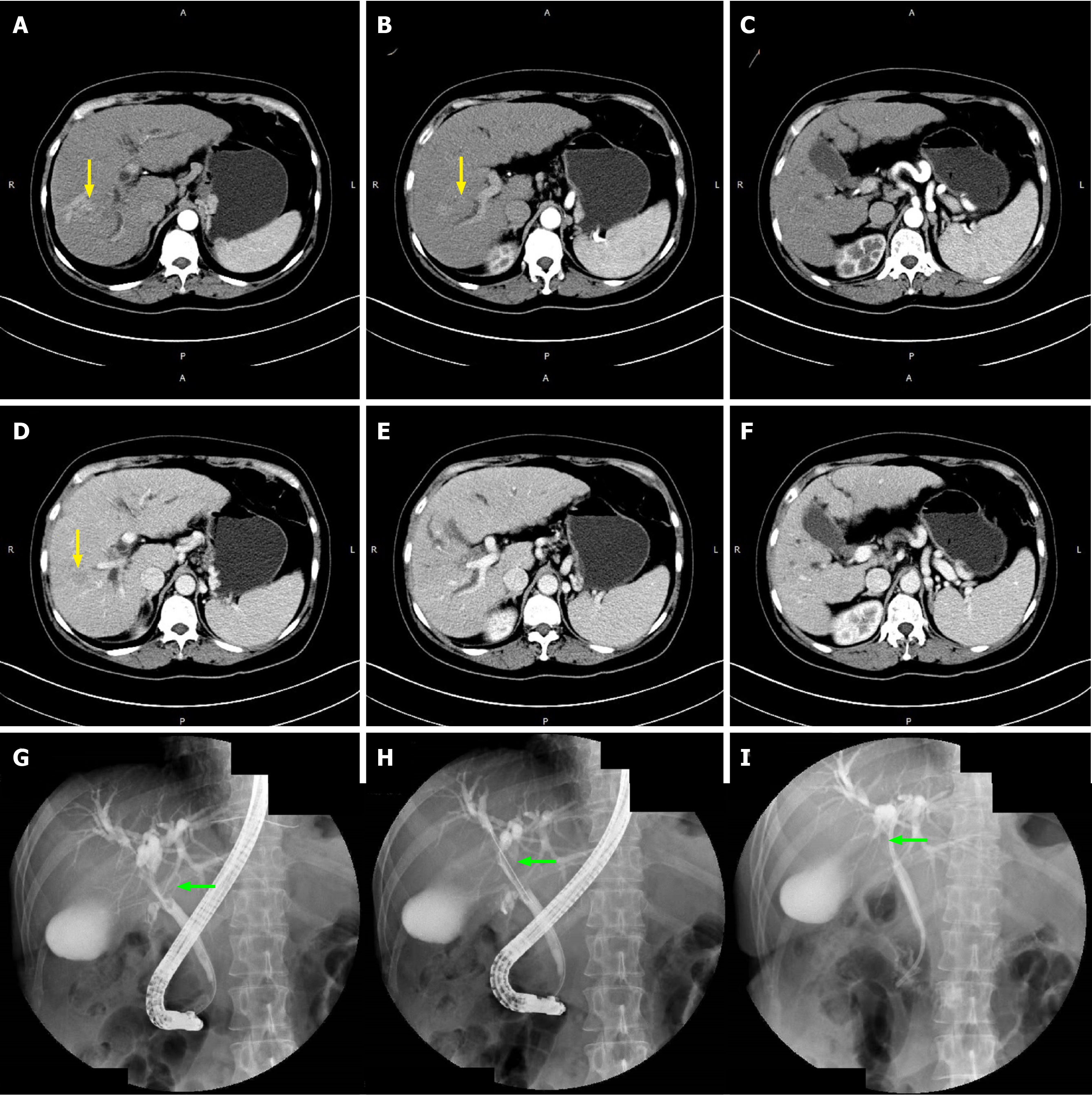
Figure 6 Computed tomography and endoscopic retrograde cholangiopancreatography images of patient No.
7. A-F: The yellow arrows indicate hepatocellular carcinoma lesions in the arterial phase (A-C) and portal-vessel phase (D-F) in computed tomography images; G-I: The green arrows indicate the location of the bile duct tumor thrombus in the common bile duct, and endoscopic nasobiliary drainage was placed through endoscopic retrograde cholangiopancreatography.
Figure 7 New proposal of classification for hepatocellular carcinoma with bile duct tumor thrombus.
Type I: Hepatocellular carcinoma (HCC) with microscopic bile duct tumor thrombus (BDTT); Type II: Resectable first-occurring or recurrent HCC mass in the liver with BDTT; Type III: BDTT without obvious HCC mass in the liver; Type IV: BDTT accompanied with unresectable intra- or extrahepatic HCC lesions. BDTT can be further divided into two subtypes according to whether tumor cells of thrombus invades into the extrahepatic bile duct wall (subtype a) or not (subtype b). BDTT: Bile duct tumor thrombus.
- Citation: Zhou D, Hu GF, Gao WC, Zhang XY, Guan WB, Wang JD, Ma F. Hepatocellular carcinoma with tumor thrombus in bile duct: A proposal of new classification according to resectability of primary lesion. World J Gastroenterol 2020; 26(44): 7005-7021
- URL: https://www.wjgnet.com/1007-9327/full/v26/i44/7005.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i44.7005