Copyright
©The Author(s) 2019.
World J Gastroenterol. Jan 28, 2019; 25(4): 469-484
Published online Jan 28, 2019. doi: 10.3748/wjg.v25.i4.469
Published online Jan 28, 2019. doi: 10.3748/wjg.v25.i4.469
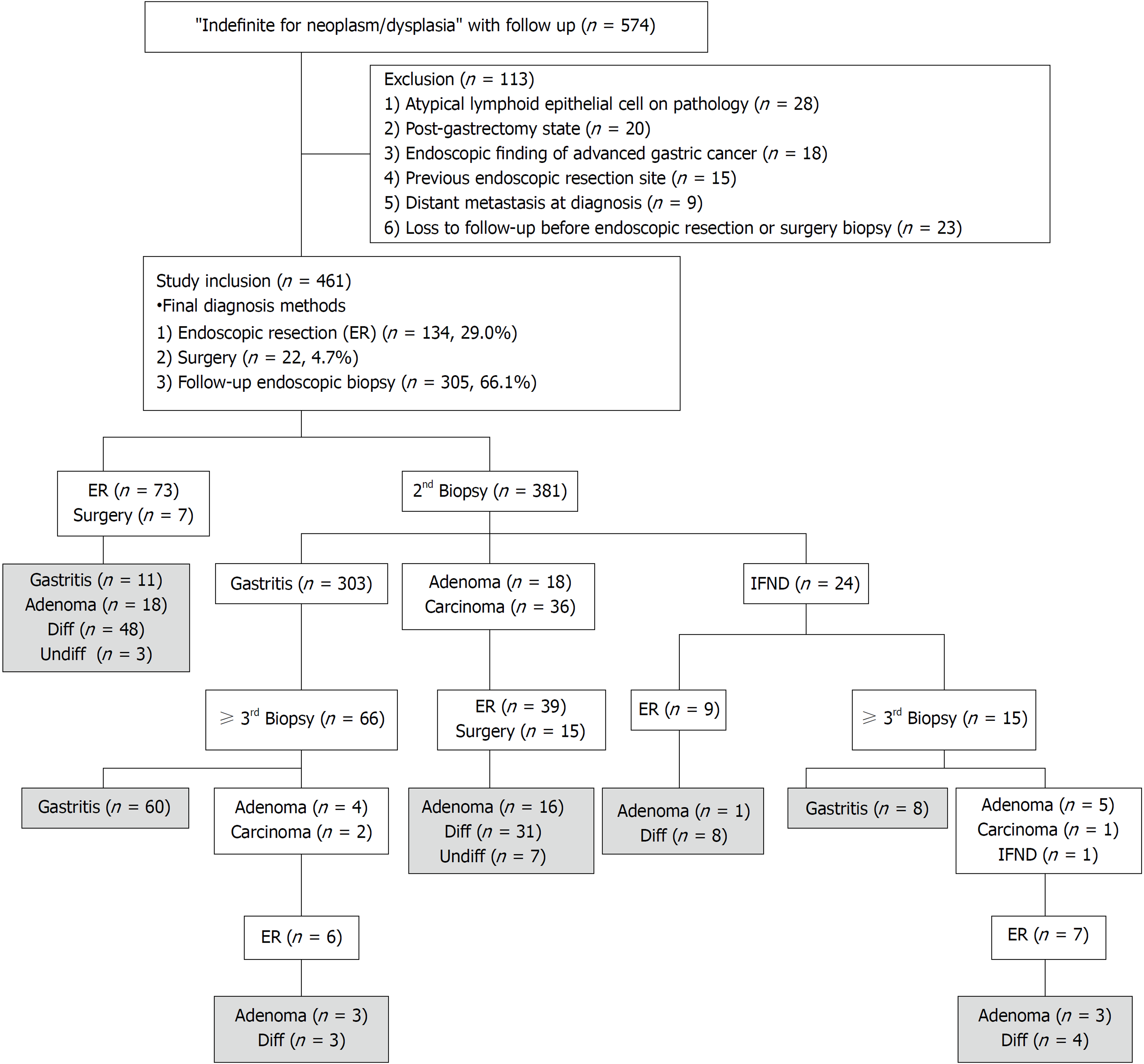
Figure 1 Flow chart of study inclusion and exclusion, and enrollment of 461 lesions with ‘indefinite for neoplasm/dysplasia’ status.
The final diagnoses are shown in the gray boxes. IFND: Indefinite for neoplasm/dysplasia; ER: Endoscopic resection; Diff: Differentiated carcinoma; Undiff: Undifferentiated carcinoma.
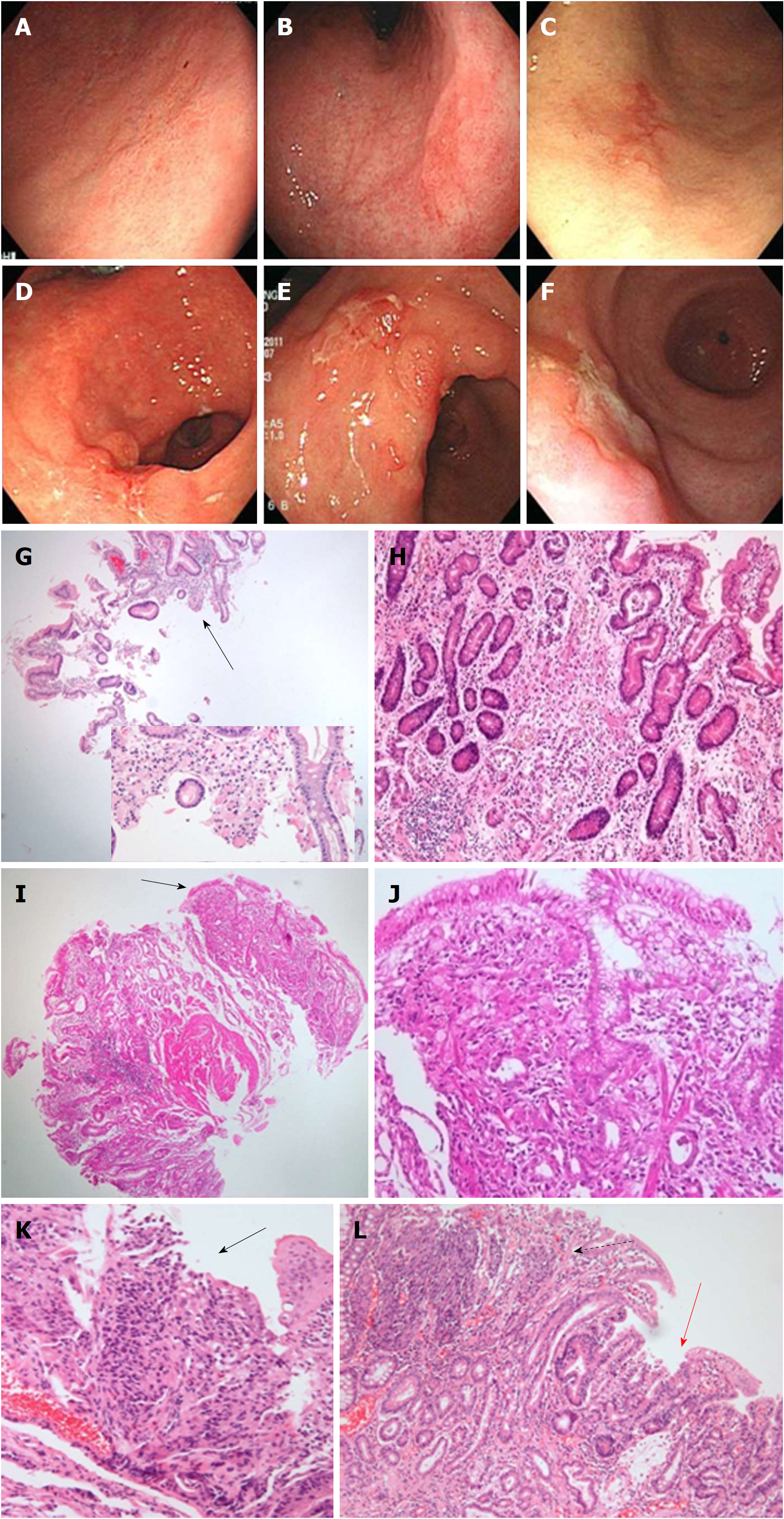
Figure 2 Representative cases of undifferentiated carcinoma.
Flat lesions with color change (A-C) and fold change with ulcerations (D-F) are shown at endoscopy. G: The case in panel A shows a few tumor cells (magnified in the inlet) in the endoscopic biopsy specimen (black arrow). H: The resected specimen shows poorly differentiated tubular adenocarcinoma with a very small tumor size (0.7 cm × 0.6 cm). I: The case in panel B shows a few tumor cells in the endoscopic biopsy specimen (black arrow). J: The resected specimen shows mixed signet ring cell carcinoma and poorly differentiated tubular adenocarcinoma with a very small tumor size (0.6 cm × 0.4 cm). K: The case in panel e shows a few tumor cells as squeezing artifact-like clusters in the endoscopic biopsy specimen (black arrow). L: The resected specimen shows mixed poorly differentiated (dotted arrow) and well-differentiated (red arrow) tubular adenocarcinoma.
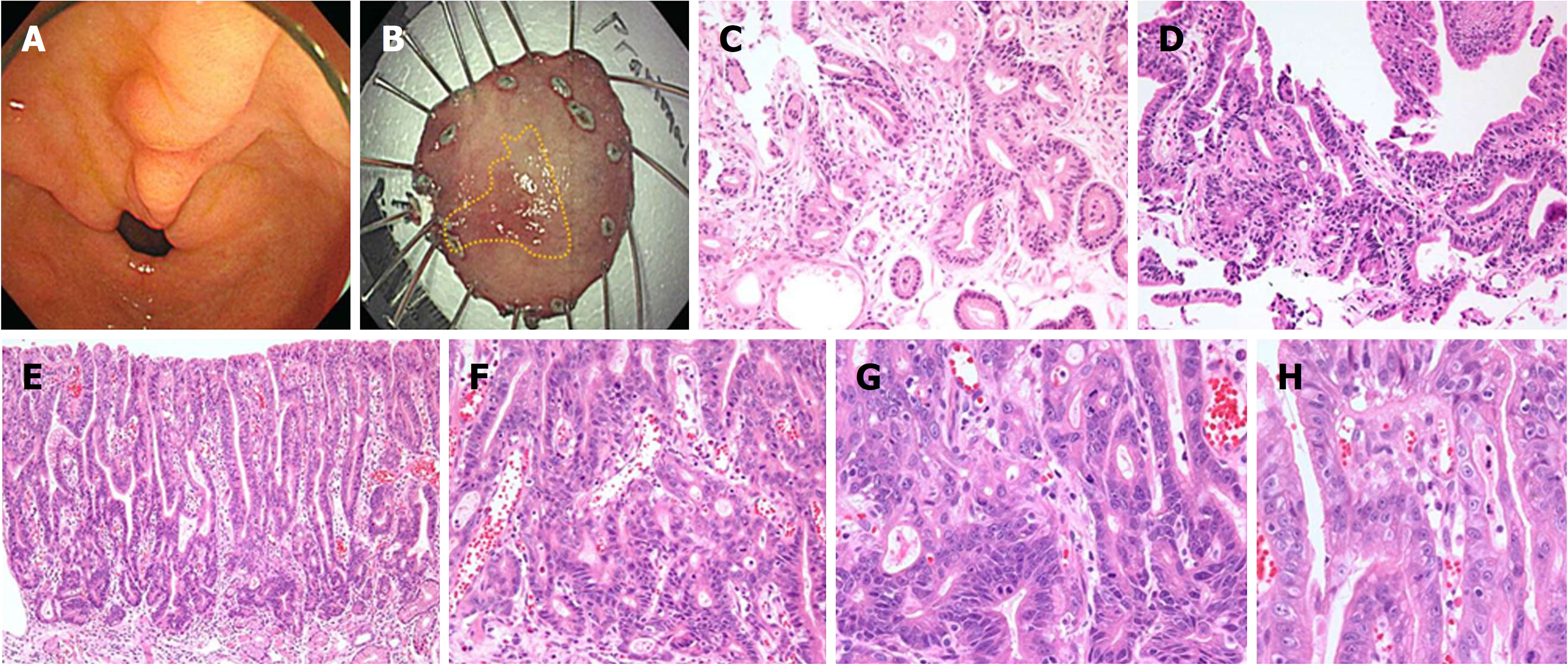
Figure 3 Representative images of Indefinite for neoplasm/dysplasia lesions with repeated diagnoses (from regenerating atypia to atypical epithelium), which were finally confirmed as well-differentiated adenocarcinoma at endoscopic submucosal dissection.
A: A lesion with mucosal irregularity and hyperemia is seen on the lesser curvature side of the prepylorus (indicated by arrows). B: After endoscopic submucosal dissection, the yellow line illustrates the boundary of the lesion confirmed in the pathology, measuring 1.7 cm × 1.0 cm. C: Regenerating atypia at the initial forceps biopsy shows focal glandular crowding with a basally-located, hyperchromatic nucleus. Glandular transition to the surrounding mucosa is observed. D: Atypical epithelium at follow-up biopsy after 598 d shows more crowded and tortuous glands. A few glands showed irregular distention. However, the hyperchromatic but basally-located nuclear atypia was mild. E: Endoscopic submucosal dissection was performed 2249 d later. It revealed well-differentiated adenocarcinoma. The low-power view shows surface maturation. F: The neoplastic tubules were prominent from the mid-portion of the tubular pit to the bottom of the gland; G: They form crowded, back-to-back, branched, and tortuous glands with disordered nuclei; H: Surface atypia is less prominent and mild nuclear atypia is observed. IFND: Indefinite for neoplasm/dysplasia.
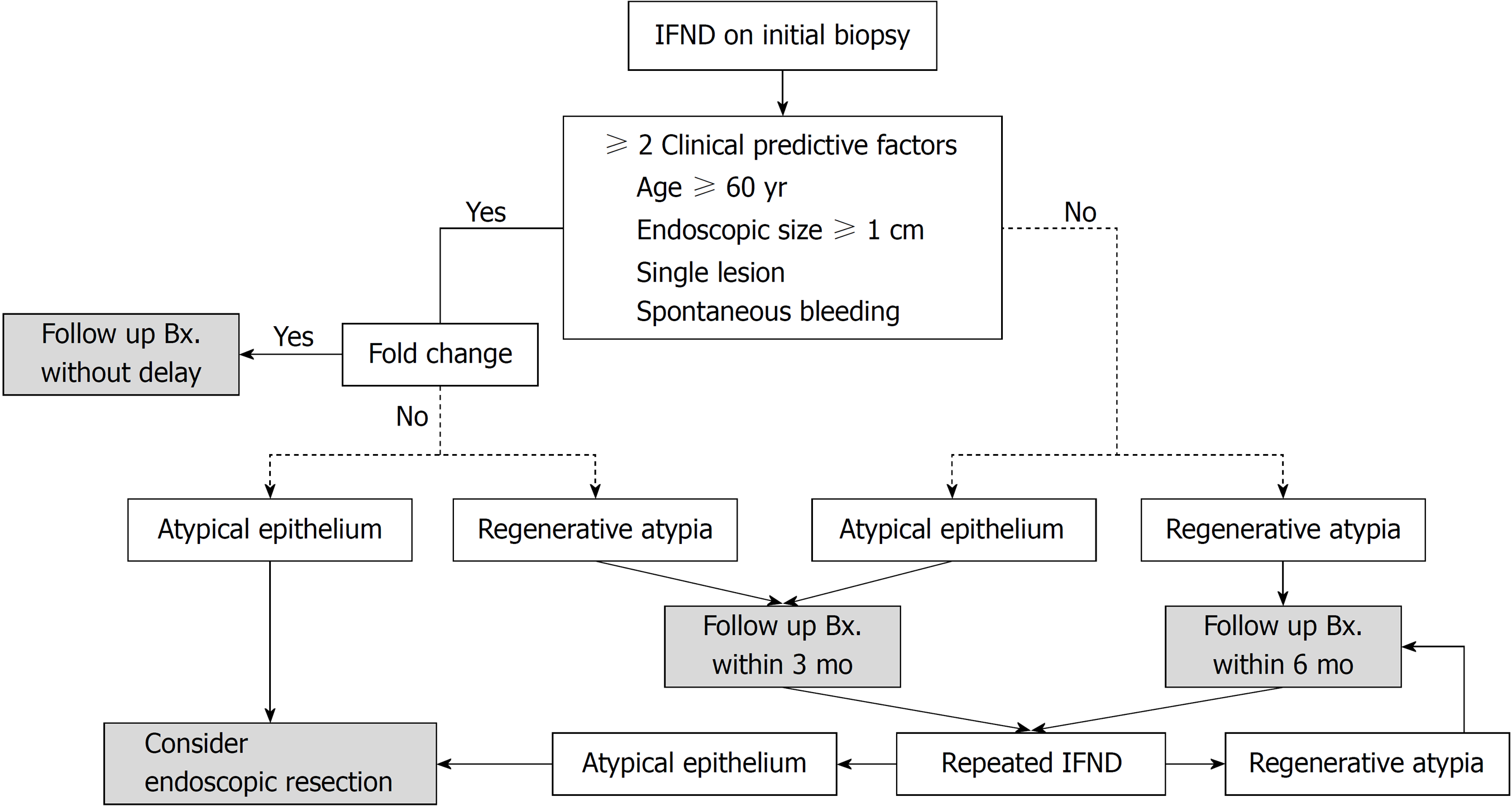
Figure 4 The guideline established in our institute for ‘indefinite for neoplasm/dysplasia’ in gastric biopsy.
Bx: Biopsy; IFND: Indefinite for neoplasm/dysplasia.
- Citation: Kwon MJ, Kang HS, Kim HT, Choo JW, Lee BH, Hong SE, Park KH, Jung DM, Lim H, Soh JS, Moon SH, Kim JH, Park HR, Min SK, Seo JW, Choe JY. Treatment for gastric ‘indefinite for neoplasm/dysplasia’ lesions based on predictive factors. World J Gastroenterol 2019; 25(4): 469-484
- URL: https://www.wjgnet.com/1007-9327/full/v25/i4/469.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i4.469