Copyright
©The Author(s) 2019.
World J Gastroenterol. Jul 21, 2019; 25(27): 3503-3526
Published online Jul 21, 2019. doi: 10.3748/wjg.v25.i27.3503
Published online Jul 21, 2019. doi: 10.3748/wjg.v25.i27.3503
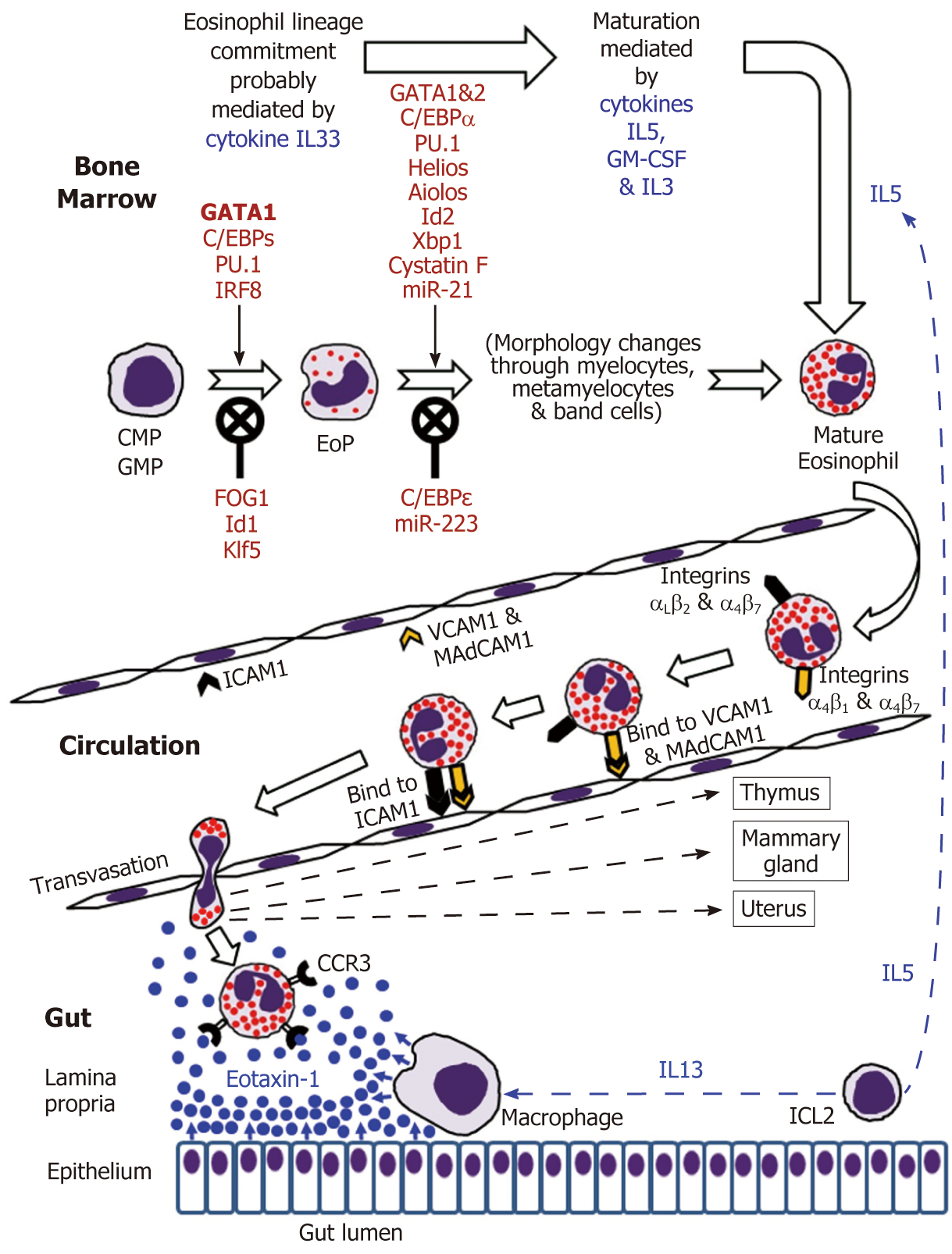
Figure 1 Eosinophil development in the bone marrow followed by mature eosinophil appearance in the circulation and eventual migration to the gut in the normal conditions.
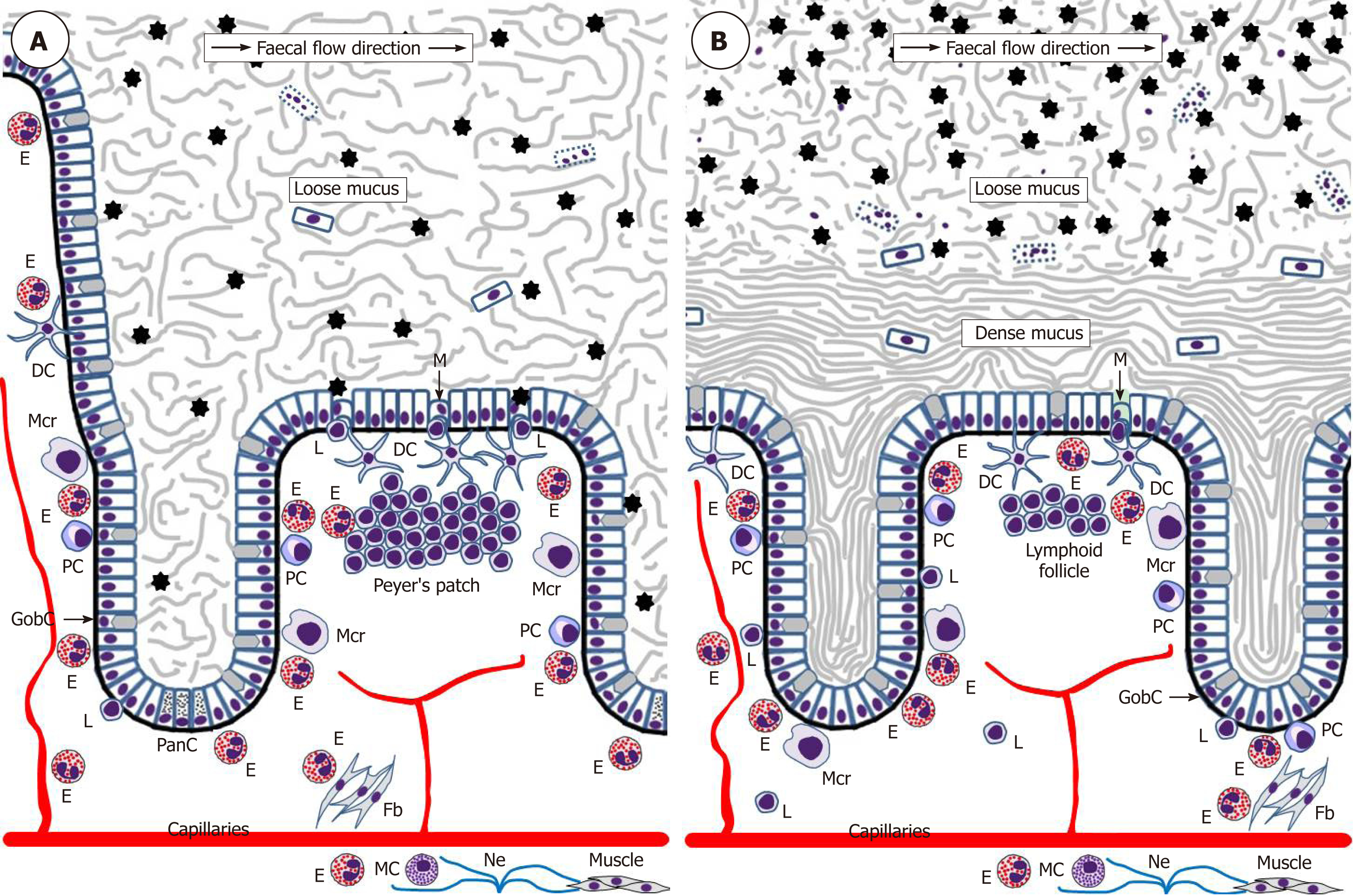
Figure 2 Schematic representation of eosinophil interactions with other cells and tissues in the small intestine (A) and colon (B).
Black asterisks indicate gut microbiota. Although one M-cell is shown in the colon, little is known about the presence of M-cells in healthy human colon.DC: Dendritic lells; E: Eosinophils; Fb: Fibroblasts; GobC: Goblet cells; L: Lymphocytes; M: M-cells; Mcr: Macrophages; Ne: Nerves; PanC: Paneth cells; PC: Plasma cells.
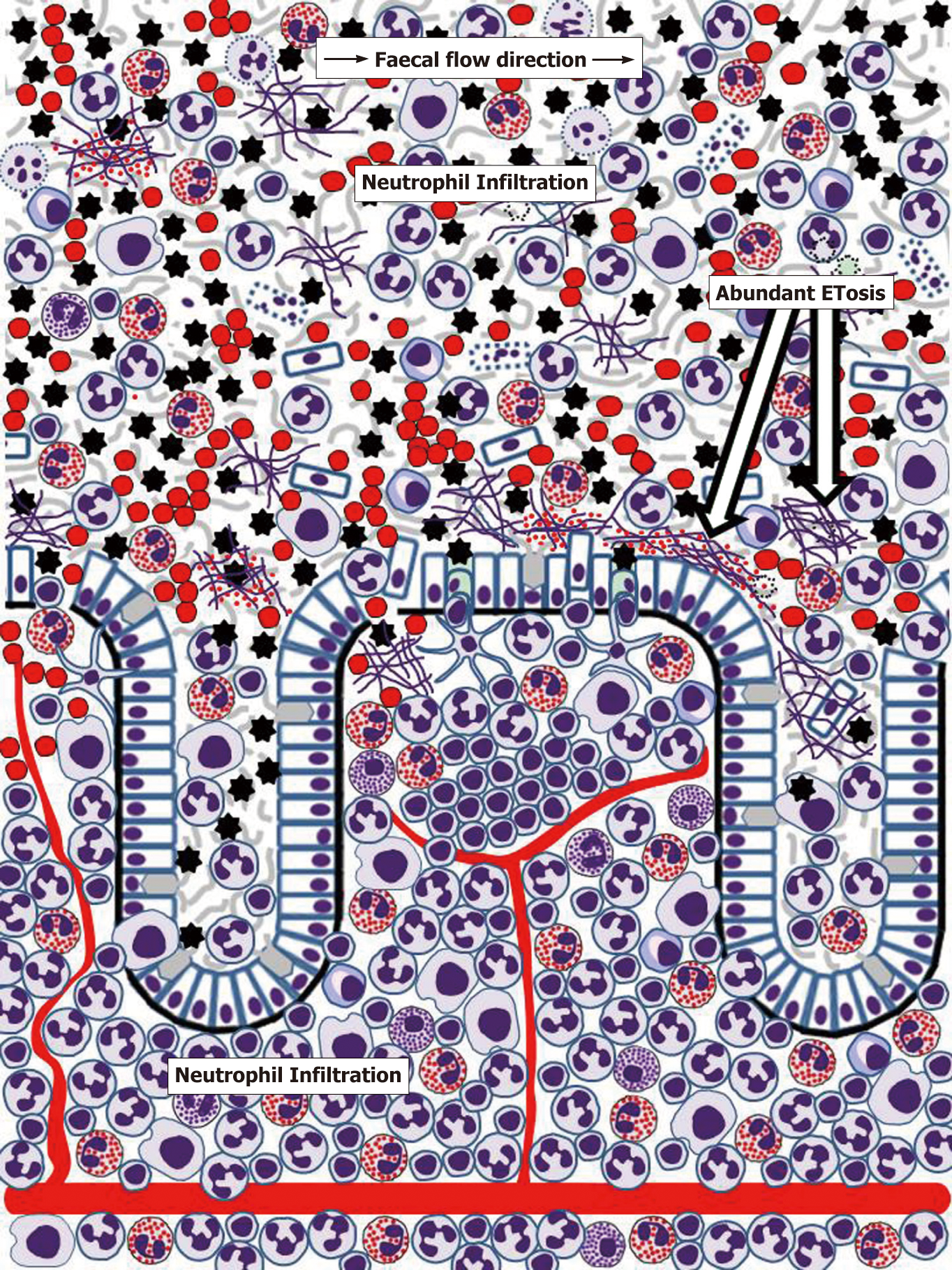
Figure 3 Schematic representation of human colonic mucosa and overlaying mucus during inflammatory bowel disease (ulcerative colitis) flare-ups.
Rapid influx of neutrophils results in severe neutrophil infiltration of the lamina propria. Further massive transepithelial migration of neutrophils and other immune cells (especially eosinophils in ulcerative colitis) eliminates mucus layer structure, enables bacterial contact with the epithelium, causes epithelial cell death, ulcer formation and bleeding. Mucus infiltration with neutrophils and eosinophils is accompanied by abundant ETosis and release of both granule proteins and free eosinophil granules. Active inflammation also induces M-cell appearance in the epithelium overlaying lymphoid follicles[171]. Cell images correspond to those used in Figure 2. Erythrocytes are presented by red circles. Small red dots correspond to free eosinophil granules.
- Citation: Loktionov A. Eosinophils in the gastrointestinal tract and their role in the pathogenesis of major colorectal disorders. World J Gastroenterol 2019; 25(27): 3503-3526
- URL: https://www.wjgnet.com/1007-9327/full/v25/i27/3503.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i27.3503