Copyright
©The Author(s) 2019.
World J Gastroenterol. Jun 14, 2019; 25(22): 2788-2798
Published online Jun 14, 2019. doi: 10.3748/wjg.v25.i22.2788
Published online Jun 14, 2019. doi: 10.3748/wjg.v25.i22.2788
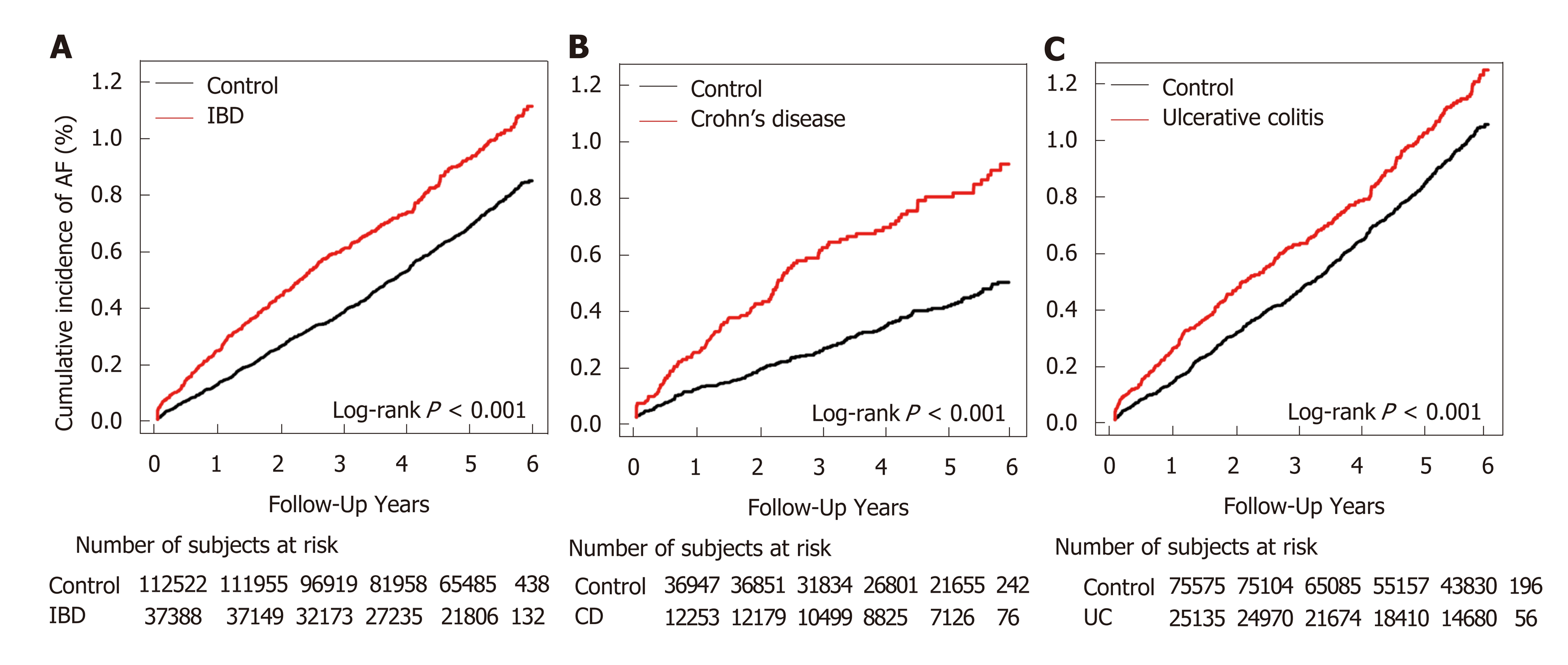
Figure 1 Kaplan–Meier survival curves for cumulative incidence of atrial fibrillation.
Cumulative incidence was defined as the probability of new-onset atrial fibrillation during follow-up. A: Comparison between inflammatory bowel disease (IBD) group and control group; B: Comparison between Crohn’s disease group and control group; C: Comparison between ulcerative colitis group and non-IBD group. CD: Crohn’s disease; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; AF: Atrial fibrillation.
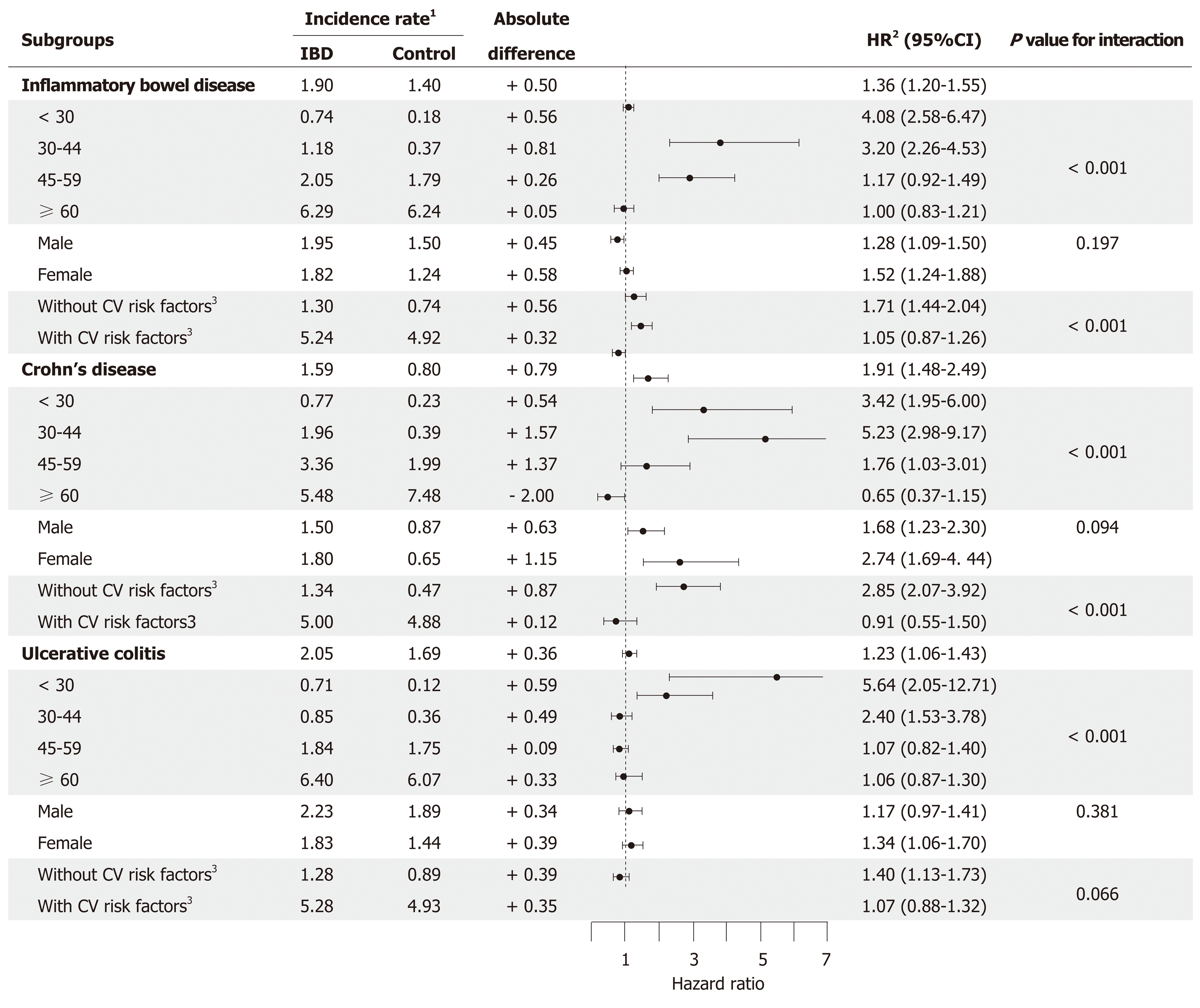
Figure 2 Subgroup analysis.
Subgroup analysis to assess the risk of atrial fibrillation in patients with inflammatory bowel disease (IBD) based on age (< 30, 30-44, 45-59, and ≥ 60 years), sex (men and women), and cardiovascular (CV) risk factors (those with and without CV risk factors). The association between IBD and the risk of development of atrial fibrillation was weaker in older individuals and in those with CV risk factors. 1Incidence rates have been calculated per 1000 patient-years; 2Adjusted for age, sex, location, income, diabetes mellitus, hypertension, dyslipidemia, stroke, myocardial infarction, venous thromboembolism, and end-stage renal disease; 3Hypertension, diabetes mellitus, or dyslipidemia. CI: Confidence interval; CV: Cardiovascular; HR: Hazard ratio; IBD: Inflammatory bowel disease.
- Citation: Choi YJ, Choi EK, Han KD, Park J, Moon I, Lee E, Choe WS, Lee SR, Cha MJ, Lim WH, Oh S. Increased risk of atrial fibrillation in patients with inflammatory bowel disease: A nationwide population-based study. World J Gastroenterol 2019; 25(22): 2788-2798
- URL: https://www.wjgnet.com/1007-9327/full/v25/i22/2788.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i22.2788