Copyright
©The Author(s) 2019.
World J Gastroenterol. May 28, 2019; 25(20): 2442-2449
Published online May 28, 2019. doi: 10.3748/wjg.v25.i20.2442
Published online May 28, 2019. doi: 10.3748/wjg.v25.i20.2442
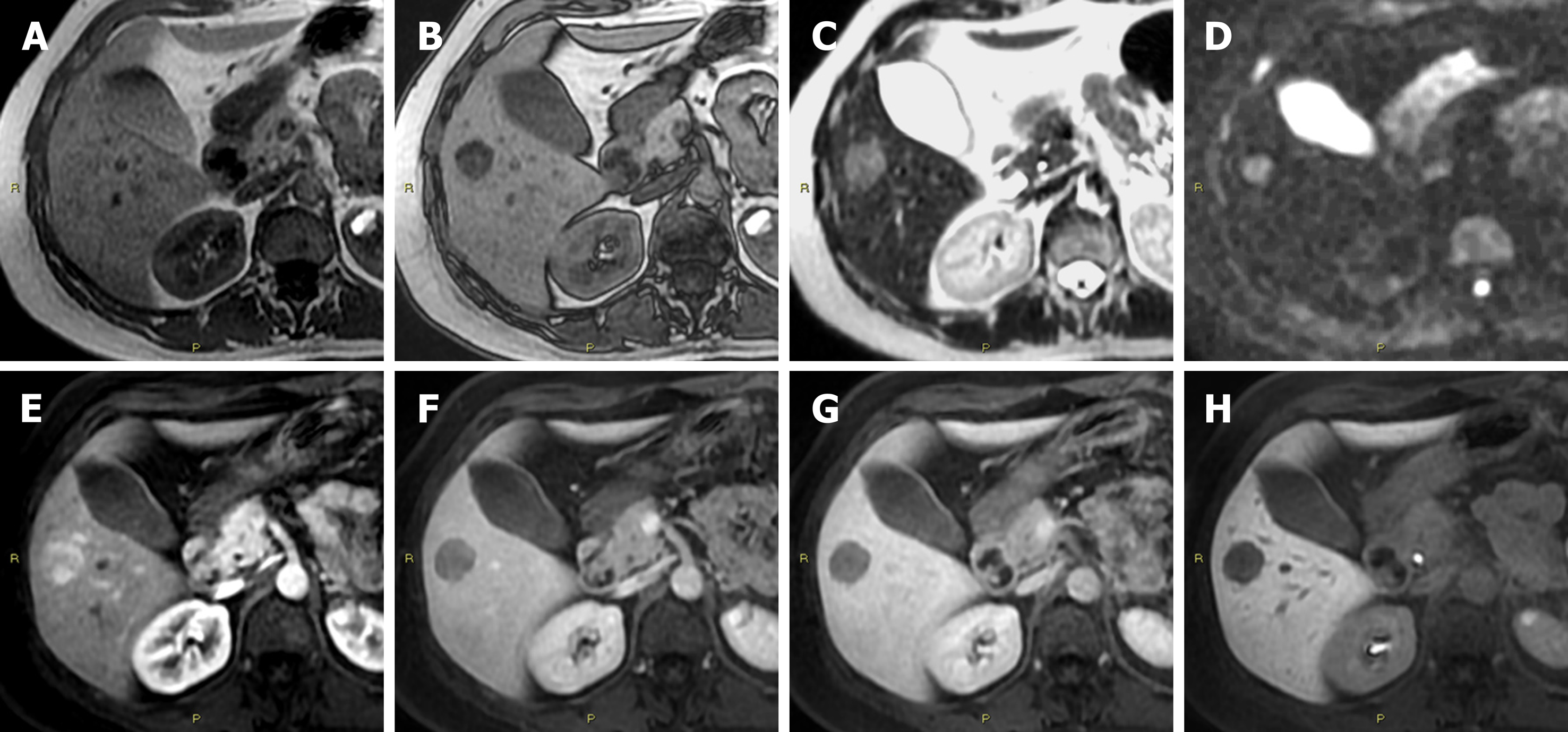
Figure 1 Diagnostic challenges in hepatocyte nuclear factor 1A mutated hepatocellular adenoma.
A: In a 51-year-old woman, the axial T1 in-phase image shows an isointense lesion in liver segment V; B: With signal dropout in the T1 out-of-phase image; C: Slightly hyperintense in the T2-weighted; D: In diffusion-weighted; E: In the arterial phase images; F: Washout of the contrast media in the portal-venous phase; G: In the delayed phase images; H: Hypointense in the hepatobiliary phase image. According to the current guidelines, this lesion is suggestive for a hepatocellular adenoma inactivated for HNF-1α. However, according to the newer proposed classification of hepatocellular adenoma, it is not possible to exclude an inflammatory hepatocellular adenoma containing fat and, as consequence, even a mixed form of β-catenin activated-inflammatory hepatocellular adenoma, on imaging.
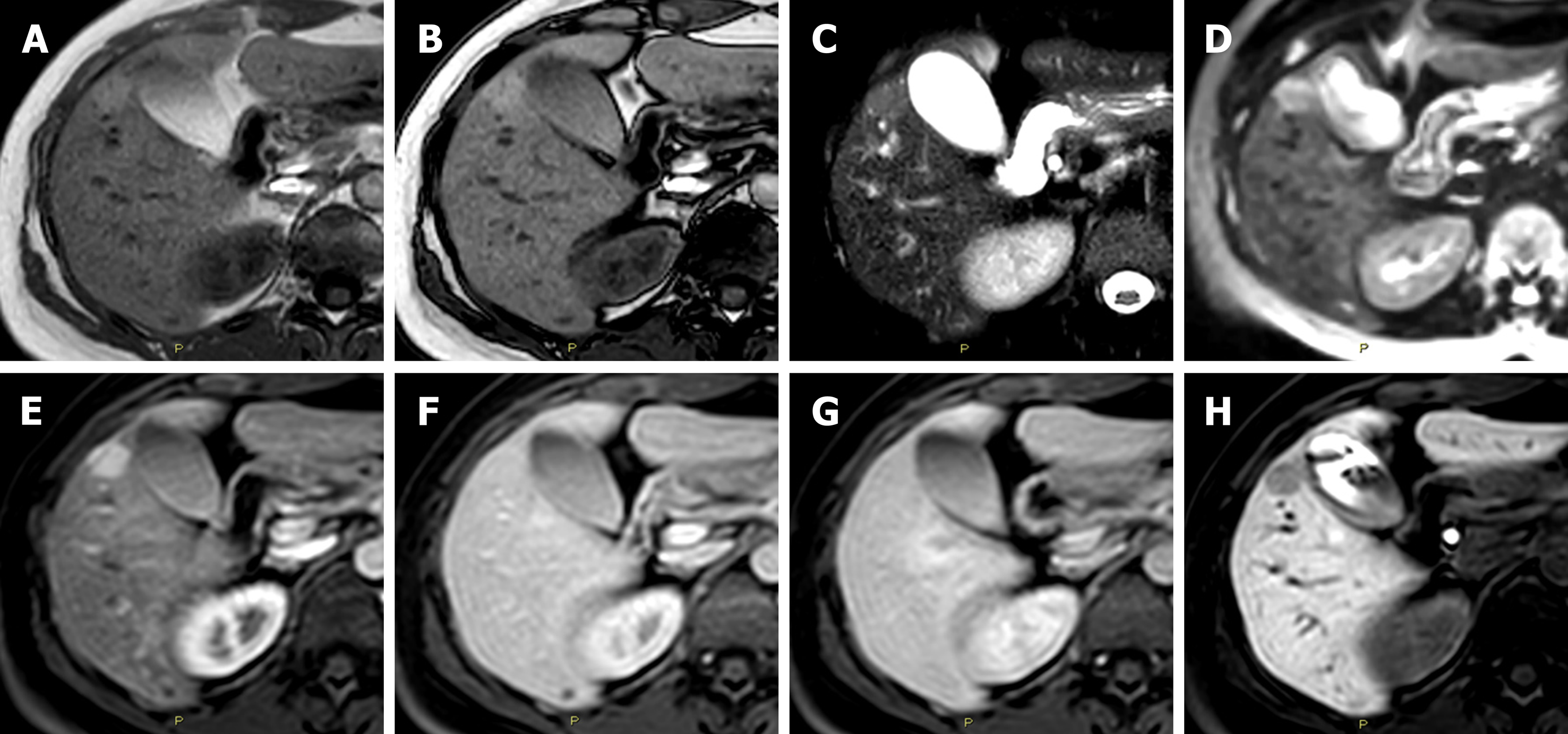
Figure 2 Diagnostic challenges in the imaging classification of hepatocellular adenoma.
A: In a 47-year-old woman the axial T1 in-phase; B: Out-of-phase images show an isointense lesion in liver segment V; C: Hyperintense in the T2-weighted; D: In the diffusion-weighted; E: In the arterial phase images; F: Without washout of the contrast media in the portal-venous phase; G: In the delayed phase images; H: Hypointense in the hepatobiliary phase image. According to the current guidelines, this lesion is suggestive for an inflammatory hepatocellular adenoma. However, it is not possible to exclude a mixed form of β-catenin activated-inflammatory hepatocellular adenoma or even a hepatocellular adenoma inactivated for HNF-1α without fatty component.
- Citation: Renzulli M, Clemente A, Tovoli F, Cappabianca S, Bolondi L, Golfieri R. Hepatocellular adenoma: An unsolved diagnostic enigma. World J Gastroenterol 2019; 25(20): 2442-2449
- URL: https://www.wjgnet.com/1007-9327/full/v25/i20/2442.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i20.2442