Copyright
©The Author(s) 2019.
World J Gastroenterol. Apr 7, 2019; 25(13): 1531-1549
Published online Apr 7, 2019. doi: 10.3748/wjg.v25.i13.1531
Published online Apr 7, 2019. doi: 10.3748/wjg.v25.i13.1531
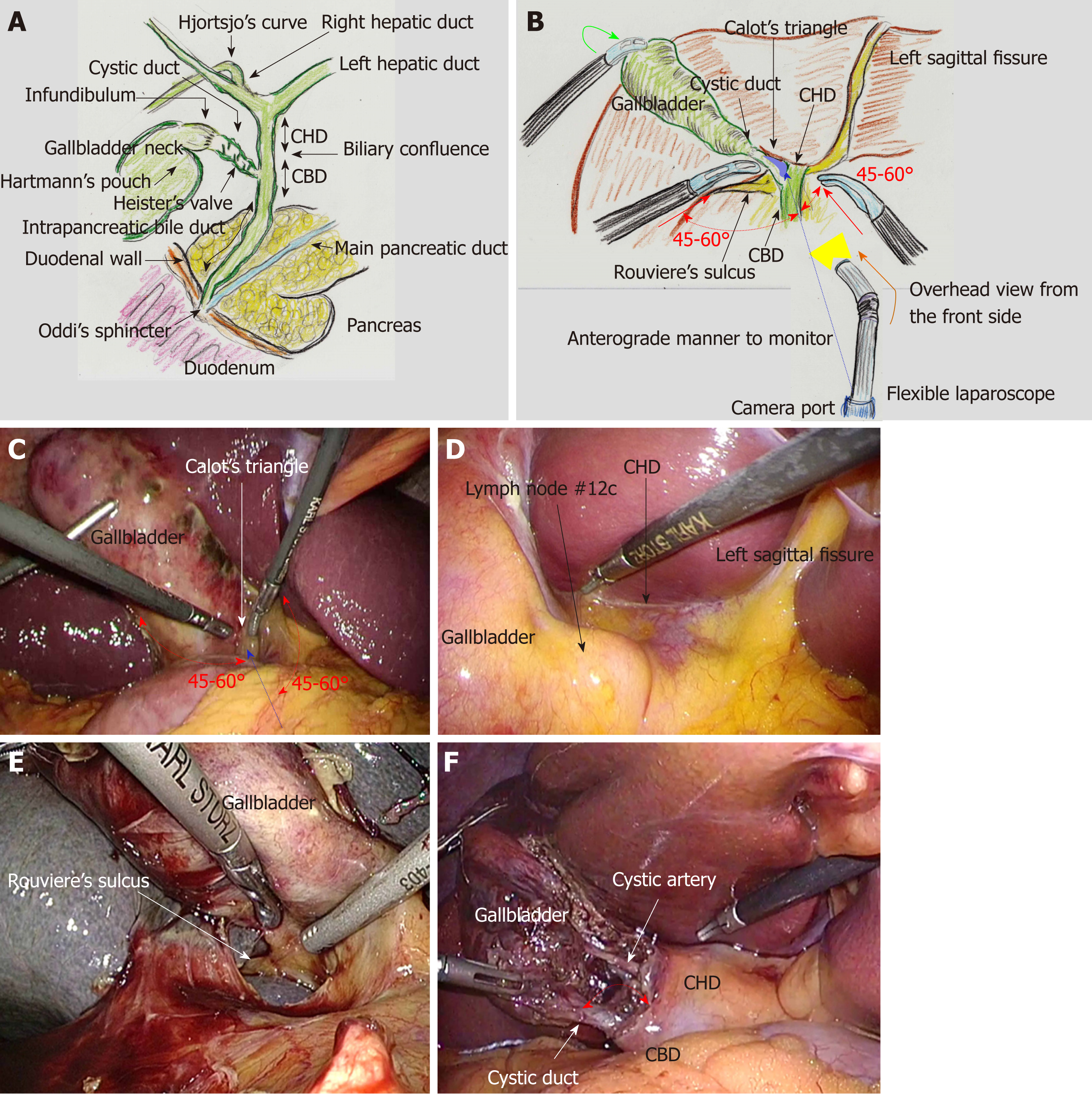
Figure 1 Biliary system and actual surgical procedures of laparoscopic choledocholithotomy.
A: The common hepatic duct (CHD), common bile duct (CBD) and intra-pancreatic bile duct compose the extrahepatic bile duct. Biliary drainage is regulated by Oddi’s sphincter. Recognition of Hjortsjo’s curve on cholangiography is useful for detecting the posterior branch from the right hepatic duct; B and C: The gallbladder fundus is superiorly and cranially lifted (green arrow). The target site is Calot’s triangle (blue shaded area). The two forceps of the main surgeon (red arrow) form appropriate angles (approximately 45°-60°) (red dotted arrow) to the axis from the camera port to Calot’s triangle (blue dotted arrow). A flexible laparoscope provides an overhead view from the upper anterior side (orange arrow), anterograde to the visual monitor; D: The bottom plateau of the U-shaped line from the left sagittal fissure to the gallbladder, which necessarily involves the CHD; E: Rouviere’s sulcus always involves the right hepatic duct; F: The whiter color change of the cystic duct is recognized, and a wider angle is created between the cystic duct and CHD (red arrow). CHD: Common hepatic duct; CBD: Common bile duct.
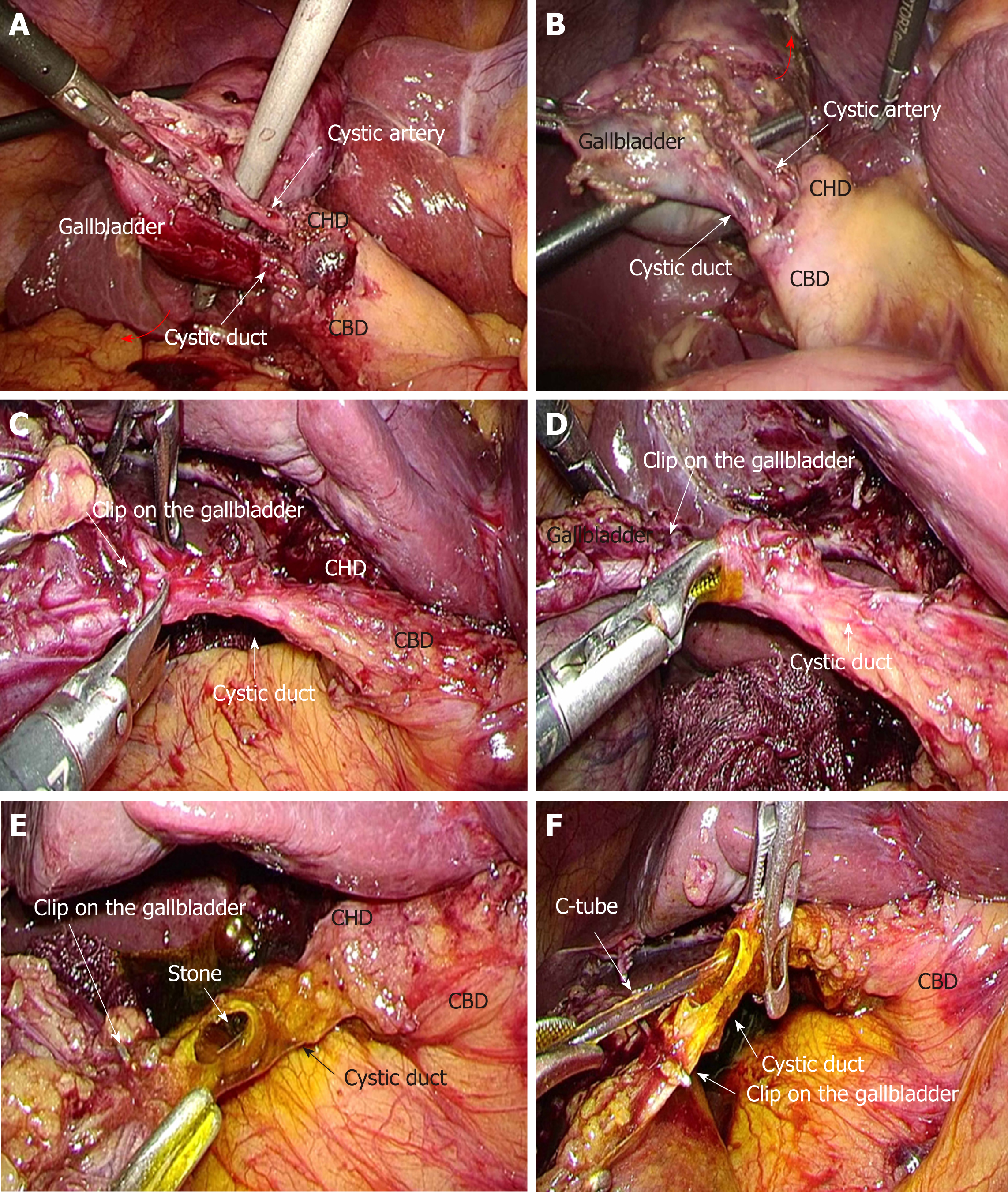
Figure 2 Actual surgical procedures of laparoscopic choledocholithotomy.
A and B: Critical view of safety is established in the anterior (A, arrow) and posterior (B, arrow) aspects; C: A semi-circular incision is made in the cystic duct; D: Heister’s valves are carefully destroyed; E: Stones in the cystic duct are removed; F: The golden-brown bile flows from the extrahepatic bile duct. The C-tube is cannulated. CHD: Common hepatic duct; CBD: Common bile duct.
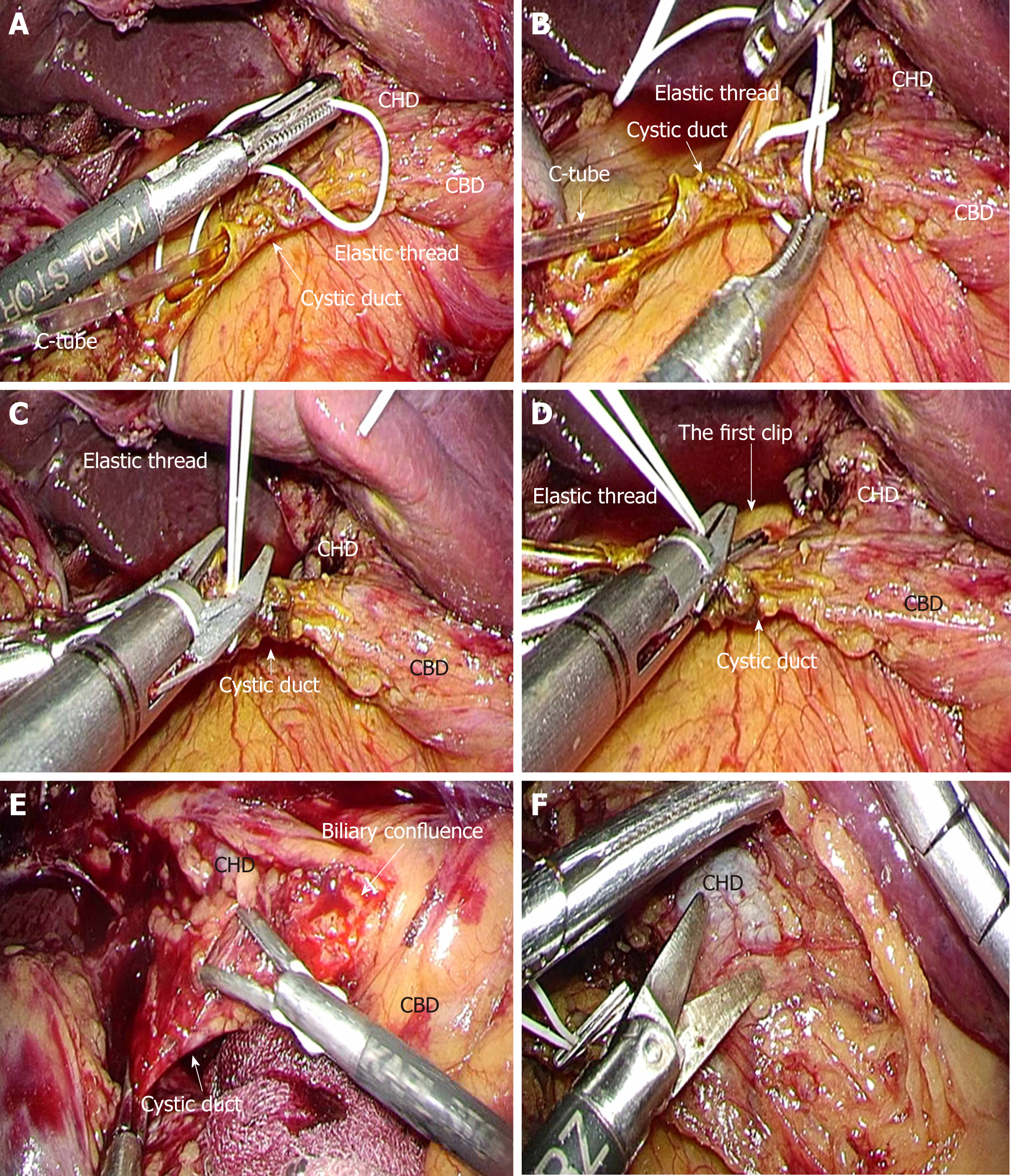
Figure 3 Actual surgical procedures of laparoscopic choledocholithotomy.
A-C: Optimal transcystic fixation of C-tube is completed with elastic suture and clips. The elastic suture is never ligated directly; D: The second clip prevents any slippage of the first clip; E: The common hepatic duct, biliary confluence and common bile duct are intentionally explored; F: Feeding and drainage vessels surrounding the extrahepatic bile duct should be preserved. CHD: Common hepatic duct; CBD: Common bile duct.
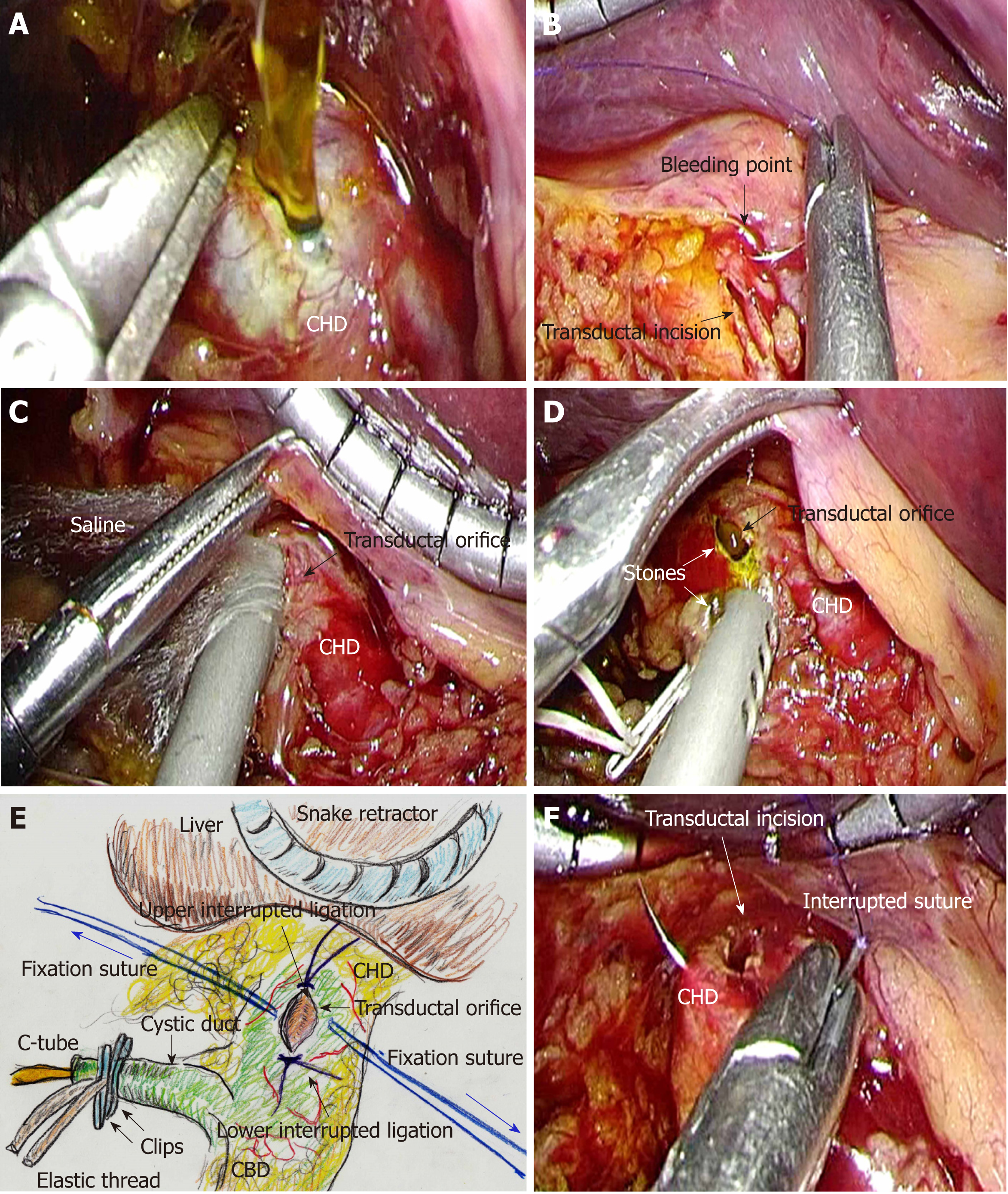
Figure 4 Actual surgical procedures of laparoscopic choledocholithotomy.
A: The extrahepatic bile duct (EHBD) is opened with sharp dissection; B: Intracorporeal suture placement and subsequent ligation are the first choice for hemostasis. No energy devices should be used; C: The cavity of the EHBD is sufficiently flushed. Frequent continuous suction is needed during laparoscopic choledocholithotomy. An automatically maintained pneumoperitoneum system is used to preserve an adequate surgical field; D: All stones are removed; E: Interrupted sutures are placed and subsequently ligated at the upper and lower edges of the transductal orifice to prevent progressive laceration resulting from cholangioscopic maneuvers. Thereafter, fixation sutures (blue arrows) are bilaterally placed to open the transductal orifice. These fixation sutures are adequately set through the abdominal wall at different points from the laparoscopic trocars; F: Interrupted sutures and subsequent ligation are placed at the upper and lower edges of the transductal incision, to prevent progressive laceration due to cholangioscopic maneuvers. CHD: Common hepatic duct; CBD: Common bile duct; EHBD: Extrahepatic bile duct.
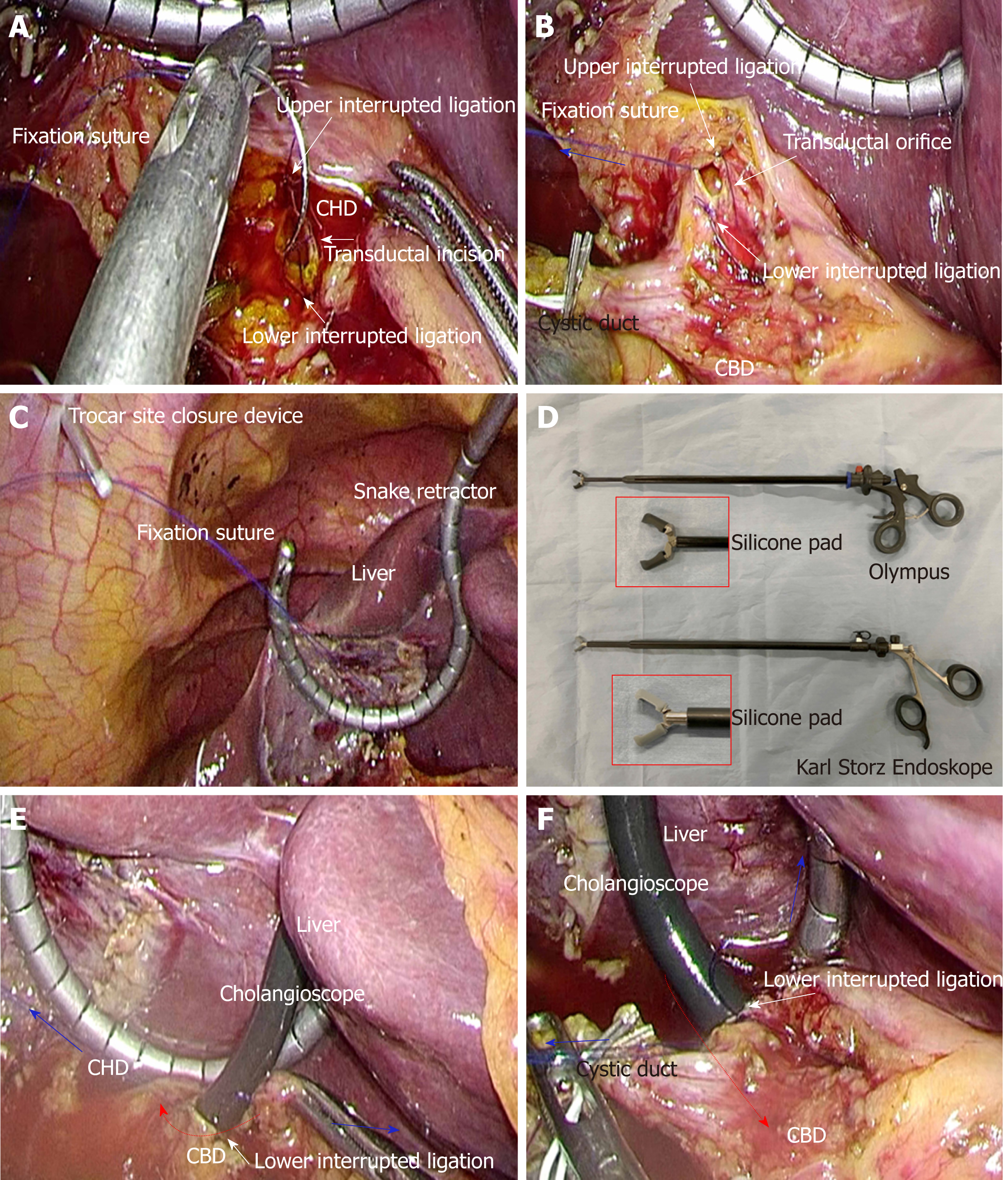
Figure 5 Actual surgical procedures of laparoscopic choledocholithotomy.
A and B: Fixation sutures (blue arrow) are bilaterally placed to open the transductal orifice; C: Fixation sutures are adequately set through the abdominal wall at different points from the laparoscopic trocars with a trocar site closure device. The liver is held cranially with a snake retractor to stretch the hepatoduodenal ligament; D: A dedicated elastic forceps is important for successful laparoscopic choledocholithotomy. The tip of the forceps contains a silicone pad to avoid damaging the cholangioscope. Olympus (A66070A; Tokyo, Japan) and Karl Storz Endoskope (K33531 PG; Tuttlingen, Germany) provide made-to-order forceps, respectively; E and F: The bifurcation of hepatic ducts on the common hepatic duct side (E) and characteristic findings of the end of the intra-pancreatic bile duct on the common bile duct side (F) should be confirmed. Interrupted ligations at the upper and lower edges of the transductal incision prevent progressive laceration during cholangioscope maneuvers (red arrows). Fixation sutures (blue arrows) are removed. CHD: Common hepatic duct; CBD: Common bile duct.
Figure 6 Laparoscopic choledocholithotomy.
A: Generally, both the transductal incision and subsequent primary closure are made in the same direction along the long axis; B: In ducts with diameter smaller than 7-8 mm, primary closure is performed in the direction of the short axis to avoid postoperative stenosis; C and D: Though severe adhesions and dense tissue are often intractable during reoperative surgery, a laparoscopic approach is safe and feasible for choledocholithotomy; E and F: A transductal incision (blue arrow) is made along the long axis, and full-layer interrupted sutures are placed at the upper and lower edges of the transductal incision to avoid severe laceration of the extrahepatic bile duct during cholangioscope maneuvers. CHD: Common hepatic duct; CBD: Common bile duct.
- Citation: Hori T. Comprehensive and innovative techniques for laparoscopic choledocholithotomy: A surgical guide to successfully accomplish this advanced manipulation. World J Gastroenterol 2019; 25(13): 1531-1549
- URL: https://www.wjgnet.com/1007-9327/full/v25/i13/1531.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i13.1531