Copyright
©The Author(s) 2017.
World J Gastroenterol. Jun 7, 2017; 23(21): 3934-3944
Published online Jun 7, 2017. doi: 10.3748/wjg.v23.i21.3934
Published online Jun 7, 2017. doi: 10.3748/wjg.v23.i21.3934
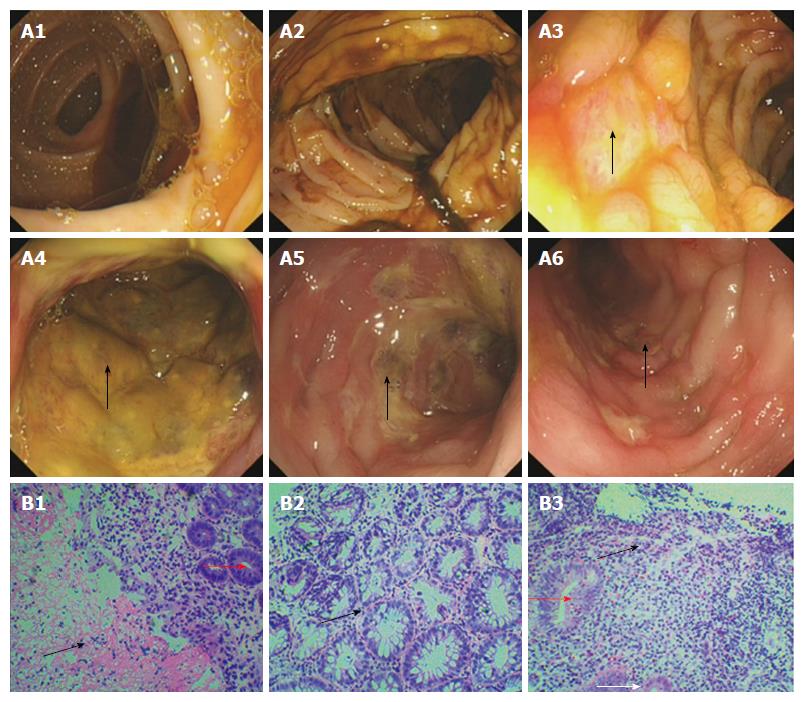
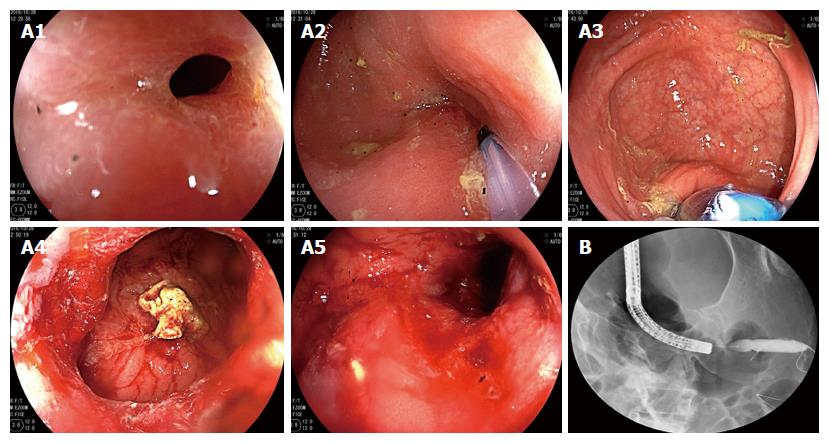
Figure 1 Colonoscopy and biopsy 14 mo ago.
Electronic colonoscopy performed 14 mo prior to the ultimate hospital admission revealed smooth mucosa of the ileocecal junction and ascending colon (A1 and A2), nodular mucosal elevations in the transverse colon and descending colon (arrows, A3 and A4), severe mucosal congestion, erosion, and ulcer in the sigmoid colon (arrow, A5), and mild mucosal congestion, erosion and ulcer in the rectum (arrow, A6). Pathological analysis revealed chronic inflammation associated with necrosis (black arrow head, B1) and branching crypts (black arrow head, B2) in the mucosa of the sigmoid colon, as well as chronic mucosal inflammation and cryptitis (red arrow heads, B1 and B3)/eosinophil infiltration (black arrow head, B3) in the transverse colon. Hematoxylin and eosin staining; magnification of × 100 for B1 and B3, and × 200 for B2.
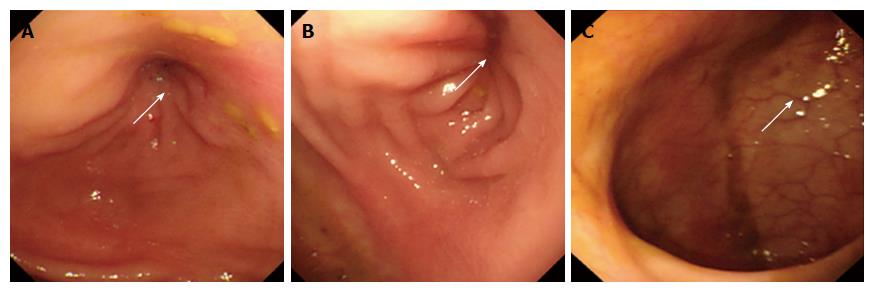
Figure 2 Colonoscopy 4 mo ago.
Electronic colonoscopy performed 4 mo prior to the ultimate hospital admission revealed stenosis of the sigmoid colon, with a diameter of about 0.5 cm (arrows, A and B). The colonoscope could not pass through the stenotic segment. The rectal mucosa was smooth, with clear vascular texture (arrow, C).
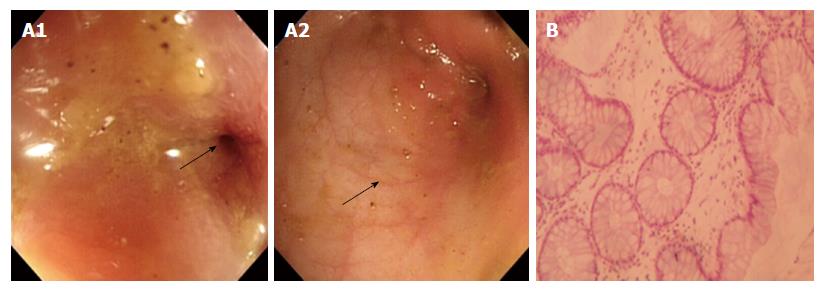
Figure 3 Colonoscopy and biopsy 3 mo ago.
Electronic colonoscopy performed 3 mo prior to the ultimate hospital admission revealed stenosis of the sigmoid colon (arrow, A1), with a diameter of 4-5 mm at the site of stenosis. The mucosa was smooth with clear vascular texture (arrow, A2). Pathological analysis of the biopsied tissue revealed mild crypt distortion and stroma edema (B). Hematoxylin and eosin staining; magnification of × 200 for B.
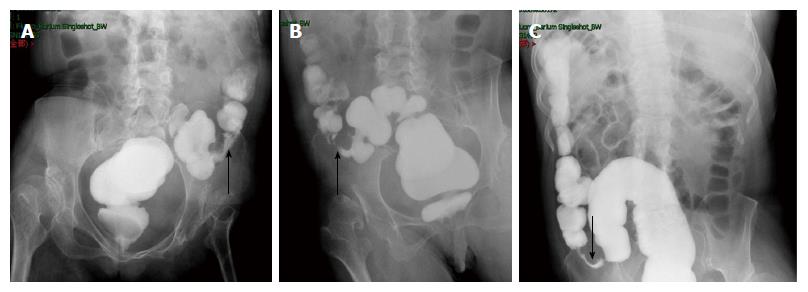
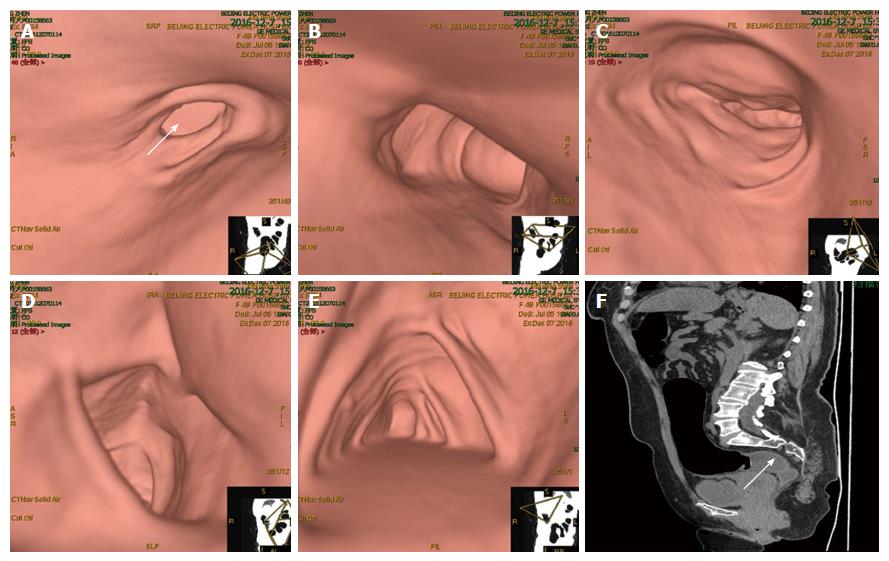
Figure 4 Colonography.
Electronic colonoscopy performed 3 mo prior to the ultimate hospital admission revealed stenosis at the junction between the descending colon and sigmoid colon, with the narrowest diameter measuring about 0.5 cm (A, supine position; B, prone position). The stenotic segment was about 4.3 cm long (arrow, C).
Figure 5 Colonoscopic balloon dilatation 3 mo ago.
The patient underwent X-ray-guided colonoscopic balloon dilatation at 3 mo prior to the ultimate hospital admission. Electronic colonoscopy revealed stenosis of the sigmoid colon (A1). A guide wire was inserted through the stenotic segment (A2), and a 15-mm inflatable balloon was introduced via the guide wire (A3) and gradually expanded to a diameter of 15 mm (A4 and A5). After expansion, X-ray revealed that the stenotic segment was well expanded (B).
Figure 6 Computed tomography virtual colonoscopy.
Computed tomography virtual colonoscopy revealed partial wall thickening and luminal stenosis in the sigmoid colon (arrow, A), as well as unobstructed lumen and smooth mucosa of the descending colon (B), transverse colon (C), ascending colon (D) and cecum (E). Sagittal reconstruction showed stenosis of the sigmoid colon (arrow, F).
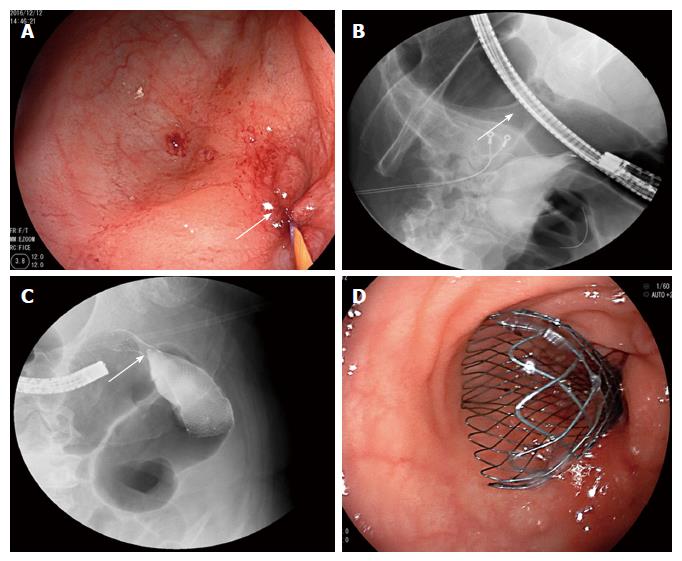
Figure 7 Stent placement for sigmoid colon stenosis.
The patient underwent stent placement for sigmoid colon stenosis. A guide wire was inserted via electronic colonoscopy to the proximal end of the stenotic segment (arrow, A). X-ray radiography confirmed that the guide wire had achieved the correct position and showed that the stenotic segment was 4 cm long (arrow, B). Additionally, X-ray showed that an 8-cm-long self-expandable memory metallic stent had been placed at the correct location (arrow, C). Colonoscopy confirmed that the distal end of the stent was at the correct location (D).
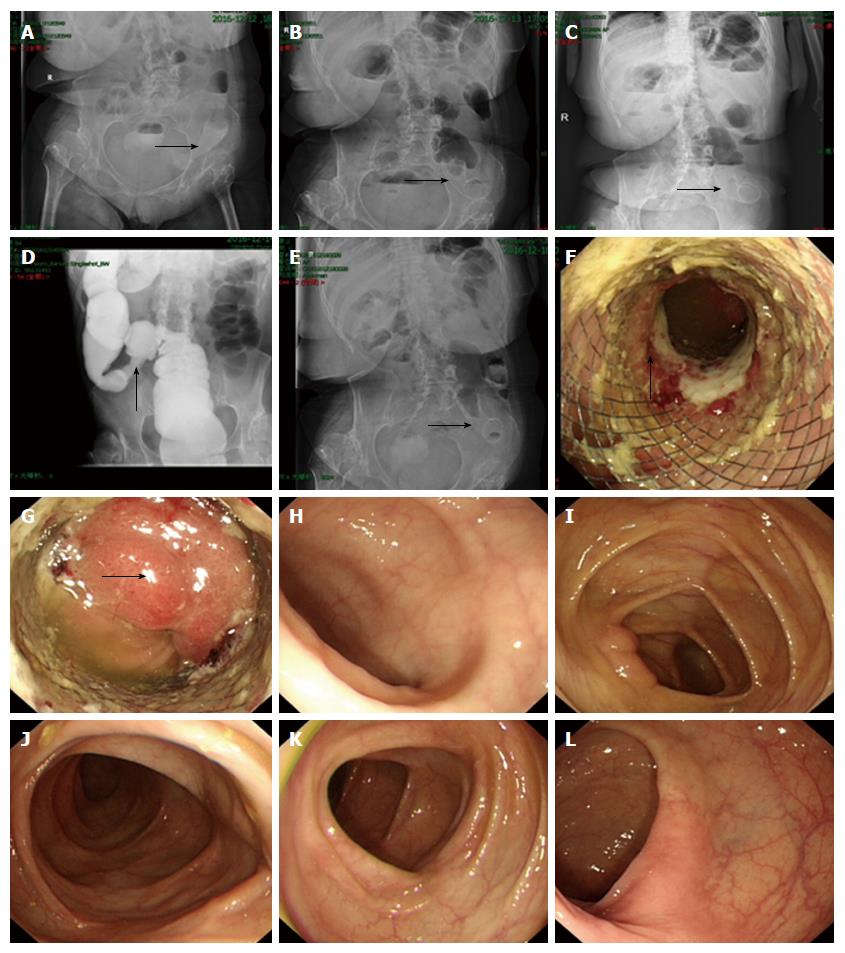
Figure 8 Abdominal X-ray and overall colonoscopy after stent implantation.
Plain abdominal X-ray performed on the day of stenting showed that the stent was partially expanded (arrow, A). On post-placement day 1, the stent showed further expansion (arrow, B), and on day 2 showed full expansion (arrow, C). Colonography showed that the stenotic sigmoid colon segment was successfully expanded (arrow, D). On day 6, plain abdominal X-ray showed that the stent remained completely expanded and stably positioned (arrow, E). On day 8, electronic colonoscopy showed the stenotic sigmoid colon segment was expanded by the metallic stent, with local colonic mucosa embedded in the stent meshes, and the colonic mucosa in the upper part of the stent showed congestion, edema, erosion and ulcer (arrow, F). The endoscope was able to pass through the stenotic segment, and the colonic mucosa in the upper edge of the stent showed congestion and edema (arrow, G). The mucosa of the terminal ileum (H), ileocecal junction (I), transverse colon (J), descending colon (K) and rectum (L) was smooth, had clear vascular texture, and showed no erosion, ulceration or neoplasm.
Figure 9 Laparoscopic sigmoidectomy.
The patient underwent a laparoscopic sigmoidectomy. Intraoperatively, sigmoid colon stenosis was visible (arrow, A) and the stenotic segment showed adhesions to the left-side pelvic wall and uterus (arrow, B). After separation of the adhesions, the stenotic segment was dissected at sites about 10 cm beyond both ends of the stenotic segment (C and D), and an end-to-end anastomosis was made between the descending colon and rectum (arrows, E and F).
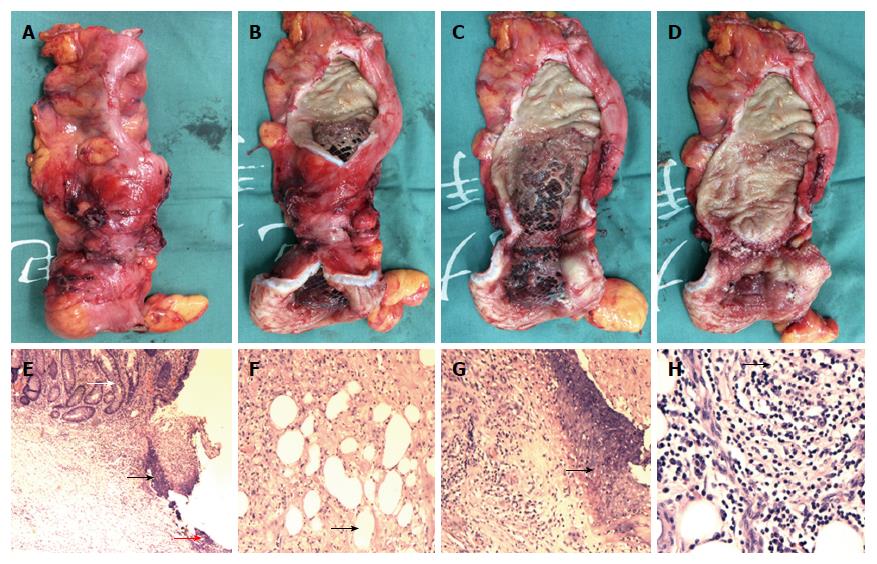
Figure 10 Specimen and pathological analysis.
The resected specimen showed stenotic sigmoid colon (A and B), with obvious compression by the metallic stent visible (C and D). Pathological analysis showed multiple ulcers in the mucosa (E, black arrow head), with the deepest ulcer penetrating through the muscle layer and reaching the mesenteric adipose tissue (F and H, black arrow head). Fibrous scar tissue (E, red arrow head) was visible at the ulcer base (G, black arrow head), but the structure of the mucosa around the ulcer was roughly normal (E, white arrow head), with no granuloma, vasculitis, lymphatic tissue hyperplasia, or full-thickness inflammatory changes (E-H). Hematoxylin and eosin staining; magnification of × 40 for E, × 100 for F and G, × 200 for H.
- Citation: Zhang ZM, Lin XC, Ma L, Jin AQ, Lin FC, Liu Z, Liu LM, Zhang C, Zhang N, Huo LJ, Jiang XL, Kang F, Qin HJ, Li QY, Yu HW, Deng H, Zhu MW, Liu ZX, Wan BJ, Yang HY, Liao JH, Luo X, Li YW, Wei WP, Song MM, Zhao Y, Shi XY, Lu ZH. Ischemic or toxic injury: A challenging diagnosis and treatment of drug-induced stenosis of the sigmoid colon. World J Gastroenterol 2017; 23(21): 3934-3944
- URL: https://www.wjgnet.com/1007-9327/full/v23/i21/3934.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i21.3934