Copyright
©The Author(s) 2016.
World J Gastroenterol. Dec 21, 2016; 22(47): 10287-10303
Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10287
Published online Dec 21, 2016. doi: 10.3748/wjg.v22.i47.10287
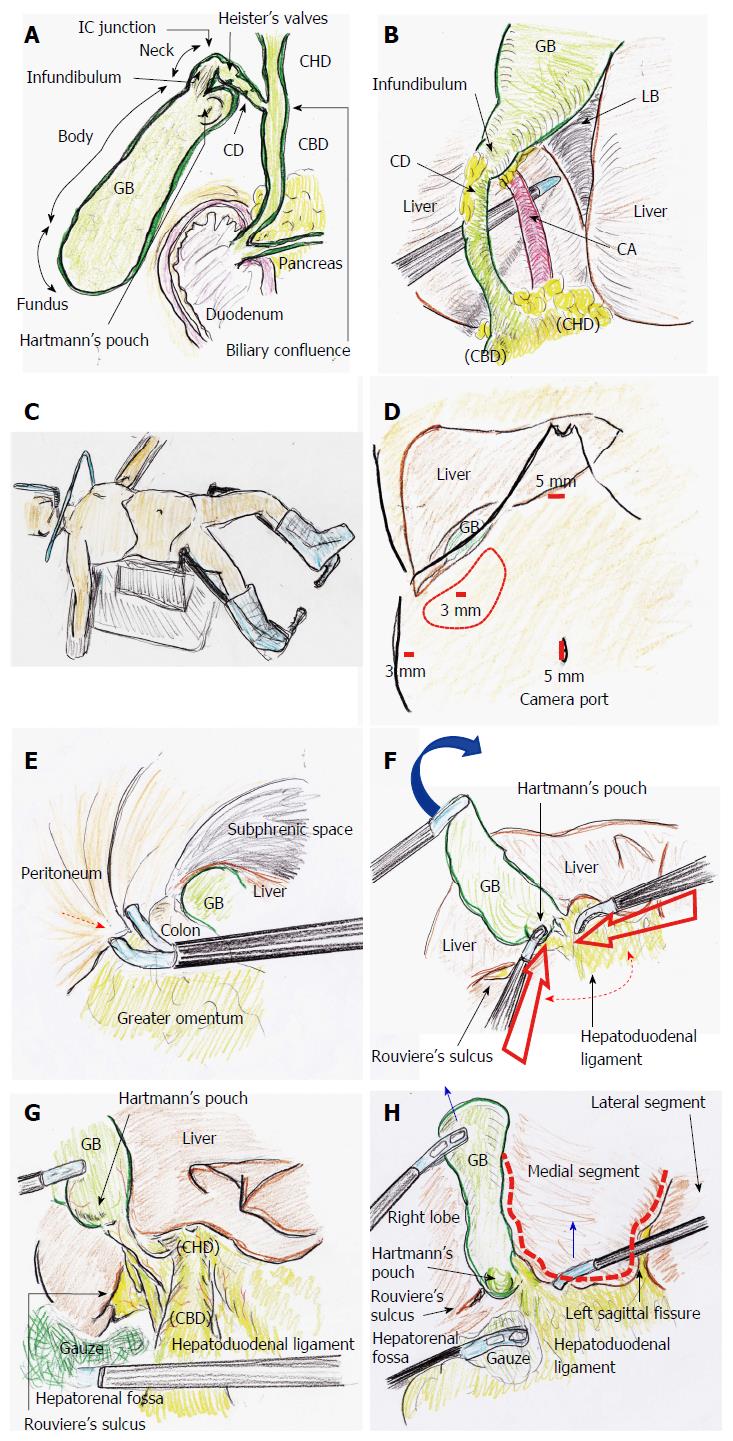
Figure 1 Tips and pitfalls of laparoscopic cholecystectomy.
A: Anatomy is important when performing LC; B: Strasberg’s CVS is shown; C: The patient is placed in a combination of an open-leg supine position and lithotomy position; D: Four ports are placed. The operator’s lateral port should be adequately placed (red circle); E: Port placement (red arrow) should be performed without any injuries; F: The GB fundus is superiorly and cranially lifted (blue arrow). The operator’s ports should then be placed with the forceps tip positioned at an adequate degree around Calot’s triangle (dotted arrow); G: Gauze is placed to dilate the hepatorenal fossa. The hepatoduodenal ligament is stretched. Rouviere’s sulcus and Hartmann’s pouch are confirmed; H: The left sagittal fissure is confirmed. A U-shaped line (dotted line) is visually traced from the round ligament of the liver to the left side of the GB. The bottom plateau of this U-shaped line necessarily involves the CHD and hepatic hilum. Adequate retractions are performed (blue arrows). CD: Cystic duct; CHD: Common hepatic duct; CVS: Critical view of safety; GB: Gallbladder; IC: Infundibulum-cystic duct; LB: Liver bed; LC: Laparoscopic cholecystectomy.
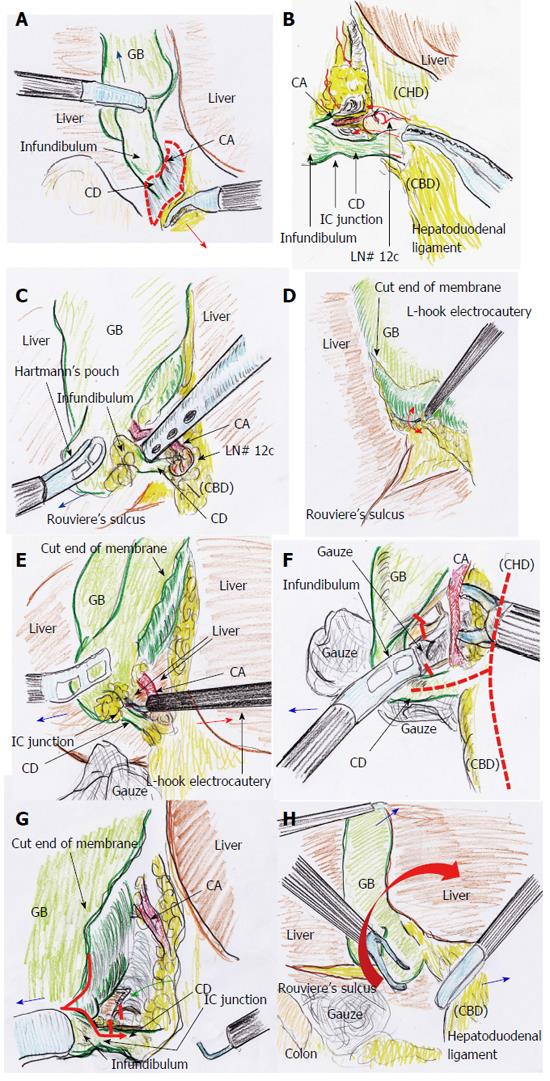
Figure 2 Tips and pitfalls of laparoscopic cholecystectomy.
A: Countertraction by grasping tissue (red arrow) is a useful dissection, and a dissectable/cuttable layer (dotted circle) is made under coordinated retraction (blue arrow); B: Blunt dissection in the overhead view is useful around Calot’s triangle (red arrows); C: Blunt dissection by suction in the overhead view is also useful under adequate retraction (blue arrow); D: A dissectible/cuttable layer is created and should be intentionally traced as close to the GB as possible. The width of the dissectable/cuttable layer is confirmed with a reciprocating L-hook (red arrow); E: A safe field is routinely made to the foreground. Tension is created with an L-hook (red arrow), and the tissue is then cut by energization. Adequate traction is performed (blue arrow); F: Hartmann’s pouch should be pulled laterally and inferiorly (blue arrow) to open the anterior left side of Calot’s triangle and create a wider angle between the CD and CHD (dotted line). A parallel junction of the CD with the CHD should be avoided. Nerves around the GB neck and CD are cut nearly at the GB (red lines); G: Hartmann’s pouch should be pulled laterally and inferiorly (blue arrow). The GB should be followed down to the presumed point of the IC junction, as close to the GB side as possible (red arrow). Nerves around the GB neck and the CD are cut (red lines). A partial penetration window is made to confirm the dorsal side (green arrow). The anterior left side of Calot’s triangle is adequately exposed in the overhead view; H: The posterior right side of Calot’s triangle is exposed and dissected while applying superior and medial traction of the GB infundibulum or Hartmann’s pouch (red arrow). The GB should never be pushed directly to the liver side. Supportive tractions are performed (blue arrows). CD: Cystic duct; CHD: Common hepatic duct; CVS: Critical view of safety; GB: Gallbladder; IC: Infundibulum-cystic duct; LB: Liver bed; LC: Laparoscopic cholecystectomy.
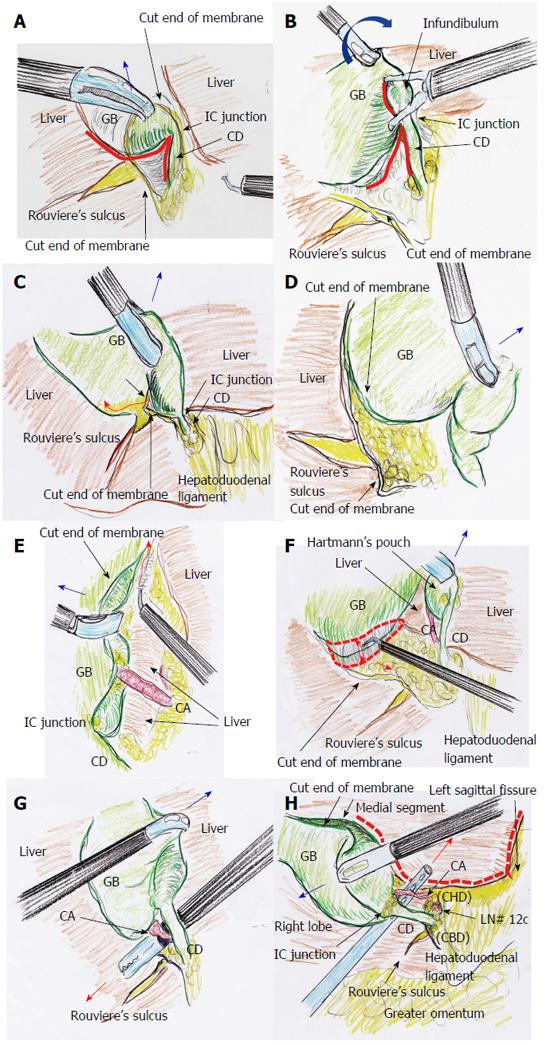
Figure 3 Tips and pitfalls of laparoscopic cholecystectomy.
A: Adequate retraction is performed for the laparoscopic view from underneath (blue arrow). Confirmation of the S-like curve on Hartmann’s pouch, infundibulum, IC junction, and CD is important (red line); B: The IC junction is confirmed as an inverted V shape (red line) because of the superior and medial traction of the GB (blue arrow); C: The cutline of the membrane is made to the GB body at a safe distance from Rouviere’s sulcus (red arrow). Adequate retraction is performed (blue arrow); D: Dissectable tissue around the GB should never be followed into Rouviere’s sulcus. Uncoupling of the GB wall and fatty fissure of Rouviere’s sulcus is important to avoid any biliary injuries. Adequate retraction is performed (blue arrow); E: Approximately two-thirds or half of the GB body is removed from the LB in the overhead view. A dissectable/cuttable layer is cut by L-hook electrocautery (red arrow) under adequate retraction (blue arrow), as close to the GB as possible; F: Approximately two-thirds or half of the GB body is removed from the LB in the view from underneath with adequate retraction (blue arrow). The dissectable/cuttable layer (dotted circle) is cut as close to the GB as possible using the L-hook electrocautery technique (red arrows); G: The CVS is ventrally confirmed (red arrow) under counter-retraction (blue arrow). Approximately two-thirds or half of the GB body is removed from the LB. Rouviere’s sulcus is far from the CD and GB; H: The CVS is dorsally confirmed (red arrow) under counter-retraction (blue arrow). Approximately two-thirds or half of the GB body is removed from the LB. Rouviere’s sulcus is located far from the CD and GB. The U-like line from the round ligament of the liver to the left side of the GB is visually traced (dotted line). CD: Cystic duct; CHD: Common hepatic duct; CVS: Critical view of safety; GB: Gallbladder; IC: Infundibulum-cystic duct; LB: Liver bed; LC: Laparoscopic cholecystectomy.
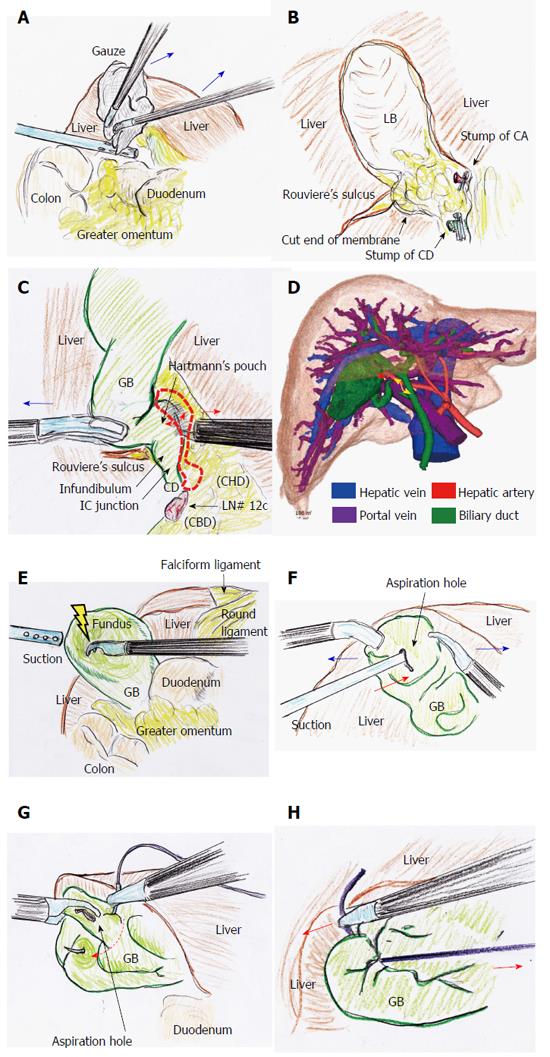
Figure 4 Tips and pitfalls of laparoscopic cholecystectomy.
A: Adequate compression using gauze (blue arrows) works well to stop bleeding at the LB; B: Hemostasis by thermal spread should be never used, nearly at the LB of the GB neck, Rouviere’s sulcus, and CD stump; C: The GB neck and Hartmann’s pouch often extend into the dorsal space due to inflammatory change and/or healing contracture, and unexpected excursions of important ducts and vessels may occur (dotted area). The dissectable/cuttable layer is cut under adequate retraction (blue arrow) as close to the GB as possible using the L-hook electrocautery technique (red arrows); D: Surgeons should not hesitate to perform preoperative detailed imaging studies in complicated cases. The CD (yellow arrow) and CA (red arrow) can be clearly detected on the 3D image; E: The GB is decompressed at the fundus by a dissector with energization; F: Under GB fixation (blue arrows), aspiration is surely performed (red arrow); G: A couple of sutures are placed to close an aspiration hole (dotted arrow); H: The aspiration hole is promptly closed by an extracorporeal ligation (red arrows). CD: Cystic duct; CHD: Common hepatic duct; CVS: Critical view of safety; GB: Gallbladder; IC: Infundibulum-cystic duct; LB: Liver bed; LC: Laparoscopic cholecystectomy.
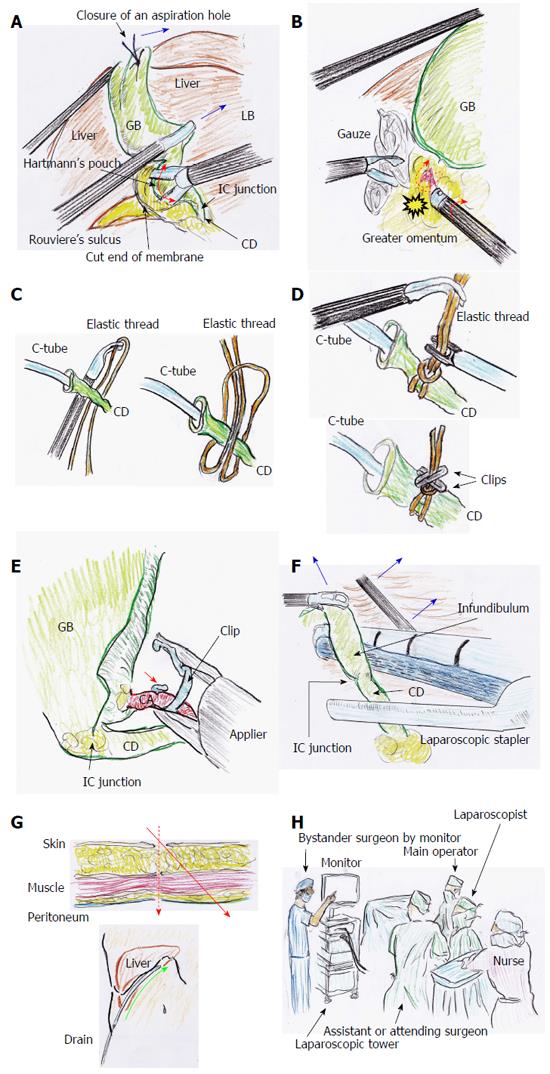
Figure 5 Tips and pitfalls of laparoscopic cholecystectomy.
A: After GB decompression by aspiration, the GB neck and/or Hartmann’s pouch can be pulled from the dorsal space. Hence, dissection can be performed as close to the GB as possible (red arrow) under adequate retractions (blue arrow); B: The rubbing of a bleeding vessel or oozing tissue (dotted arrow) by a button-shaped electrode with suction with a soft-coagulation system is a key technique for reliable hemostasis. During this hemostasis, subtle rotation of the electrode is important (red arrow); C: An elastic thread is never ligated directly; D: Clips are positioned to establish angular separation; E: A clip should be applied with the tip extending beyond the duct or vessels (red arrow); F: If the CD is too thick, loop ligation or a laparoscopic stapler can be chosen, under adequate retractions (blue arrows); G: Laparoscopic port penetrates abdominal wall at right angle (dotted arrow). A drain pathway through the abdominal wall is remade from the same skin incision (red arrow), to make the best drain placement (green arrow); H: A detached observer may be an actual solution for prevention of misidentification during LC. CD: Cystic duct; GB: Gallbladder; IC: Infundibulum-cystic duct; LC: Laparoscopic cholecystectomy.
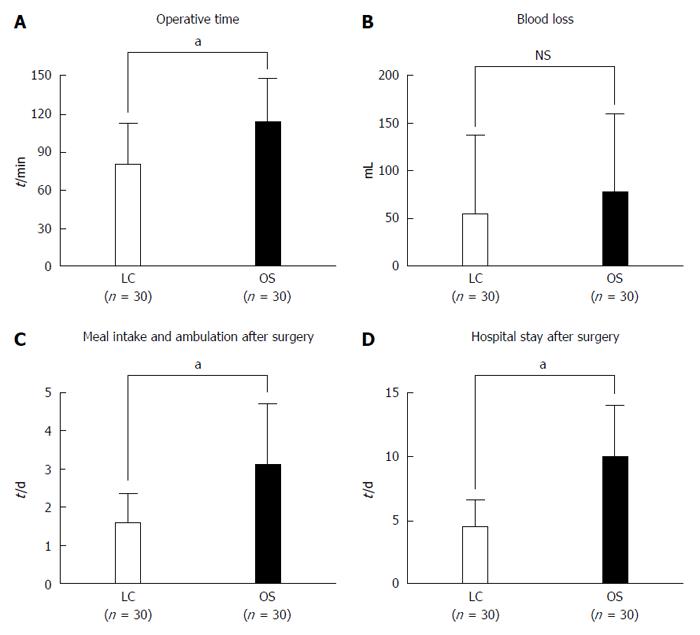
Figure 6 Tips and pitfalls of laparoscopic cholecystectomy.
A: Operative time; B: Intraoperative blood loss; C: Postoperative time to adequate meal intake and ambulation; D: Postoperative hospital stay after surgery were compared between LC and OS among patients undergoing emergency treatment for acute cholecystitis. There were significant differences not in blood loss but in operative time, postoperative duration until adequate meal intake and ambulation, and postoperative hospital stay (aP < 0.05). NS: Not significant; LC: Laparoscopic cholecystectomy.
- Citation: Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, Kato S, Yasukawa D, Aisu Y, Sasaki M, Kimura Y, Takamatsu Y, Naito M, Nakauchi M, Tanaka T, Gunji D, Nakamura K, Sato K, Mizuno M, Iida T, Yagi S, Uemoto S, Yoshimura T. Protocol for laparoscopic cholecystectomy: Is it rocket science? World J Gastroenterol 2016; 22(47): 10287-10303
- URL: https://www.wjgnet.com/1007-9327/full/v22/i47/10287.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i47.10287