Copyright
©The Author(s) 2016.
World J Gastroenterol. Nov 7, 2016; 22(41): 9127-9140
Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9127
Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9127
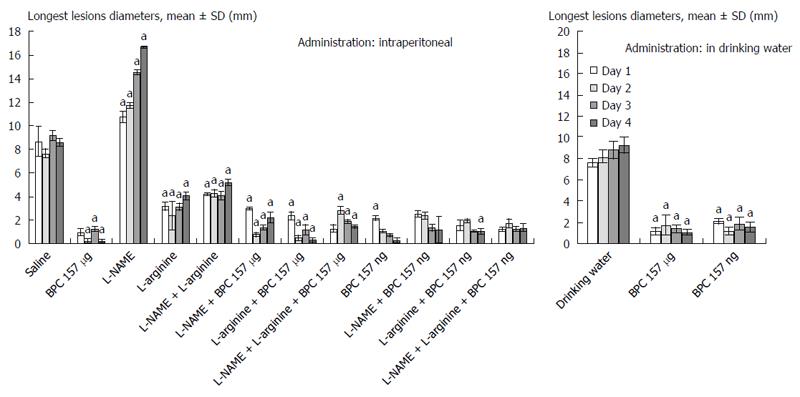
Figure 1 Gastric lesions, sum of the longest lesions diameters, mean ± SD, mm, in rats that underwent esophagogastric anastomosis.
Medication (/kg) given intraperitoneally (ip) (once time daily) or continuously in drinking water (po) after the creation of an esophagogastric anastomosis in rats. BPC 157 (10 μg, 10 ng), L-NAME (5 mg), and L-arginine (100 mg) given alone and/or combined intraperitoneally with the first application at 30 min after anastomosis creation and the last at 24 h before sacrifice. Drinking water alone (12 mL/d per rat) or BPC 157 in drinking water (10 μg, 10 ng/kg; 0.16 μg, 0.16 ng/mL) was provided continuously until sacrifice. aP < 0.05, at least, vs control.
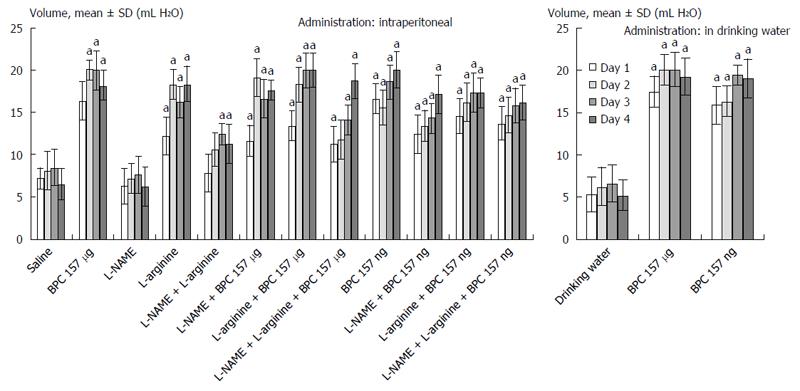
Figure 2 Anastomosis strength.
Water volume that could be sustained before leakage, mean ± SD, mL, in rats that underwent esophagogastric anastomosis. Medication (/kg) given intraperitoneally (ip) (once time daily) or continuously in drinking water (po) after the creation of esophagogastric anastomosis in rats. BPC 157 10 μg and 10 ng, L-NAME 5 mg, and L-arginine 100 mg given alone and/or combined intraperitoneally with the first application at 30 min after anastomosis creation and last at 24 h before sacrifice. Drinking water alone (12 mL/d per rat) or BPC 157 in drinking water (10 μg, 10 ng/kg; 0.16 μg, 0.16 ng/mL) was provided continuously until sacrifice. aP < 0.05, at least, vs control.
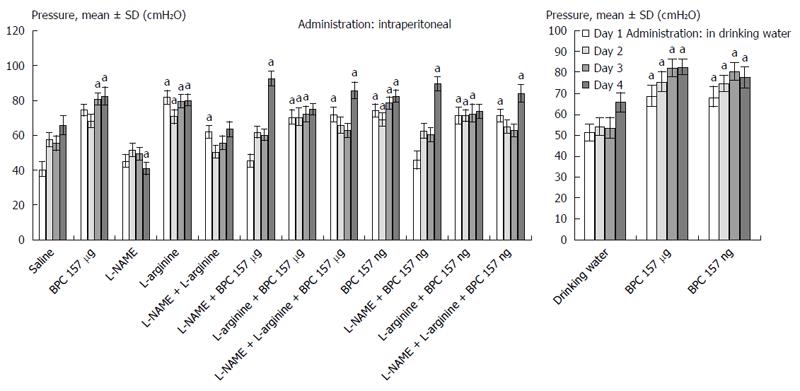
Figure 3 Pressure in the esophagus at the anastomosis site.
Mean ± SD, cmH2O, in rats that underwent esophagogastric anastomosis. Medication (/kg) given intraperitoneally (ip) (once time daily) or continuously in drinking water (po) after the creation of esophagogastric anastomosis in rats. BPC 157 10 μg and 10 ng, L-NAME 5 mg, and L-arginine 100 mg given alone and/or combined intraperitoneally with the first application at 30 min after anastomosis creation and last at 24 h before sacrifice. Drinking water alone (12 mL/d per rat) or BPC 157 in drinking water (10 μg, 10 ng/kg; 0.16 μg, 0.16 ng/mL) was provided continuously until sacrifice. aP < 0.05 at least vs control. The values of 68-76 cm H2O for the lower esophageal sphincter were considered to be normal, as determined previously[17,18,20-23].
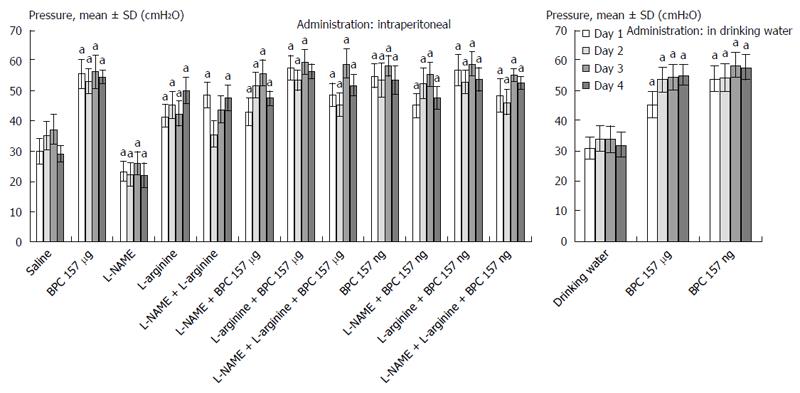
Figure 4 Pressure in the pyloric sphincter.
Mean ± SD, cmH2O, in rats that underwent esophagogastric anastomosis. Medication (/kg) given intraperitoneally (ip) (once time daily) or continuously in drinking water (po) after the creation of esophagogastric anastomosis in rats. BPC 157 10 μg and 10 ng, L-NAME 5 mg, and L-arginine 100 mg given alone and/or in combination intraperitoneally with the first application at 30 min after anastomosis creation and last at 24 h before sacrifice. Drinking water alone (12 mL/d per rat) or BPC 157 in drinking water (10 μg, 10 ng/kg; 0.16 μg, 0.16 ng/mL) was provided continuously until sacrifice. aP < 0.05, at least vs control. The values of 68-74 cm H2O for pyloric sphincter were considered normal, as previously determined[17,18,20-23].
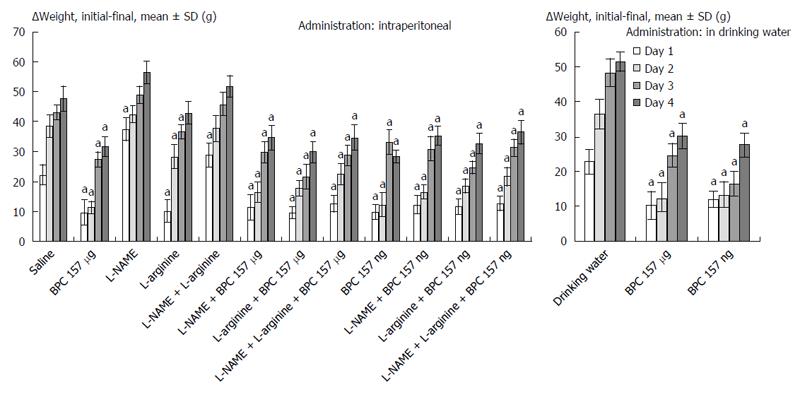
Figure 5 Weight loss (g) presented as the Δ between the initial and final weights[13,18], mean ± SD, in rats that underwent esophagogastric anastomosis.
Medication (/kg) given intraperitoneally (once time daily) or continuously in drinking water after the creation of an esophagogastric anastomosis in rats. BPC 157 10 μg and 10 ng, L-NAME 5 mg, and L-arginine 100 mg given alone and/or combined intraperitoneally with the first application at 30 min after anastomosis creation and the last at 24 h before sacrifice. Drinking water alone (12 mL/d per rat) or BPC 157 in drinking water (10 μg and 10 ng/kg; 0.16 μg and 0.16 ng/mL) was provided continuously until sacrifice. aP < 0.05, at least, vs control.
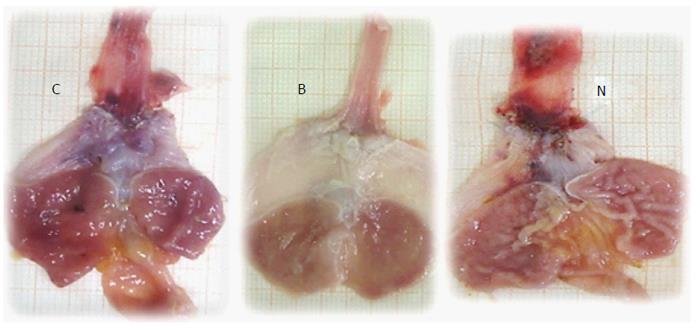
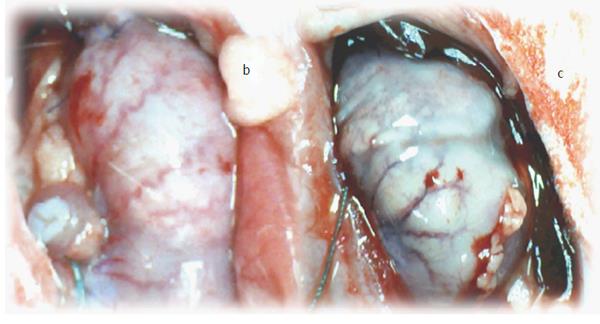
Figure 6 Illustrative gross presentation of rats that underwent esophagogastric anastomosis at post-operative day 4 and then received medication saline (control, C), BPC 157 (B), or L-NAME (N).
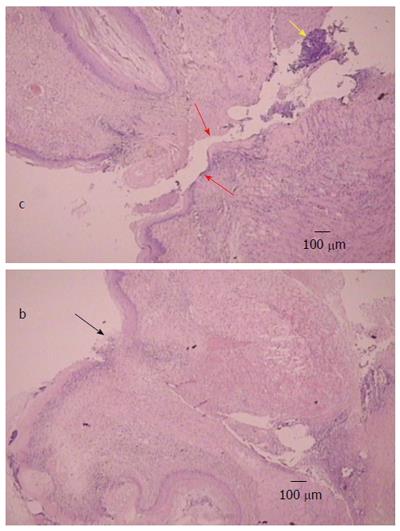
Figure 7 Illustrative microscopic presentation in rats that underwent esophagogastric anastomosis at post-operative day 2, hematoxylin eosin staining.
Separated anastomosis edges (red arrows) with neutrophils within the edges (yellow arrow) were consistently noted in controls (c). Separated wound edges (red arrows). Connected edges in rats that underwent esophagogastric anastomosis and treated with BPC 157 regimens (black arrow) (b).
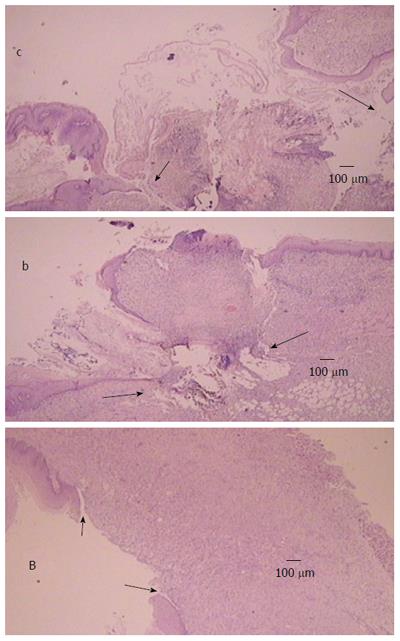
Figure 8 Illustrative microscopic presentation in rats that underwent esophagogastric anastomosis at post-operative day 4 [controls (c), BPC 157 (b)] and at post-operative day 7 [BPC 157 (B)], hematoxylin eosin staining.
Tissue destruction at the anastomosis edges (arrows) were consistently noted in controls (c), which is a presentation that precedes lethal outcome. Initial organization of the exudate (b) (arrows) and wound completely closed with granulation tissue (B) (arrows), which is consistently noted in rats that underwent esophagogastric anastomosis and were treated with BPC 157.
Figure 9 Blood vessels presentation at the ventral site of the stomach surface in rats that just underwent esophagogastric anastomosis.
In general, immediately after anastomosis creation and saline bath application, blood vessels disappeared from the rat gastric surface, and this effect lasts at least the next 15 min (scored Min/Med/Max 0/0/0), a period that was carefully monitored (control, c). With a BPC 157 bath immediately after anastomosis creation, the blood vessels did not disappear from the rat gastric surface; instead, these vessels remained present during at least the next 15 min of monitoring (BPC 157, b).
- Citation: Djakovic Z, Djakovic I, Cesarec V, Madzarac G, Becejac T, Zukanovic G, Drmic D, Batelja L, Zenko Sever A, Kolenc D, Pajtak A, Knez N, Japjec M, Luetic K, Stancic-Rokotov D, Seiwerth S, Sikiric P. Esophagogastric anastomosis in rats: Improved healing by BPC 157 and L-arginine, aggravated by L-NAME. World J Gastroenterol 2016; 22(41): 9127-9140
- URL: https://www.wjgnet.com/1007-9327/full/v22/i41/9127.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i41.9127