Copyright
©The Author(s) 2016.
World J Gastroenterol. Jan 28, 2016; 22(4): 1541-1550
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1541
Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1541
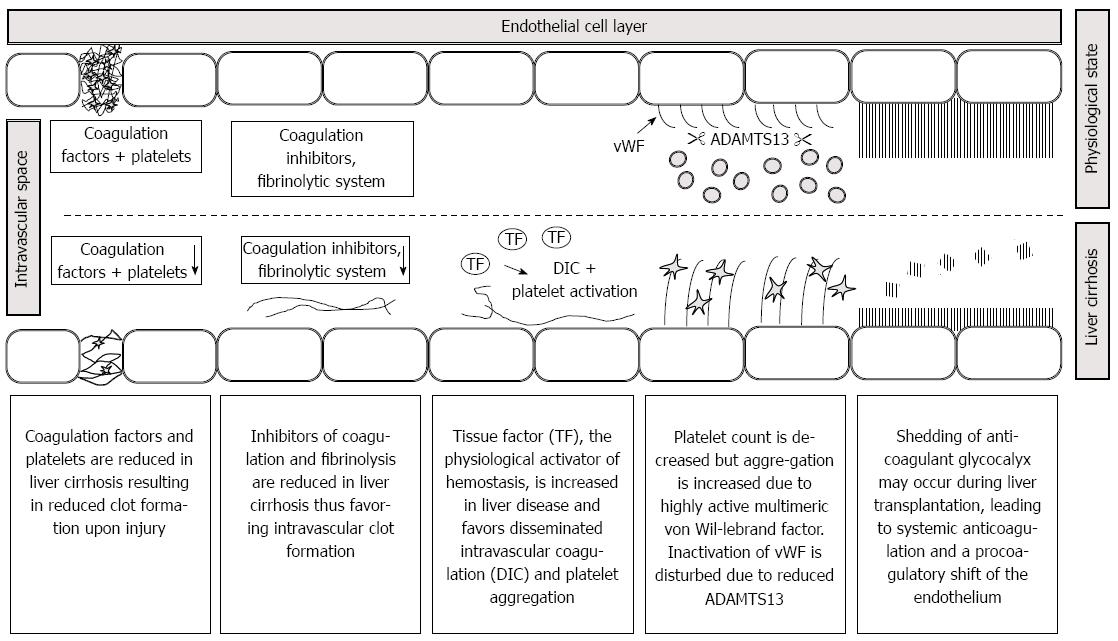
Figure 1 Pathophysiology of hemostasis in patients presenting for liver transplantation.
A reduction in coagulation factors due to end stage liver disease worsens clot quality. Decreases in anticoagulant factors, fibrinolysis and ADAMTS 13 as well as increases in tissue factor and von Willebrand factor multimeres may favor disseminated intravascular coagulation. Shedding of glycocalyx induces a systemic anticoagulation and contributes to the procoagulatory shift of the endothelium. Note that pathophysiology may vary upon the underlying liver pathophysiology.
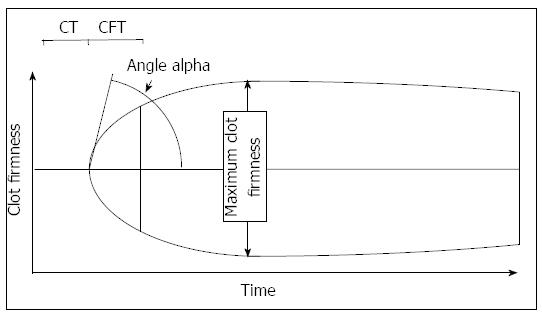
Figure 2 Thrombelastometry variables most often used to interpretate a tracing.
The thrombelastogram shows the firmness of a clot during the measurement time. The clotting time is defined as the time from recalcification and activation of blood samples to the onset of coagulation. The maximum clot firmness describes the physical properties of a clot, which is defined by platelet count and fibrinogen concentration. The α angle and the clot formation time describe the kinetics of clot generation.
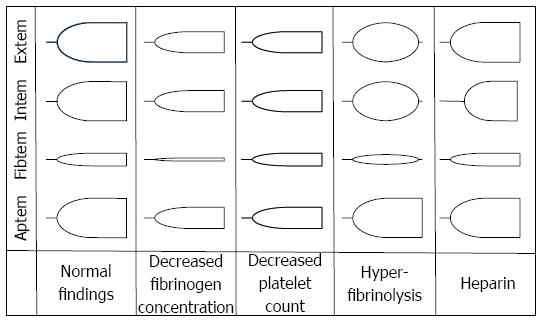
Figure 3 Typical changes in thrombelastometry tracings.
Shown are the effects of hypofibrinogenemia, thrombocytopenia, hyperfibrinolysis, and heparin.
- Citation: Hartmann M, Szalai C, Saner FH. Hemostasis in liver transplantation: Pathophysiology, monitoring, and treatment. World J Gastroenterol 2016; 22(4): 1541-1550
- URL: https://www.wjgnet.com/1007-9327/full/v22/i4/1541.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i4.1541