Copyright
©The Author(s) 2016.
World J Gastroenterol. Oct 14, 2016; 22(38): 8624-8630
Published online Oct 14, 2016. doi: 10.3748/wjg.v22.i38.8624
Published online Oct 14, 2016. doi: 10.3748/wjg.v22.i38.8624
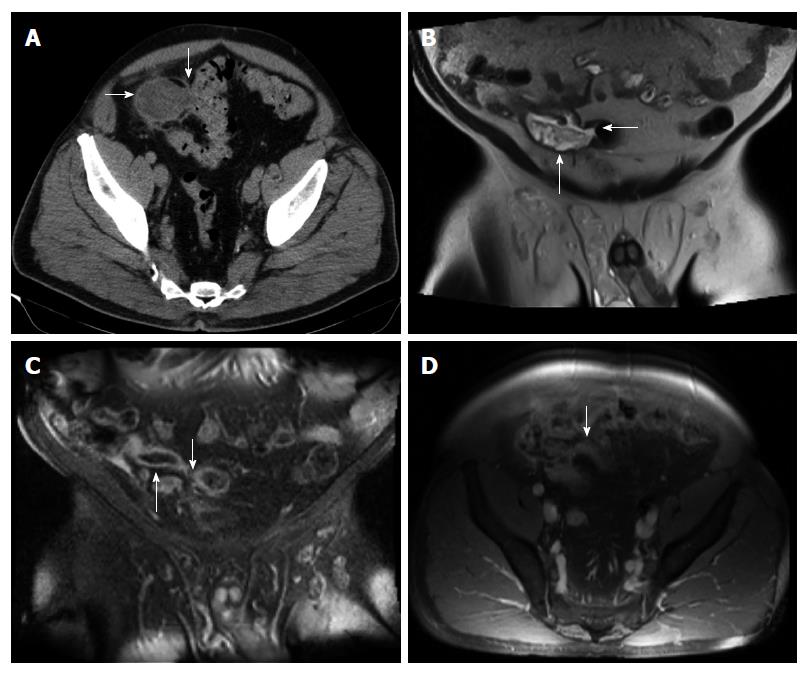
Figure 1 Abdomino-pelvic computed tomography.
A: Axial computed tomography (CT) image of the pelvis, enhanced with iodinated contrast, demonstrates a dilated, heterogeneous appendix (horizontal arrow) forming a fistula with sigmoid colon (fistulous connection at vertical arrow); B: Coronal T2-weighted fluid-sensitive MRI sequence depicts dilated, fluid-filled, appendix (vertical arrow), extending and forming a fistula with the sigmoid colon (horizontal arrow); C: Coronal post-gadolinium contrast enhanced T1-weighted MRI image demonstrates dilated appendix with non-enhanced, central fluid and enhanced wall (upward arrow) that extends towards sigmoid colon (downward arrow); D: Axial post-gadolinium contrast enhanced T1-weighted MRI image demonstrates abnormally thick and enhanced appendiceal wall (arrow) without significant surrounding inflammatory changes.
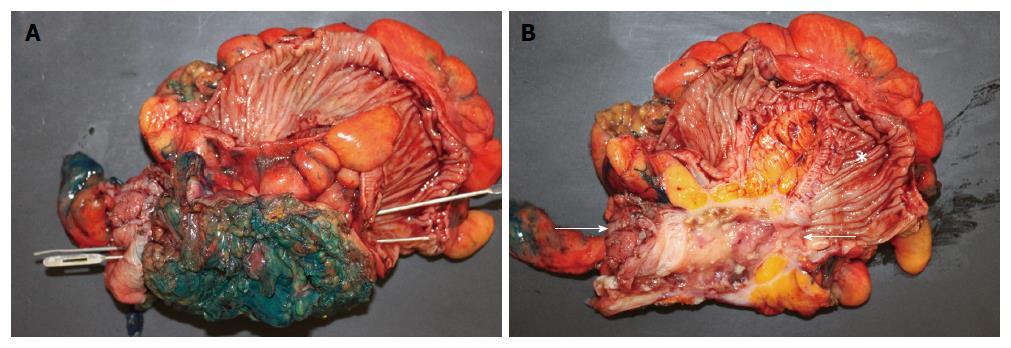
Figure 2 Open laparotomy revealed an extensive mass involving appendix, cecum, sigmoid colon, anterior abdominal wall, and urinary bladder.
A: Gross pathologic photograph shows entire surgically resected specimen (including appendix, cecum, sigmoid colon, part of bladder, and anterior abdominal wall) after bisecting the sigmoid colon that exposes the haustral folds within sigmoid, but before bisecting the centro-inferior tumor (note green ink identifying surgical margins of tumor). Insertion of two parallel probes (one inserted from left to right and the other inserted from right to left) demonstrate a fistula traveling from the cecum, on the bottom left, to the sigmoid, on the bottom right. Bisection of the centro-inferior tumor (B) reveals that the appendix forms the malignant fistula; B: Gross pathologic specimen after bisection of centro-inferior tumor (seen before bisection in A) exposes an irregular, cystically dilated, malignant appendix that forms the malignant fistula. It is lined by a variably thick wall composed of the mucinous adenocarcinoma and filled with viscous, mucoid, content. Sigmoid (star). Cecum is at left bottom of photograph immediately adjacent to arrow.
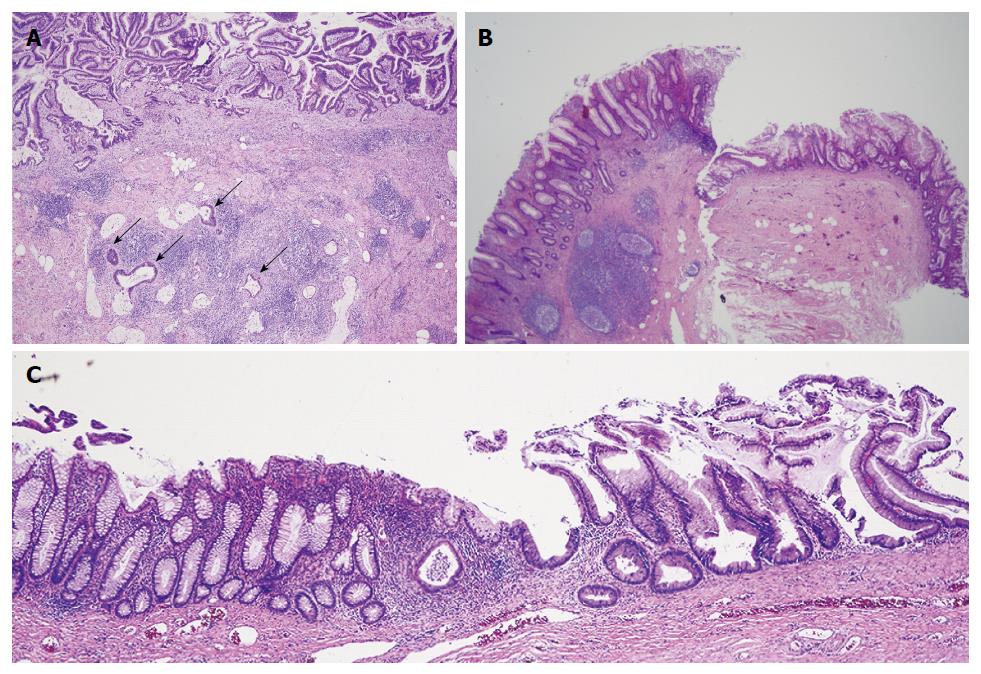
Figure 3 Microscopic pathology showed well-differentiated, invasive, mucinous, adenocarcinoma diffusely involving the appendix, sigmoid, and cecum through the serosa.
A: Low power photomicrograph of mucinous appendiceal adenocarcinoma (MAA) within fistulous (appendiceal) wall showing villoglandular adenomatous epithelium containing basophilic cells, within bizarre mucosal glands (upper area), and infiltration of cancerous mucinous glands deep in the wall (arrows). The fistulous wall also shows extensive fibrosis and chronic inflammation [hematoxylin-eosin staining (HE)]; B: Low power photomicrograph shows mucinous appendiceal adenocarcinoma with serrated glands, on the right, contiguous with normal cecal mucosa, with normal cecal glands, on the left (HE); C: Low power photomicrograph shows junction of mucinous appendiceal adenocarcinoma with serrated glands on the right, contiguous with normal sigmoid mucosa with normal glands, on the left (HE).
- Citation: Hakim S, Amin M, Cappell MS. Limited, local, extracolonic spread of mucinous appendiceal adenocarcinoma after perforation with formation of a malignant appendix-to-sigmoid fistula: Case report and literature review. World J Gastroenterol 2016; 22(38): 8624-8630
- URL: https://www.wjgnet.com/1007-9327/full/v22/i38/8624.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i38.8624