Copyright
©The Author(s) 2016.
World J Gastroenterol. Sep 7, 2016; 22(33): 7507-7517
Published online Sep 7, 2016. doi: 10.3748/wjg.v22.i33.7507
Published online Sep 7, 2016. doi: 10.3748/wjg.v22.i33.7507
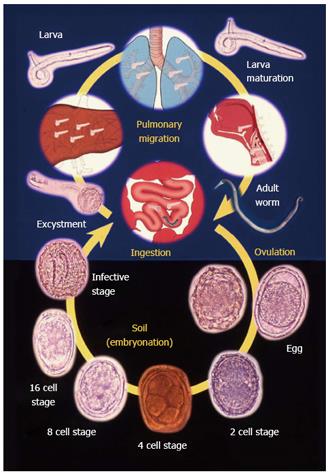
Figure 1 Life cycle of Ascaris lumbricoides.
Adapted from khuroo et al[5].
Figure 2 Sputum examination of a child with ascaris pneumonia showing filariform larva.
Figure 3 Massive aggregate of ascarides within jejunum causing obstruction, infarction and gangrene of bowel necessitating bowel resection.
Adapted from Khuroo[5].
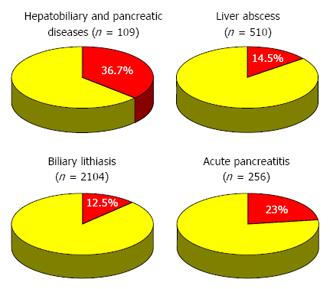
Figure 4 Impact of hepatobiliary and pancreatic ascariasis as an etiologic factor in biliary disease, hepatic abscesses, biliary lithiasis and acute pancreatitis.
Numbers in parenthesis shows number of patients with disease and percentages are those caused by ascariasis. Adapted from Ref. [1,3,6,37].
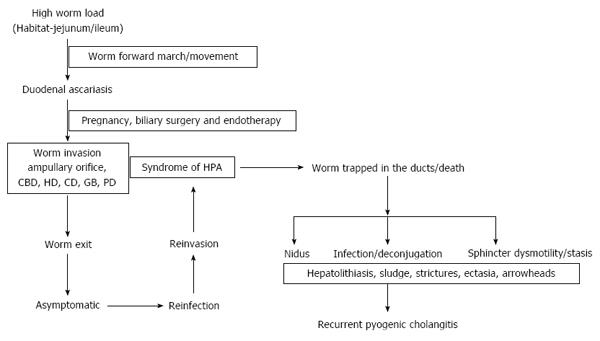
Figure 5 Pathogenesis and natural course of hepatobiliary and pancreatic ascariasis in high endemic regions.
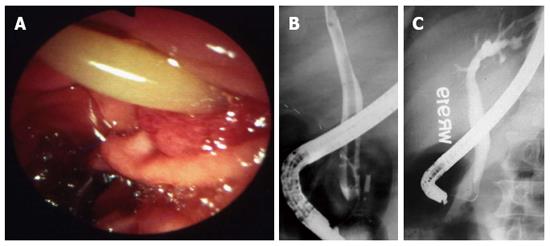
Figure 6 Duodenal ascariasis presenting as biliary colic.
A: Duodenoscopy showing adult ascaride in the ampullary orifice; B: Endoscopic retrograde cholangiogram showing long linear filling defect in the common bile duct; C: Cholangiogram after extraction of worms from bile duct. Patient had immediate relief of biliary colic. Adapted from Khuroo[5].
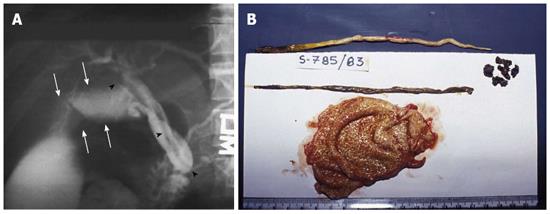
Figure 7 Choledochus ascariasis blocking orifice of cystic duct, causing acute obstructive cholecystitis, needing emergency cholecystectomy.
A: Endoscopic retrograde cholangiogram showing linear filling defect in common bile duct (black arrows). Cystic duct and gall bladder is grossly dilated (white arrows); B: Gall bladder showing inflamed gall bladder with 2 adult ascarides and few stones around macerated dead worm. Adapted from Khuroo[5].
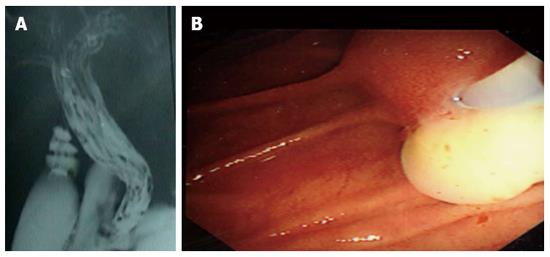
Figure 8 Hepatic ascariasis presenting as suppurative cholangitis.
A: Endoscopic retrograde cholangiogram showing palisading of ascarides in common bile ducts and hepatic ducts; B: Duodenoscopic view showing pus exuding from ampullary orifice.
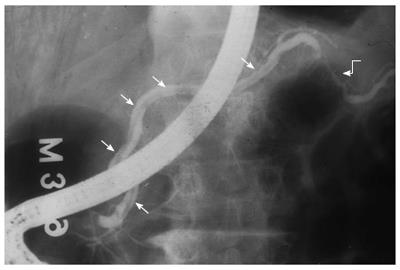
Figure 9 Pancreatic ascariasis presenting as necrotizing pancreatitis.
A linear filling defect is seen all along the pancreatic duct (straight arrows). A stricture is seen in the tail region (curved arrow) reminiscent of pancreatic necrosis. Adapted from Khuroo et al[2].
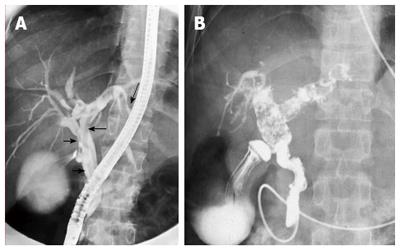
Figure 10 Recurrent pyogenic cholangitis aftermath of biliary ascariasis.
A: Endoscopic retrograde cholangiogram obtained 5 years prior to present admission revealing two long linear smooth filling defect in the common and left hepatic duct (arrows); B: Cholangiogram performed during present admission. Cholangiogram revealed biliary dilatation with multiple filling defects and cholangitic changes in the common hepatic, right and left hepatic duct. Naso-biliary tube is in place to treat pyogenic cholangitis. Adapted from Khuroo et al[4].
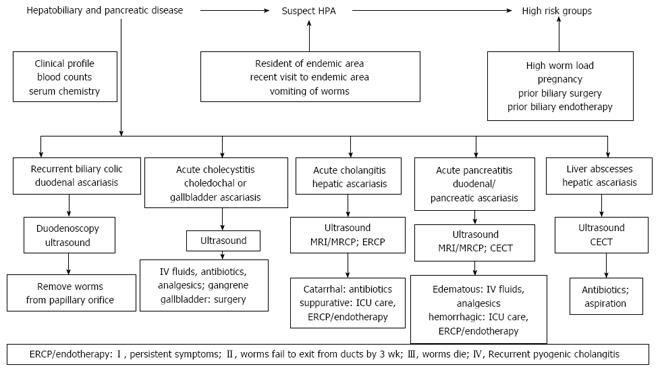
Figure 11 Flow chart showing diagnostic and management algorithm.
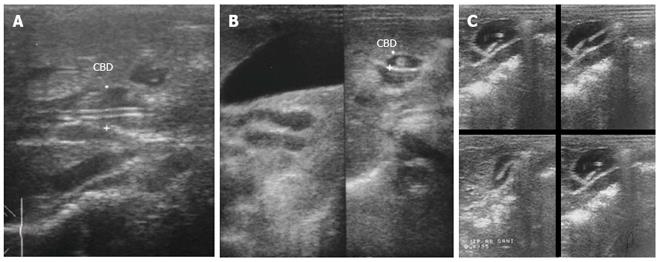
Figure 12 Ultrasonography images in hepatobiliary and pancreatic ascariasis.
A: Biliary ultrasound depicting four-line sign; B: Ultrasound showing tube like structure within common bile duct with distended gall bladder; C: Ascarides in gall bladder showing active movements as seen in serial images. Adapted from Khuroo[5].
Figure 13 Hepatic ascariasis presenting as suppurative cholangitis managed with nasobiliary tube drainage.
Note ascaride placed in common bile duct and left hepatic duct. Nasobiliary tube is in place to decompress and drain the duct.
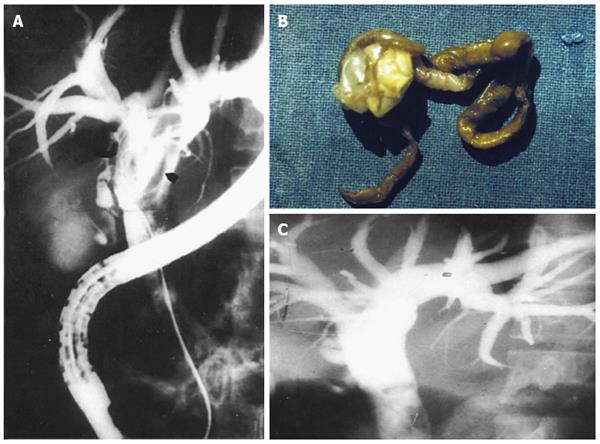
Figure 14 Endotherapy in hepatobiliary ascariasis.
A: Cholangiogram showing dilated ducts multiple linear filling defects; B: Dead ascaride extracted from biliary tract; C: Cholangiogram obtained after extraction of dead ascaris. Ducts are free of filling defects. Adapted from Khuroo et al[15].
- Citation: Khuroo MS, Rather AA, Khuroo NS, Khuroo MS. Hepatobiliary and pancreatic ascariasis. World J Gastroenterol 2016; 22(33): 7507-7517
- URL: https://www.wjgnet.com/1007-9327/full/v22/i33/7507.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i33.7507