Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 7, 2015; 21(41): 11832-11841
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11832
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11832
Figure 1 Duodenal adenocarcinoma imaged with magnifying endoscopy with narrow-band imaging.
White opaque substance (WOS) in lesion margins on magnifying endoscopy with narrow-band imaging (M-NBI). Speckled WOS is found at the lesion margins (arrows), and little is in the central area.
Figure 2 Diagnostic algorithm of magnifying endoscopy with narrow band imaging for superficial non-ampullary duodenal epithelial tumor.
From Kikuchi et al[16].
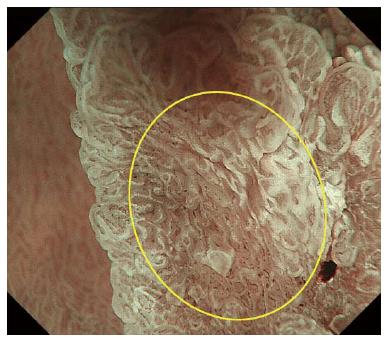
Figure 3 Duodenal adenocarcinoma imaged with magnifying endoscopy with narrow-band imaging.
An indistinct area of a marginal crypt epithelium (MCE) structure as imaged by magnifying endoscopy with narrow-band imaging (M-NBI). There are no discernible microsurface features (yellow circle).
Figure 4 Duodenal adenocarcinoma imaged with magnifying endoscopy with narrow-band imaging.
Because of uneven distribution of white opaque substance (WOS) on magnifying endoscopy with narrow-band imaging (M-NBI), this lesion displays multiple microsurface patterns as mixed-type (yellow circle).
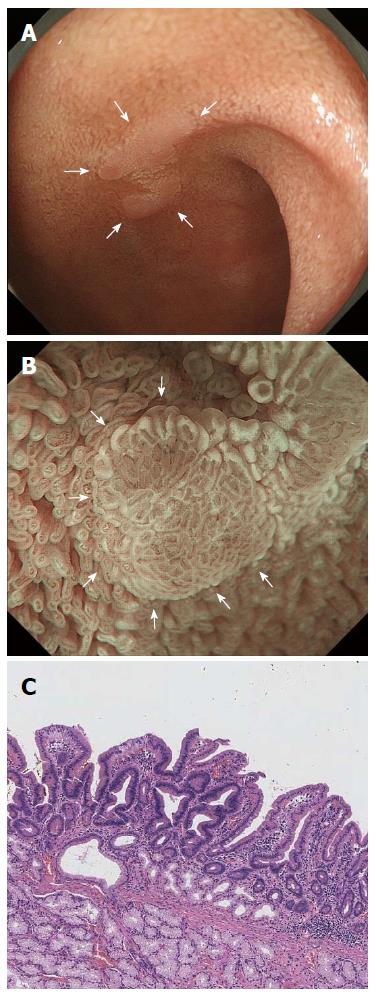
Figure 5 Magnifying endoscopy with narrow-band imaging imaging of a duodenal adenoma.
A: Endoscopic findings using conventional endoscopy with white light imaging. A pale, slightly elevated lesion (10 mm in diameter, arrow) is observed in the proximal duodenum; B: Endoscopic findings using magnifying endoscopy with narrow-band imaging (M-NBI). A demarcation line (DL, arrows) separates changes in the mucosal microsurface (MS) structure from the surrounding normal mucosa. Vessel plus surface (VS) classifications: V, Because of the white opaque substance (WOS), the morphology of the subepithelial microvessels cannot be observed, making this an absent microvascular (MV) pattern; S, The WOS has a regular reticular pattern with a symmetrical distribution and regular arrangement. Thus, this lesion is graded as a regular MS pattern using WOS as a marker for the MS pattern. The VS classification of this lesion was absent MV pattern and regular MS pattern (WOS+) with a DL. Therefore, the M-NBI diagnosis was benign; C: The final histological diagnosis was of a low-grade adenoma.
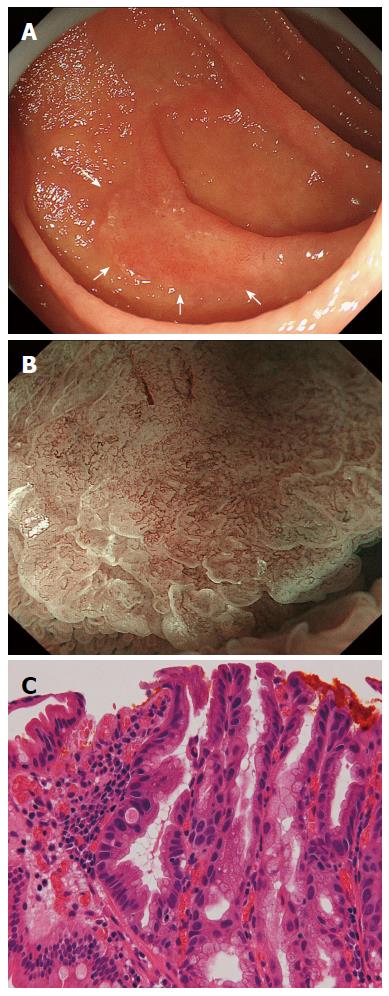
Figure 6 Duodenal adenocarcinoma with typical magnifying endoscopy with narrow-band imaging findings.
A: Endoscopic findings using conventional endoscopy with white light imaging. A reddish, slightly elevated lesion (13 mm in diameter, arrows) is observed in the second portion of the duodenum; B: Endoscopic findings using magnifying endoscopy with narrow-band imaging findings (M-NBI). A clear demarcation line (DL) is visible because of differences in the vessel plus surface (VS) component between the cancerous and noncancerous mucosa. V: Proliferation of microvessels with variable sizes, asymmetrical distribution and irregular arrangement make this an irregular microvascular (MV) pattern; S: There are areas where the marginal crypt epithelium (MCE) cannot be visualized and where the visible MCE shows a variety of morphologies, an asymmetrical distribution and an irregular arrangement. This lesion is assessed as an irregular mucosal microsurface (MS) pattern. The VS classification of this lesion was an irregular MV pattern and irregular MS pattern with a DL. Therefore, the M-NBI diagnosis was cancer; C: The final histological diagnosis was a well-differentiated intramucosal adenocarcinoma.
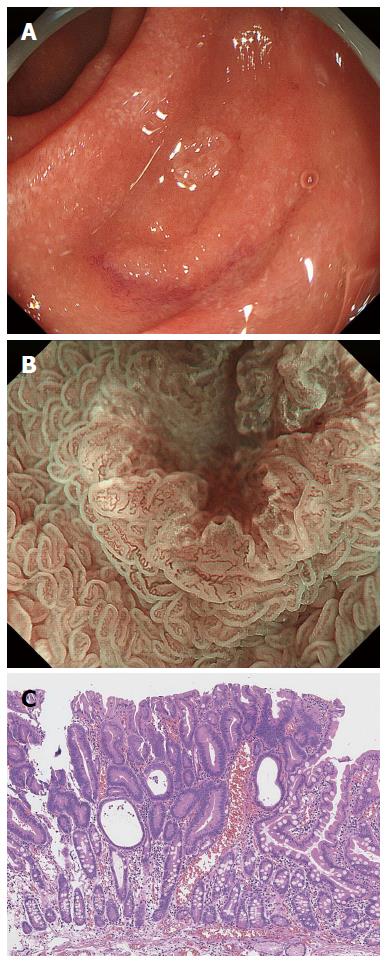
Figure 7 False-positive magnifying endoscopy with narrow-band imaging diagnosis.
A: Endoscopic findings using conventional endoscopy with white light imaging. A whitish, slightly depressed lesion (5 mm in diameter) is observed in the second portion of the duodenum. In this case, magnifying endoscopy with narrow-band imaging diagnosis (M-NBI) examination was conducted before biopsy; B: Endoscopic findings using M-NBI. A clear demarcation line (DL) is visible because of differences in the vessel plus surface (VS) component between the tumor and surrounding mucosa. V: The individual vessels show a variety of morphologies, such as open- and closed-looped and coil-shaped, with no two microvessels sharing the same morphology. The microvessels are anastomosing with each other within the intervening parts but show no consistent regularity. Therefore, this lesion was assessed as an irregular microvascular (MV) pattern; S: This individual section of marginal crypt epithelium (MCE) shows a curved morphology but lacks continuity or a consistent directionality, and the intervening parts are also irregular with unequal sizes. Therefore, this lesion was assessed as an irregular mucosal microsurface (MS) pattern. The VS classification of this lesion was an irregular MV pattern and irregular MS pattern with a DL. Therefore, the M-NBI diagnosis was cancer; C: The final histological diagnosis was a low-grade adenoma.
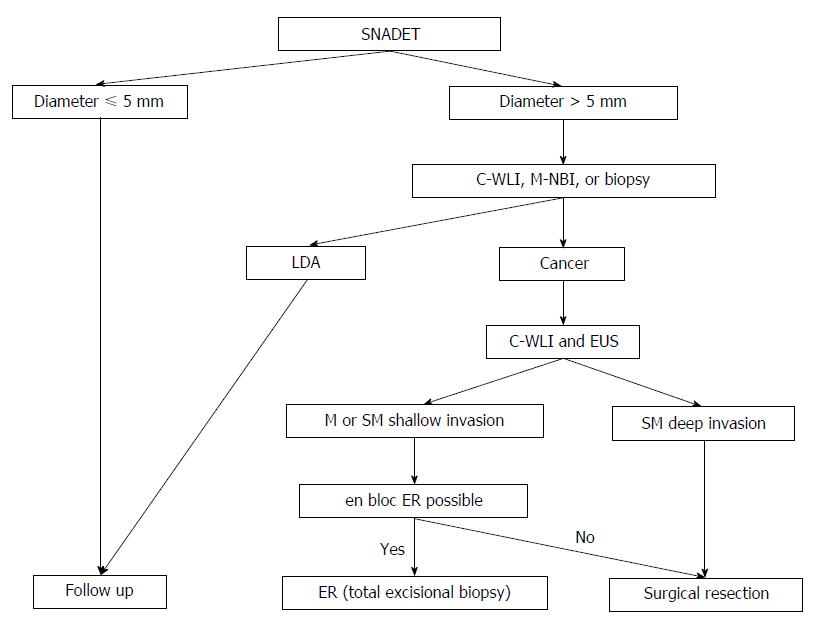
Figure 8 Suggested algorithm for the management of superficial non-ampullary duodenal epithelial tumor according to depth of invasion; tumor size; endoscopic findings, including magnifying endoscopy; and biopsy results.
Endoscopic features of cancer are a red color in the tumor; a nodular, rough surface on conventional white light imaging; a marginal type of milk-white mucosa; an unclassified vascular pattern; a frequency of ill-defined mucosal pattern; and a population of mixed-type lesions with multiple surface patterns on magnifying endoscopy with narrow-band imaging. Endoscopic features of submucosal carcinoma are ulceration and a 0-I or 0-IIa + IIc macroscopic type with a red color. SNADET: Superficial non-ampullary duodenal epithelial tumor; C-WLI: Conventional white-light imaging; M-NBI: Magnifying endoscopy with narrow-band imaging; LDA: Low-grade adenoma; EUS: Endoscopic ultrasonography; ER: Endoscopic resection.
- Citation: Tsuji S, Doyama H, Tsuji K, Tsuyama S, Tominaga K, Yoshida N, Takemura K, Yamada S, Niwa H, Katayanagi K, Kurumaya H, Okada T. Preoperative endoscopic diagnosis of superficial non-ampullary duodenal epithelial tumors, including magnifying endoscopy. World J Gastroenterol 2015; 21(41): 11832-11841
- URL: https://www.wjgnet.com/1007-9327/full/v21/i41/11832.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i41.11832