Copyright
©The Author(s) 2015.
World J Gastroenterol. Nov 7, 2015; 21(41): 11584-11596
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11584
Published online Nov 7, 2015. doi: 10.3748/wjg.v21.i41.11584
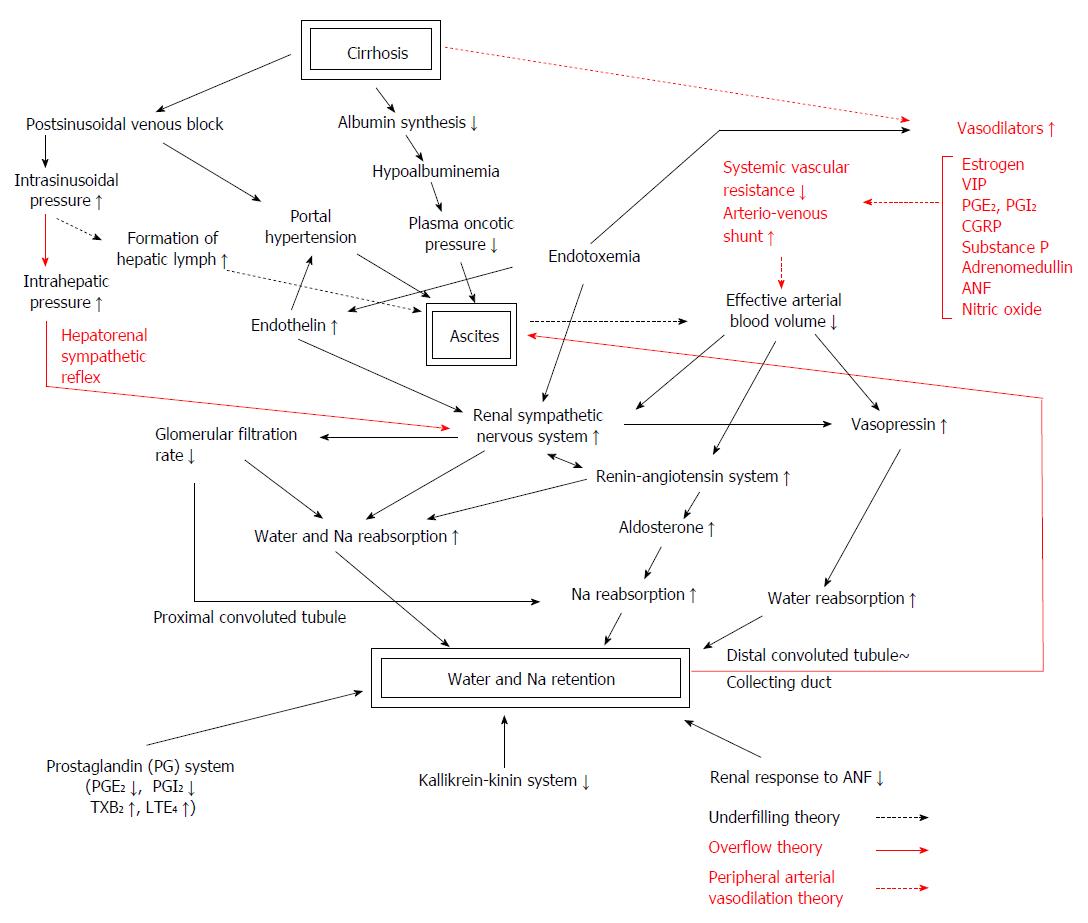
Figure 1 Phatophysiologic backgrounds and main theories of ascites formation in liver cirrhosis.
The pathogenetic events leading to ascites formation in patients with liver cirrhosis are multifactorial. They include hepatic venous outflow block, portal hypertension and hypoalbuminemia as hepatic factors, hyperdynamic circulation, peripheral arterial vasodilation, decreased effective circulating blood volume and altered neurohumoral systems as systemic circulatory factors, and enhanced salt and water reabsorption in proximal and distal nephron and convoluted duct related to intrarenal haemodynamic derangement as renal factors. They are closely interrelated and enhance salt and water reabsorption in the kidney. The activities of the two major vasoconstrictor and antinatriuretic systems, the renin-angiotensin-aldosteron system and the sympathetic nervous system, are increased in most cirrhotics with tense ascites. Increased plasma level of arginine vasopressin enhances water reabsorption in the collecting duct and contributes to water retention. Endothelin, an endothelial-derived peptide with marked vasoconstrictor activity, is also increased in advanced cirrhosis[86,87]. Increased endothelin levels were proven to be related to creatinine clearance, effective renal plasma flow[88], serum creatinine and blood pressure[89], and may also contribute to renal dysfunction in patients with cirrhosis[88]. Three main hypotheses, the underfilling theory, the overflow theory and the peripheral arterial vasodilation theory, are considered to explain variable pathophysiological changes occurred in a patient with advanced liver cirrhosis. VIP: Vasoactive intestinal peptide; CGRP: Calcitonin gene-related peptide; PG: Prostaglandin; TX; Thromboxane; LT: Leukotriene.
- Citation: Fukui H. Do vasopressin V2 receptor antagonists benefit cirrhotics with refractory ascites? World J Gastroenterol 2015; 21(41): 11584-11596
- URL: https://www.wjgnet.com/1007-9327/full/v21/i41/11584.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i41.11584