Copyright
©The Author(s) 2015.
World J Gastroenterol. Oct 28, 2015; 21(40): 11362-11370
Published online Oct 28, 2015. doi: 10.3748/wjg.v21.i40.11362
Published online Oct 28, 2015. doi: 10.3748/wjg.v21.i40.11362
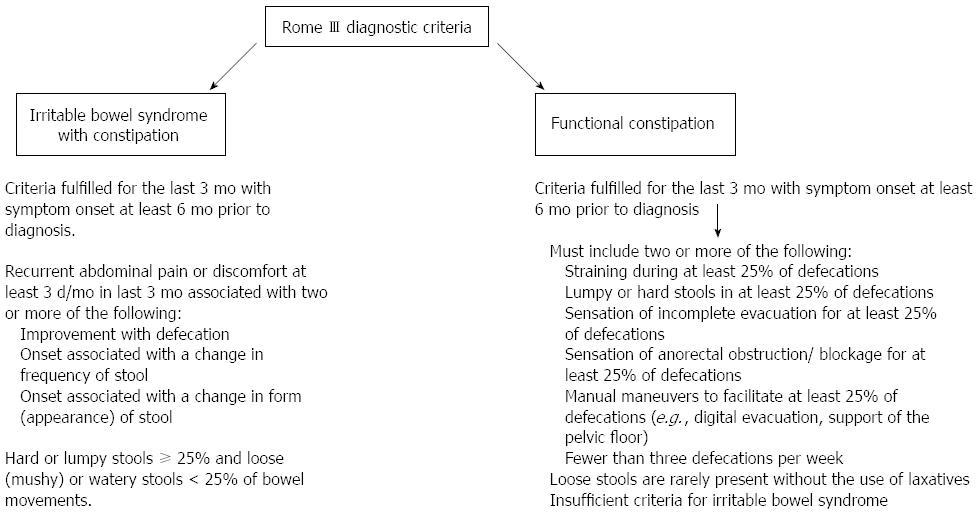
Figure 1 Rome III criteria for irritable bowel syndrome and functional constipation.
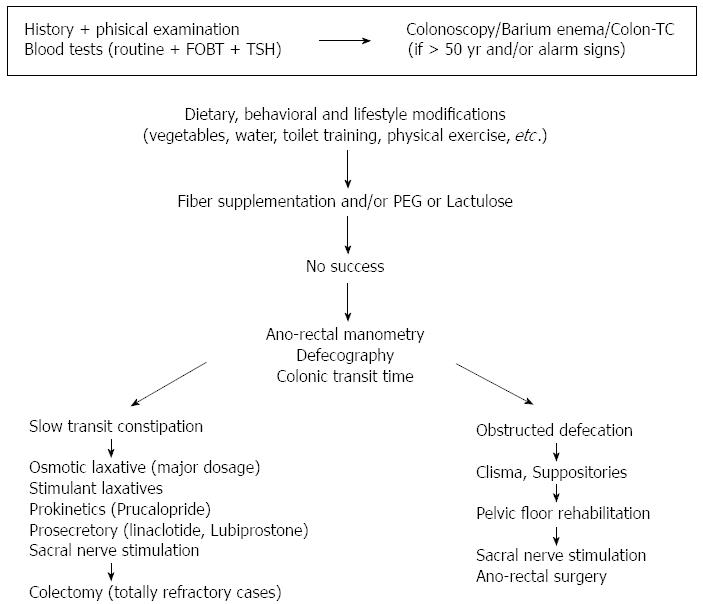
Figure 2 Multi-step management of chronic constipation.
After a careful history and some blood tests, if there are no alarm signs and the patient is < 50 years old the first line approach encompasses a correction of lifestyle and dietary habits (on the contrary a colonic morphological assessment by using colonoscopy or barium enema or colon-CT is advisable). If the results are not satisfying, fiber supplementation and/or therapy with polyethylene glycol (PEG) or lactulose are advisable. Should there be unsatisfactory results, “second line” drug therapy, using saline or stimulant or softening laxatives, could be suitable and, possibly using or adding the new drugs with a prokinetic or prosecretory effect (prucalopride, lubiprostone, linaclotide). At this step performing some diagnostic “second level” exams (e.g., anorectal manometry and/or defecography and/or colonic transit time) should be taken into account. Pelvic floor rehabilitation and subsequently anorectal surgery or sacral nerve stimulation should be considered on the basis of the results of the “second level” exams. Colectomy represents the “last resort” and should be suggested only for patients with “inertia coli” only after performing also colonic and gastrojejunal manometry. FOBT: Fecal occult blood test.
- Citation: Bellini M, Gambaccini D, Usai-Satta P, De Bortoli N, Bertani L, Marchi S, Stasi C. Irritable bowel syndrome and chronic constipation: Fact and fiction. World J Gastroenterol 2015; 21(40): 11362-11370
- URL: https://www.wjgnet.com/1007-9327/full/v21/i40/11362.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i40.11362