Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Feb 14, 2014; 20(6): 1602-1607
Published online Feb 14, 2014. doi: 10.3748/wjg.v20.i6.1602
Published online Feb 14, 2014. doi: 10.3748/wjg.v20.i6.1602
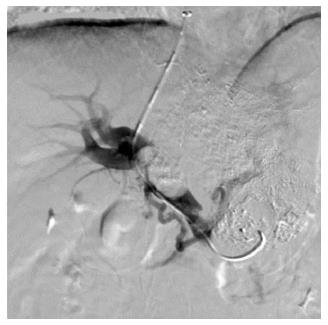
Figure 1 Portal venogram in a 59-year-old man with hepatocellular carcinoma and lung metastasis, who was treated with transjugular intrahepatic portosystemic shunt for severe varicosis and vomiting blood for 3 d.
Puncture was successfully performed in the right branch with tumor thrombus in the trunk and left branch of the portal vein.
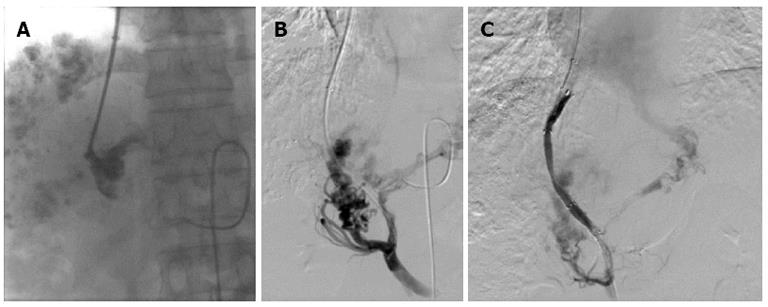
Figure 2 Portal venograms in a 41-year-old man with hepatocellular carcinoma and lymphatic metastasis, who was treated with transjugular intrahepatic portosystemic shunt for severe varicosis and vomiting blood for 5 d.
A: Injection of a small amount of contrast agent demonstrated tubular and slow blood flow with no dissipation and the portal vein was clearly defined; B: After a catheter was introduced, the portal vein image was confirmed by 30° right anterior oblique angiography; C: After two Fluency stent grafts with a length of 80 mm and diameter of 8 mm were implanted, the shunt was shown to have smooth blood flow by postoperative angiography.
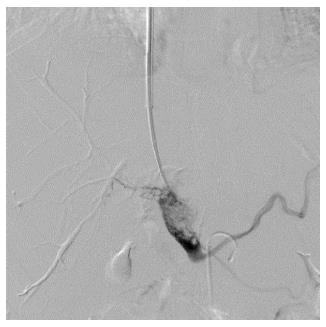
Figure 3 Portal venogram in a 37-year-old man with hepatocellular carcinoma and lung metastasis, who was treated with transjugular intrahepatic portosystemic shunt for severe varicosis and vomiting blood for 5 d.
The tumor thrombus was located in the trunk and both left and right branches of the portal vein, and needle puncture was performed in the portal bifurcation. After injection of contrast agent, tumor thrombus was seen as an expansive growth with loose texture, with clear imaging of the portal vein branches.
- Citation: Zhao JB, Feng C, Zhu QH, He XF, Li YH, Chen Y. Transjugular intrahepatic portosystemic shunt with covered stents for hepatocellular carcinoma with portal vein tumor thrombosis. World J Gastroenterol 2014; 20(6): 1602-1607
- URL: https://www.wjgnet.com/1007-9327/full/v20/i6/1602.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i6.1602