Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Nov 14, 2014; 20(42): 15916-15919
Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15916
Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15916
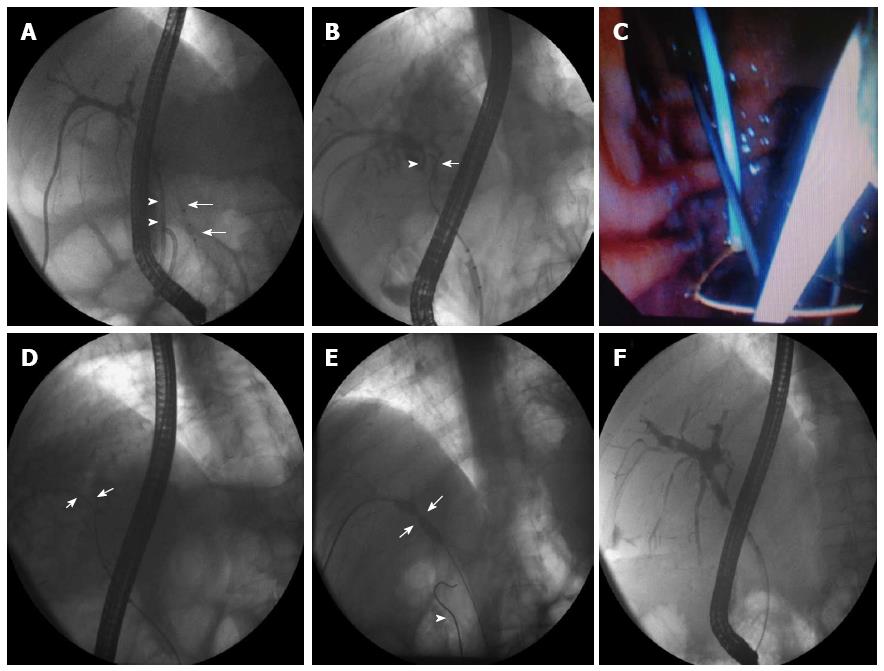
Figure 1 Fifty-three-year-old-man was admitted to our clinic for removal of a percutaneous internal-external biliary drainage catheter and insertion of stents via endoscopic retrograde cholangiopancreatography.
A: Internal portion of the percutaneous transhepatic biliary drainage (PTBD) catheter (arrowheads) and the balloon catheter extending from the papilla towards the common bile duct (CBD) (arrows) were observed separately on cholangiography; B: Despite several attempts at simultaneous percutaneous transhepatic cholangiography, all attempts at advancing a guidewire (arrow) proximally through the papilla into the intrahepatic bile ducts failed and the guidewire (arrowhead) could not be advanced into the CBD; C: The guidewire which was inserted transpapillarily was intentionally pushed through the paracholedocal area at the level of the CBD stricture and spontaneously came out of the duodenal bulb. A snare was slowly introduced via the transhepatic route into the bulbus and the guidewire was caught by closing the snare under endoscopic visualization; D: The guidewire was pulled proximally all the way through the percutaneous access (arrows); E: This was followed by a 5 and 7 mm balloon dilatation of the stricture (arrows). Another guidewire, which was inserted into the duodenal bulb at the site of the PTBD’s internal orifice, is also shown in this figure (arrowhead); F: In the third month of follow-up, the stricture was almost completely resolved, and the patient was then followed stent-free.
- Citation: Odemis B, Oztas E, Yurdakul M, Torun S, Suna N, Kayacetin E. Interesting rendezvous location in a liver transplantation patient with anastomosis stricture. World J Gastroenterol 2014; 20(42): 15916-15919
- URL: https://www.wjgnet.com/1007-9327/full/v20/i42/15916.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i42.15916