Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. Oct 7, 2014; 20(37): 13453-13465
Published online Oct 7, 2014. doi: 10.3748/wjg.v20.i37.13453
Published online Oct 7, 2014. doi: 10.3748/wjg.v20.i37.13453
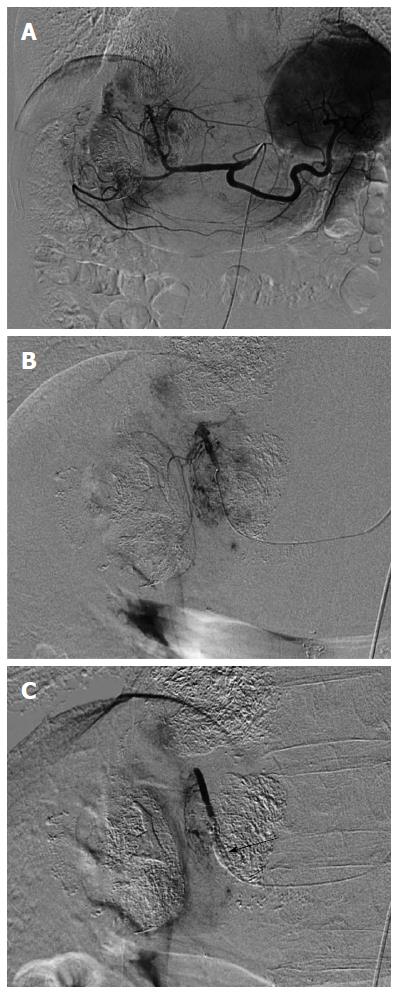
Figure 1 Selective arteriography with and without balloon-occluded feeding artery in a 72 year-old man with multiple hepatocellular carcinomas.
A: Celiac arteriography revealed multiple hepatocellular carcinomas (HCCs) in the liver; B: Opacified HCCs were shown by medial segmental arteriography without balloon-occluded feeding artery; C: In contrast, the arteriography with balloon occlusion showed faint opacification of HCCs and nontumoral liver parenchyma was opacified. Arrow indicated an inflated microballoon.
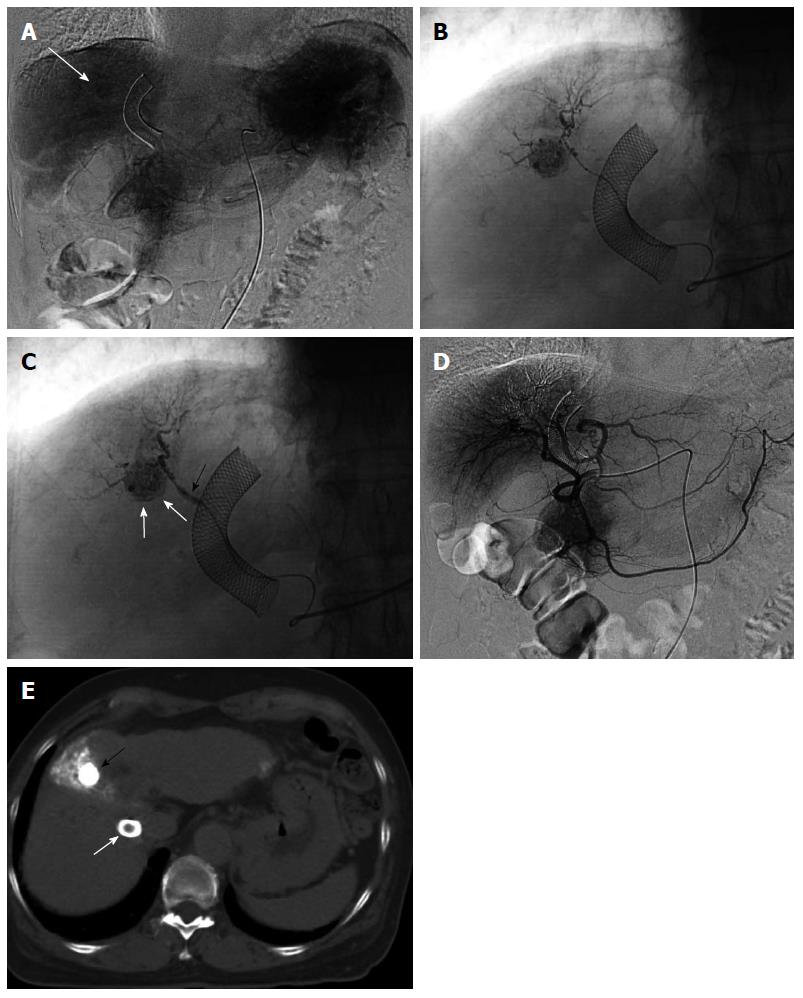
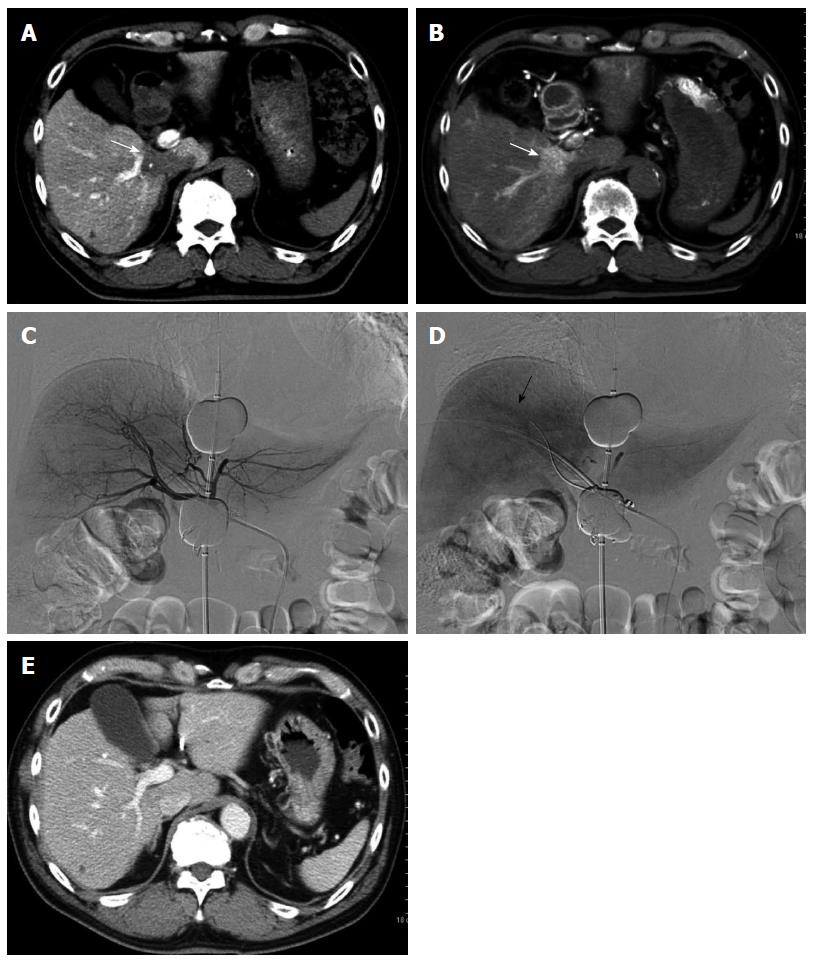
Figure 2 Two-step balloon-occluded transarterial chemoembolization.
A 76-year old woman characterized as Child-Pugh class C underwent transjugular intrahepatic portosystemic shunt (TIPS) for massive ascites before several transarterial chemoembolization (TACE) sessions. Celiac arteriography in the venous phase (A) showed a small hepatocellular carcinoma (HCC) (arrow). A microballoon catheter was advanced into the tumor feeding artery. Then, two-step balloon-TACE (B-TACE) was performed. First, tumors were sufficiently embolized by TACE without balloon occlusion of the tumor feeding artery (B); Second, a microballoon catheter was inflated to occlude the feeding artery (C, black arrow), and B-TACE was performed to fully embolize the peritumoral liver parenchyma (C, white arrows). Common hepatic arteriography showed no proximal migration or leakage of embolization materials (D). Following the two-step B-TACE procedure, computed tomography showed dense lipiodol accumulation in the HCC (E, black arrow). There was no evidence of proximal migration or leakage of embolization materials. White arrows indicated a stent for TIPS.
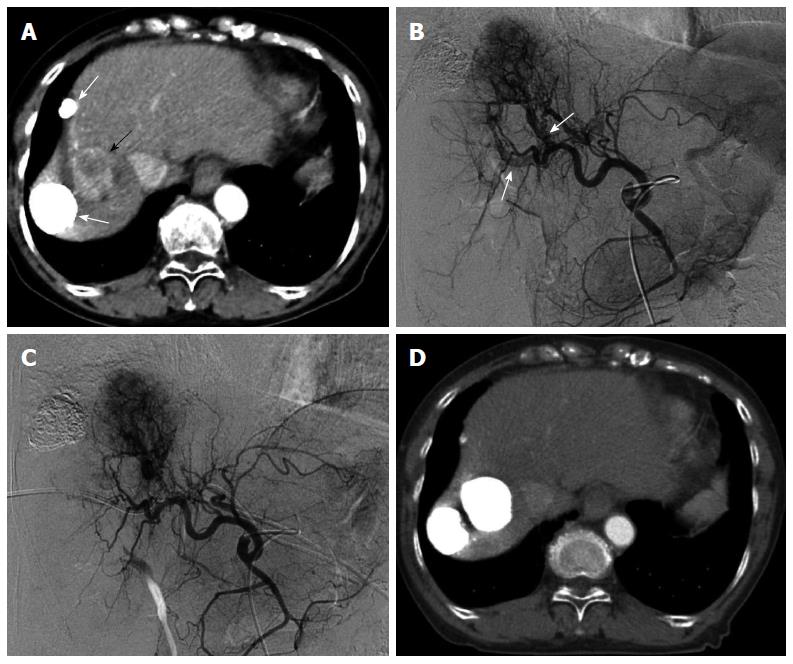
Figure 3 Multiple hepatocellular carcinomas with significant arterioportal shunts in a 71-year-old woman.
Enhanced computed tomography (CT) imaging revealed viable hepatocellular carcinomas (HCCs) (A, black arrow) with lipiodol deposit HCCs (A, white arrows). Common hepatic arteriography in the arterial phase (B) demonstrated HCC with significant arterioportal shunts (B, arrows), consisting of P8 and P4. Common hepatic arteriography under balloon occlusion of the portal vein branches of P8 and P4 showed an opacified tumor with non-visualized arterioportal shunts (C). CT images 2 mo after transcatheter arterial chemoembolization under occlusion of the 2 portal vein branches (D) demonstrated a dense lipiodol deposit in the HCC and a complete response, according to modified Response Evaluation Criteria in Solid Tumors.
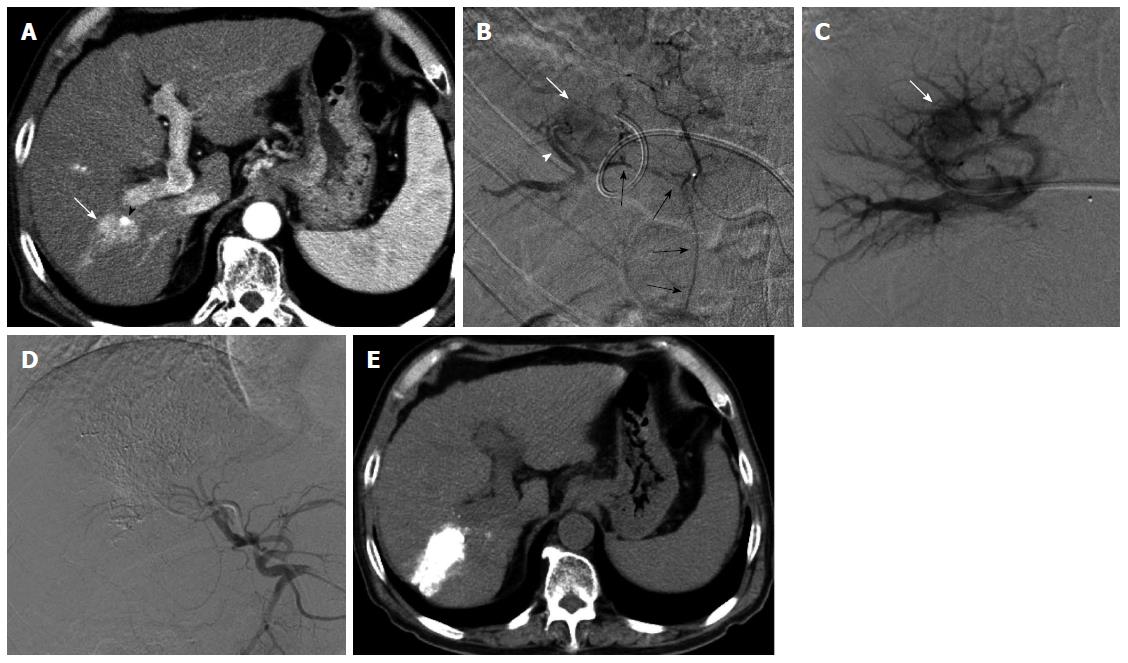
Figure 4 Transportal chemoembolization for hepatocellular carcinoma with an arterioportal shunt in a 70-year-old man.
Enhanced abdominal computed tomography (CT) examination (A) demonstrated a recurrent hepatocellular carcinoma (HCC) (A, arrow) in the posterior segment with a lipiodol deposit (arrowhead). Hepatic arteriography via the anterior branch (B) revealed a HCC (B, white arrow) fed by the cystic artery (B, black arrows) and an intratumoral arterioportal shunt (B, arrowhead). A 5-French sheath was inserted into the portal vein via the lateral superior branch of the left portal vein. Direct portography via the portal vein branch contributed an arterioportal shunt showed a tumor stain (C, arrow). Following transcatheter portal chemoembolization, proper hepatic arteriography showed non-visualized tumor stain and arterioportal shunt (D). Non-enhanced CT 7 d after therapy (E) showed a dense accumulation of lipiodol in the tumor and peritumoral liver parenchyma.
Figure 5 Retrograde-outflow percutaneous isolated hepatic perfusion for multiple hepatocellular carcinomas in a 64-year-old man.
A patients received 2 sessions of transcatheter arterial chemoembolization for multiple hepatocellular carcinomas (HCCs) at other hospital. Computed tomography (CT) during arterial portography (A) and hepatic arteriography (B) demonstrated multiple HCCs with portal vein invasion (arrows). Retrograde-outflow percutaneous isolated hepatic perfusion (C, arterial phase; D, venous phase) was performed twice (arrow of D indicated a portal branch), and enhanced CT imaging 6 mo after therapy (E) revealed that the HCC was diminished.
- Citation: Murata S, Mine T, Sugihara F, Yasui D, Yamaguchi H, Ueda T, Onozawa S, Kumita SI. Interventional treatment for unresectable hepatocellular carcinoma. World J Gastroenterol 2014; 20(37): 13453-13465
- URL: https://www.wjgnet.com/1007-9327/full/v20/i37/13453.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i37.13453