Copyright
©2014 Baishideng Publishing Group Co.
World J Gastroenterol. Jan 21, 2014; 20(3): 613-629
Published online Jan 21, 2014. doi: 10.3748/wjg.v20.i3.613
Published online Jan 21, 2014. doi: 10.3748/wjg.v20.i3.613
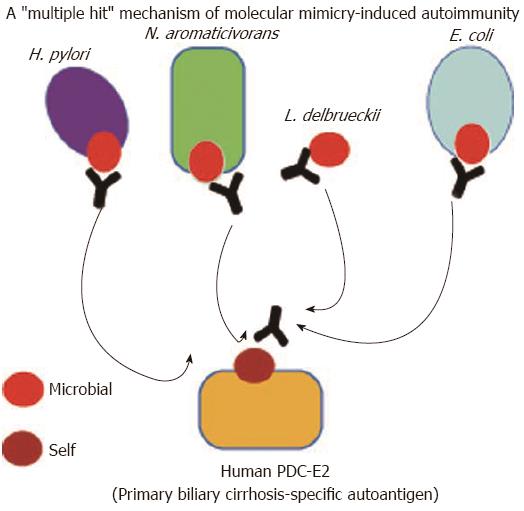
Figure 1 A “multiple hit” molecular mimicry mechanism involving microbial mimics originated from Helicobacter pylori and other microbes linked with primary biliary cirrhosis.
The major autoepitope of primary biliary cirrhosis-specific anti-mitochondrial antibodies (PDC-E2, pyruvate dehydrogenase complex) shares amino acid similarities with 4 microbial mimics from Helicobacter pylori (H. pylori)[142], N. aromaticivorans[154], L. delbrueckii[155,156], and E. coli[140,157,158]. The working hypothesis is that exposure of susceptible individuals to infections caused by these microbial agents will initiate humoral and cellular immune responses against microbial epitopes (in our case, these will be those sharing similarity with the self-epitope). Antibodies or T-cells against the microbial mimics may then cross-react with the human autoepitope initiating an autoreactive immune response which could lead to the induction of cellular damage and the perpetuation of autoimmunity (and can cause autoimmune disease). Experimental data so far provided demonstrate the existence of cross-reactive responses between self and microbial peptides from E. coli, N. amoraticivorans, and L. delbrueckii. However, experimental testing has shown that the H. pylori mimic (from urease beta) is not a target of cross-reactive responses specifically present in primary biliary cirrhosis[159]. The prevailing notion is that the mimic from H. pylori does not share amino acid similarity to an extent that could initiate cross-reactive response. On the contrary, the other microbial mimics have sufficient homologies with the human autoepitope and can promote molecular mimicry-based immune responses against self.
-
Citation: Smyk DS, Koutsoumpas AL, Mytilinaiou MG, Rigopoulou EI, Sakkas LI, Bogdanos DP.
Helicobacter pylori and autoimmune disease: Cause or bystander. World J Gastroenterol 2014; 20(3): 613-629 - URL: https://www.wjgnet.com/1007-9327/full/v20/i3/613.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i3.613