Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. May 21, 2014; 20(19): 5918-5923
Published online May 21, 2014. doi: 10.3748/wjg.v20.i19.5918
Published online May 21, 2014. doi: 10.3748/wjg.v20.i19.5918
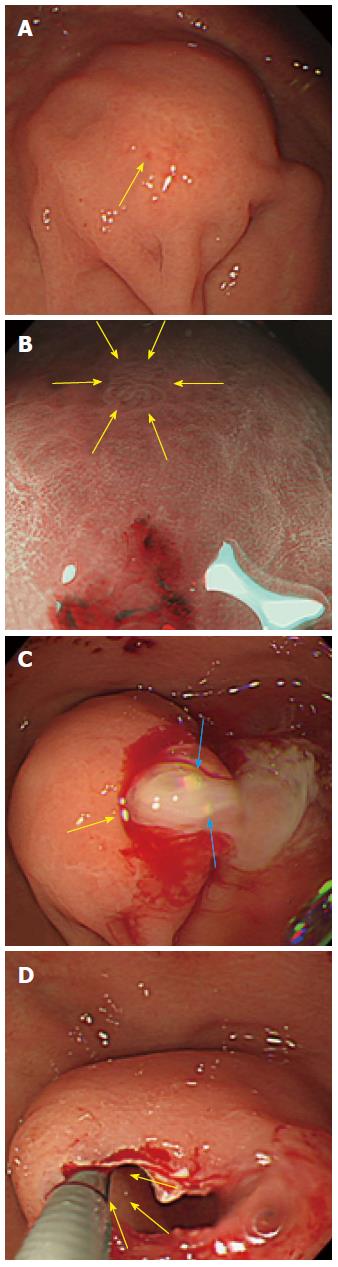
Figure 1 Esophagogastroduodenoscopy showed a submucosal tumor.
A: The esophagogastroduodenoscopy (EGD) showed a gastric submucosal tumor (SMT) measuring 30 mm in diameter in the greater curvature of upper body with bridging folds and a tiny reddish spot on top (yellow arrow); B: Using NBI-ME, the tiny area was observed to be dilated with banded marginal crypt epithelium (yellow arrows); C: Milky white mucous and calcification structures (blue arrow) were exuding from the biopsy site (yellow arrow); D: The solid portion inside the wall of the SMT with small cystic changes were exposed using forceps (yellow arrow).
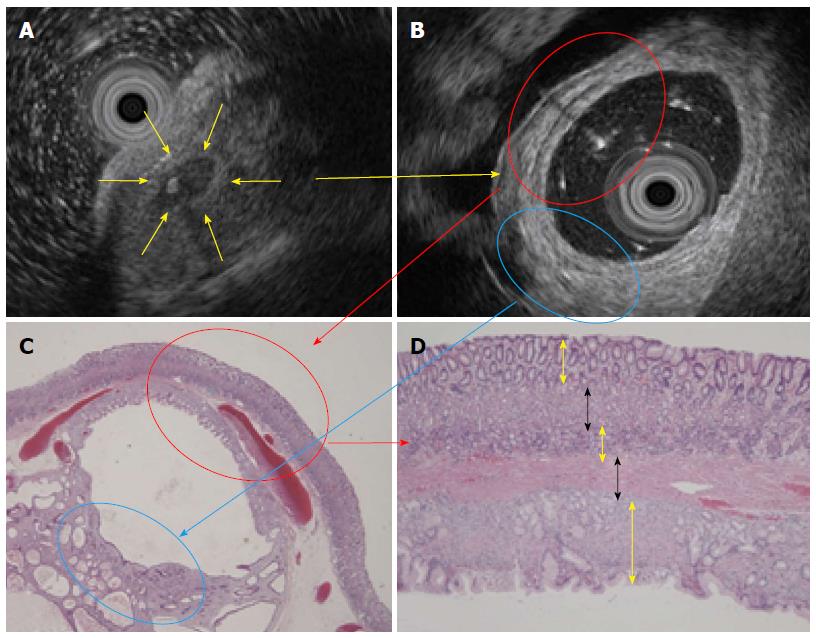
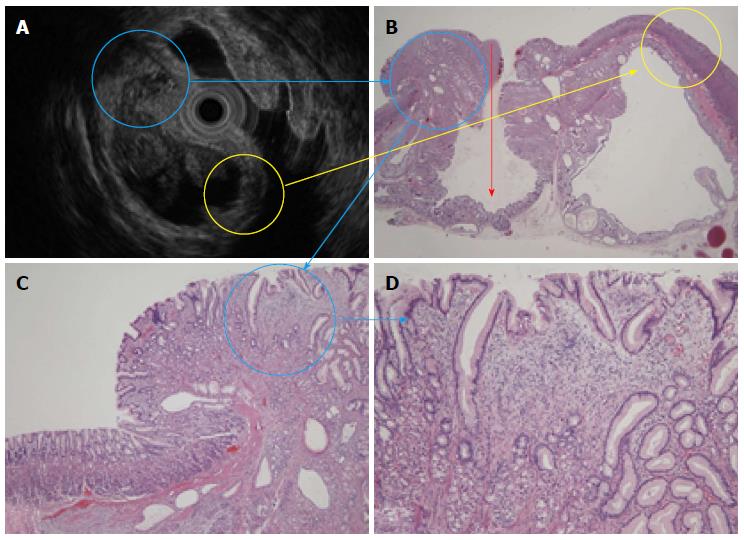
Figure 2 Endoscopic ultrasound before and after the biopsy and histology.
A: An EUS before biopsy revealed a heterogeneous tumor with a cystic area and calcification spot (yellow arrow); B: An endoscopic ultrasound (EUS) from inside the submucosal tumor (SMT) filled with distilled water and an inserted EUS probe showed 5 specific layers (red circle); C: An HE stain (× 20) also showed the 5 structural layers. The hyperechoic portion showed proliferation of pseudo-pylorus glands and cystic gland dilatation without cytological atypia (blue circle); D: The 5 layers consisted of a normal mucosal layer (yellow arrow), immature fibroblasts (black arrow), pyloric glands (yellow arrow), muscularis mucosa (black arrow) and another normal mucosal layer (yellow arrow) (HE stain × 100).
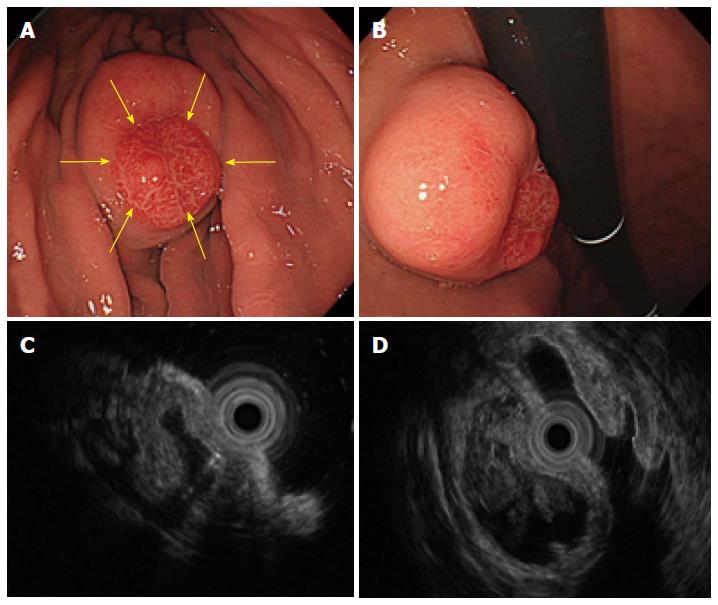
Figure 3 An submucosal tumor measuring 40 mm in diameter was found in the greater curvature of the middle body.
A and B: The size of the submucosal tumor (SMT) had increased from the 20 mm in diameter that was reported 5 years before. In addition, a reddish erosive part 10 mm in diameter was found on the top of the SMT (yellow arrows). C and D: An endoscopic ultrasound revealed a heterogeneous tumor with small spotty cystic areas, a large anechoic cystic part, with papillary structures and 5 specific structural layers as its wall.
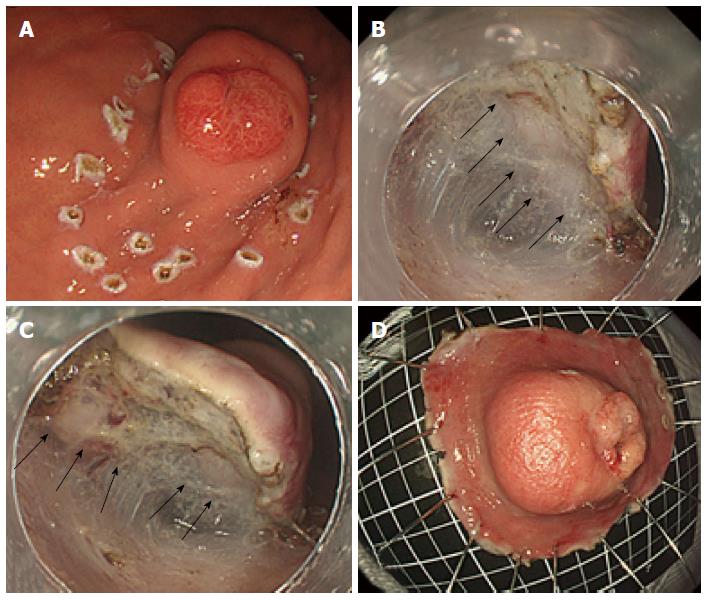
Figure 4 Endoscopic submucosal dissection to resect the submucosal tumor.
A: An en bloc resection using endoscopic submucosal dissection (ESD) was performed to obtain an accurate diagnosis; B and C: Similar to Case 1, milky white components were observed during the ESD (black arrows); D: The lesion was completely resected with a sufficient safety margin.
Figure 5 An endoscopic ultrasound and histological comparison.
A: An endoscopic ultrasound (EUS) revealed a heterogeneous tumor; B: The 5 layers shown in the EUS and HE stain (× 20) (yellow circle) consisted of a normal mucosa layer, immature fibroblast cells, pyloric glands, muscularis mucosa, and another normal mucosa layer. The surface mucosa was inverted into the submucosal layer (red arrow); C and D: The hyperechoic solid portion had tiny low echoic cystic spots (blue circle) and showed the proliferation of pseudo-pylorus glands, cystic glands, fibroblast cells, smooth muscle, and nerve elements.
- Citation: Mori H, Kobara H, Tsushimi T, Fujihara S, Nishiyama N, Matsunaga T, Ayaki M, Yachida T, Masaki T. Two rare gastric hamartomatous inverted polyp cases suggest the pathogenesis of growth. World J Gastroenterol 2014; 20(19): 5918-5923
- URL: https://www.wjgnet.com/1007-9327/full/v20/i19/5918.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i19.5918